Featured Reports
Tuesday March 13th 2018
Patient experience, public satisfaction and politics
Many of our featured reports cover patient experience. This week's is different.
Instead of looking at experience of NHS services, this briefing, using data from the British Social Attitudes survey, looks at general public satisfaction with the NHS. As the authors state, "Polling on public attitudes is different, because people tend to focus on wider issues as well as their experience of care when responding. Not everyone responding to a public poll will have used the NHS recently".
So how satisfied are the general public with our health service? The good news is that "the NHS remains a treasured national institution that is a key part of the British national identity. The public is unwavering in its support for the underlying principles of the NHS and consistently prioritises the health service for extra government funding".
The bad news is that "public dissatisfaction with the NHS grew to 29% in 2017" the highest level of dissatisfaction with the NHS since 2007". Further, "Dissatisfaction with the NHS has risen rapidly over the past three years: between 2014" and 2017, the level of dissatisfaction almost doubled".
Analysis of responses to the survey shows that people under the age of 65 report lower levels of satisfaction than those aged 65 and older. And respondents who identify as Black report lower levels of satisfaction than respondents who identify as White. The briefing notes that "Patient experience surveys also find that patients from minority ethnic groups report more negative experiences, and this may be a contributing factor to differences in the satisfaction levels reported in the BSA survey".
The top two reasons for satisfaction were "quality of care" and "free at the point of use". The top two reasons for dissatisfaction were "not enough staff" and "takes too long to get an appointment". There is an interesting mix here of opinions that may stem from patient experience but which could also reflect political viewpoints.
The question of political viewpoints is important. The conclusion to the briefing states that "With an increase over the last few years in the proportion of survey respondents reporting lack of funding as a reason for their dissatisfaction, it seems the public is increasingly aware of the reality of funding pressures that the NHS has experienced". It finishes by saying that "With equally small increases in funding planned over the next few years and NHS performance on key headline measures worsening, it is hard to see the public's satisfaction with the NHS improving in the near future".
Tuesday April 23rd 2024
Ways of knowing
"Permanent medical devices are implanted for a wide range of indications across many medical specialties" says this study. It concentrates on one in particular - the vaginal mesh implant used to treat stress urinary incontinence.
Developed in the 1990's and initially seen as the gold standard, the device was before long subject to "a cascade of governmental reviews and regulatory warnings" arising from reports of pain, haemorrhage, infection and more.
The study aimed to explore and understand women's experience of living with complications attributed to vaginal mesh surgery. It found key themes including:
- Loss of dignity. Participants described the humiliation of urine leakage that was the context for surgery, but which could also become a barrier to discussions about post-surgical complications.
- Loss of self. Pain and exhaustion, along with loss of jobs and social lives led some women to feel robbed of present and future selves.
- Dehumanisation. Participants described the need to be treated as a human being, not as body part. Some described being "butchered" by surgeons.
- Trust. Some women felt 'lied to', 'conned' or 'tricked' into surgery. Some were angry that vaginal mesh had been 'sold to them' as 'gold standard', saying that risks had been underplayed.
- Infallibility. This theme describes encountering an infallible and inflexible medical way of knowing. Participants felt that the medical community 'denied' that symptoms were caused by mesh. Some felt treated as if they were 'neurotic', or 'hysterical'.
The issue of "ways of knowing" is crucial. Women described how they sought their own ways of knowing, as well as a sense of solidarity, in online communities. They were sustained by the collective marginality of those existing together in a 'wilderness'. In community, they found their way out of the wilderness and no longer felt alone or 'mad'.
The authors find that women, overall, are asking to be treated as "an embodied whole". Clinicians need to understand that their scientific knowledge (medicine) and craft knowledge (surgical practice) should be tempered with "wisdom" - knowledge that is forged through experience and relationships, and is concerned with moral life and human dignity.
They state that "epistemic injustice - whereby a person’s contribution to the production of knowledge is unrecognised or unjustly excluded... is an ethical issue for careful consideration in healthcare". And "Differentiating anatomy, or indeed pathology, from the experience of a condition may help us to understand the areas of miscommunication that led to widespread mesh use".
This, they say, "has important implications for clinical education in the future".
Tuesday April 16th 2024
Co-opting feminism
"Increased awareness and advocacy in women’s health are vital to overcome sex inequalities in healthcare" says this paper from Australia. But, it says, "Feminist narratives of increasing women’s autonomy and empowerment regarding their healthcare... are now increasingly adopted by commercial entities to market new interventions (technologies, tests, treatments) that lack robust evidence or ignore the evidence that is available".
One example is the AMH hormone test, used in fertility treatment. Levels of AMH in the blood are associated with the number of eggs in a woman’s ovaries. High levels indicate the presence of more eggs and, in theory, higher fertility potential.
But the authors warn that "the notion that AMH testing can enable women to make informed reproductive decisions rests on the incorrect assumption that the test reliably predicts fertility. The evidence now consistently shows that the AMH test cannot reliably predict likelihood of pregnancy, time to pregnancy, or specific age of menopause for individuals".
In spite of this, "persuasive feminist rhetoric is being used on upmarket websites to conceal or gloss over the test’s limitations, as well as the commercial incentives behind the test’s promotion". One website, for example, tells women "You’re not ovary-acting. Understand your hormones and fertility, be the boss of your symptoms and get the expert care you deserve - every step of the way".
A second example relates to breast density - a risk factor for breast cancer. The paper states that "Consumer advocacy groups, often sponsored by large companies... argue that all women must be informed of their breast density to enhance their knowledge and health".
Concerns about population-wide notification, however, include the relatively non-modifiable nature of breast density and the lack of evidence that clinical pathways for women with dense breasts are beneficial. Breast density notification can "increase women’s anxiety, confusion, and intentions to seek supplemental screening", while supplemental screening itself can "include high rates of false positive results", perhaps because of "The unreliability of breast density measurement, which varies across time and by assessor".
Here, the authors point to messaging "evoking fear, guilt, or placing blame on women (eg, 'If you haven’t had a mammogram, you need more than your breasts examined').
The authors argue that "Women’s health is vital and cannot be allowed to be hijacked by vested interests". On the other hand, "persuasive messaging that uses the guise of feminist health advocacy can be difficult to criticise, as legitimate critique may be misconstrued as misogynistic or paternalistic".
They say that "Health consumers and clinicians need to be wary of the simplistic narratives that any information and knowledge is always power". And, they say, "Communication between women and their clinicians is a key aspect to addressing this".
Tuesday April 9th 2024
The data gold rush
"Direct-to-consumer virtual care" is the focus of this Canadian study. It looks at "patient-initiated virtual care delivered by for-profit companies via proprietary software platforms". These services, it says, "allow patients to obtain rapid and convenient access to virtual care without having a prior relationship with the clinician".
It notes that "Patients appear to value direct-to-consumer virtual care services", although it then warns that "much of the research has been commissioned by companies in the industry". Benefits can include better access, convenience, cost savings and positive health outcomes. But some studies have indicated risks including overdiagnosis and overtreatment.
The key question for this paper, though, is the virtual care industry’s data handling practices. That question was explored through interviews with industry insiders and by examining industry websites.
A key finding was that "patient data were highly valued by the virtual care industry and used to generate revenues". While this could help companies to improve and expand services, it could also mean adjusting patient care pathways to promote pharmaceutical products. One study participant described a "gold rush" to gain access to data.
These data handling practices were seen as both normal and acceptable. One participant explained that "these companies are doing what every other company that collects personal information does - using the data to make money".
At the same time, study participants were aware of ethical issues.
One example was that "targeted advertising... could interfere in the patient care journey, with implications for patient health". One participant said "I would like my care journey to be governed by what’s the best care for me, not who paid the most amount of money to get in front of me".
Another concern was privacy. There were "confusing and vague privacy policies [and] difficulty opting out of data uses". De-identification was not necessarily a safeguard: the process was described as "subjective" and some providers were said to be "pretty flexible with it". Furthermore, "if companies combine and share datasets, the extra information also increases the risk of reidentification".
The authors conclude that "Patients, healthcare providers and policy-makers should be aware that the direct-to-consumer virtual care industry appears to view patient data as a revenue stream, which has implications for patient privacy, autonomy and quality of care". And, they say, "Policy-makers should consider how other models of virtual care, as well as enhanced privacy legislation and regulation, can address these concerns".
Wednesday April 3rd 2024
Transparency now
Numerous NHS strategies talk about the importance of being 'patient-centred'. Healthcare staff are often brilliant at this, and platforms such as Care Opinion are full of appreciative feedback from patients who have felt listened to and cared for.
Why, then, do healthcare institutions so often get it wrong? What causes the shift from careful and attentive listening by individual staff to careless and dismissive responses at the organisational level?
Our contributors to the spring edition of our quarterly magazine have both tried to raise serious concerns with NHS bodies and have both run into organisational brick walls.
In 1978, Liza Morton was the youngest baby in the world to be fitted with a cardiac pacemaker. She recently asked to see her paediatric medical records - partly to make sense of her childhood experiences, and partly because the records could hold important information for her ongoing cardiac care. But the records have been destroyed. No-one had thought to tell her, and no-one seems to want to take responsibility.
Kath Sansom has spent years campaigning for women harmed by pelvic mesh. She recently replied to a government consultation on industry payments to healthcare providers - an issue on which mesh campaigners have long been calling for greater transparency. The government has taken four months to respond and has failed to answer any of the points she raised.
We stand by Liza and Kath in their fight for information and for justice. And we condemn healthcare bodies whose reluctance to engage with patients is an affront not just to patients but also to the many, many healthcare staff who work day in and day out for a patient-centred NHS.
Tuesday March 26th 2024
Parity a long way off
"The issue of unsafe discharge from hospital is nothing new" says the Parliamentary and Health Service Ombudsman in the opener to this report. In 2016, "my predecessor had seen patients not being assessed or consulted properly before discharge, carers not being informed and people being kept in hospital due to poor coordination across services".
In mental health services, this can present a risk to a great many people. In 2020 to 2021, there were more than 270,000 attendances at A&E departments in England where a person was recorded as having a primary diagnosis of a psychiatric condition.
During 2021 to 2022 more than 50,000 people were detained under the Mental Health Act, and more than 97,000 people in England were admitted into NHS-funded mental health, learning disability or autism inpatient care.
So how much improvement has the ombudsman seen in the years since 2016? According to this report, not enough. Failings in discharge procedures persist, and "The most common failing... is the involvement of patients, their families and carers in decision-making".
The report presents a series of case studies set out under headings that reveal the problems experienced by patients. These include incorrect information on self-help support, families not updated on the day of discharge, poor record-keeping, poor communication, poor joint working between professionals, and failure to carry out a Mental Capacity Act assessment.
The report makes a number of detailed recommendations, but an overarching concern is that "when these mistakes happen, the health service must be open and honest in its response, acknowledge the impact it has had, and commit to learning".
That ought to go without saying, and it is worrying to see the ombudsman feeling that he has to spell it out.
Equally worrying is the fact that we are now seven years on from Prime Minister Theresa May's call for true parity for mental and physical health. And yet the ombudsman's conclusion is that "reaching the point where mental health is given equal priority to physical health in terms of access and outcomes of care still remains a long way off".
Tuesday March 19th 2024
The death of Patient A
In February 2007 a patient (Patient A) died in the operating theatre of the Salford Royal Hospital. This report states its purpose as "to examine what led to the death of Patient A, and what action the Trust took or did not take following their death".
It reveals a litany of poor professional practice, combined with abuse of power, centred on a spinal consultant, Doctor F. Concerns around this doctor's practice included:
- Negligent and fraudulent clinical practice, leading to serious life-threatening harm to patients.
- Poor clinical practice, including not treating patients in a dignified manner during physical examinations.
- Bullying, intimidation and harassment of colleagues, including unsolicited sexual contact with female staff.
- An extramarital affair between Doctor F and a senior divisional managing director of the Trust, which allowed poor clinical practices and behaviours to continue through undue protection of Doctor F.
The report details harms to other patients of Doctor F. These included a paused operation, with failure to proceed with the next phase for 90 minutes, and no communication with senior colleagues. There were poor preoperative documentation and consent processes. One spinal procedure involved multiple misplaced screws and a life-threatening haemorrhage due to direct vessel damage.
The report's author says that the patients and/or their families should receive a full and transparent explanation and an apology for the level of care they received from Doctor F and the Trust. And, he says, "Lessons need to be learnt from these unfortunate events".
These are depressingly weak recommendations. We know what the lessons are because arrogance, dysfunctional cultures and reluctance to concede error have already been detailed in multiple inquiry reports: Mid Staffs, Morecambe Bay, Gosport, Cwm Taf, Shrewsbury & Telford, East Kent and more. The lessons are clear. It is time we started acting on them.
Tuesday March 12th 2024
The elephant in the room
Patient experience during the Covid crisis was bad. Thousands of people died in isolation from family and friends. Lockdown exacerbated loneliness, anxiety and mental ill-health. Even the arrival of vaccines was, for some people, a cause of fear rather than hope.
Patient experience through the climate crisis will be worse. But while the NHS can claim to have been taken by surprise by Covid, it cannot make the same claim for global heating.
This report from the World Economic Forum explains how scientists have spent at least the last twenty years warning of the impacts of climate change - including those on human health.
Some impacts are well-known - floods droughts, wildfires and rising sea levels. Others, such as the probable arrival in Europe of diseases like malaria, dengue and Zika may not yet have permeated the public consciousness.
Equally, the uneven consequences across population groups may be poorly understood. The report makes the point that "climate change will exacerbate global health inequities. The most vulnerable populations, including women, youth, elderly, lower-income groups and hard-to-reach communities, will be the most affected".
We have seen with Covid how a massive disruption to human health also causes huge disruption to healthcare systems. The report says that climate change will likewise create "a significant additional burden on already strained infrastructures".
The report offers both scenarios and solutions, and issues a clear call to action. "Unlike the case with COVID-19, which took governments and the global healthcare industry by surprise, a unique window exists to adapt and prepare healthcare infrastructures, workforces and supply chains for the escalating impact of the climate crisis".
Importantly, the task is not restricted to healthcare professionals and policymakers: "Collaborative efforts involving multiple stakeholders and industries are essential".
In today's NHS the talk is primarily about waiting lists, workforce and increasingly, productivity. Few, if any, are thinking seriously about the far bigger elephant in the room. But both patients and professionals need to ready themselves.
Tuesday March 5th 2024
Online records access here to stay
In 2021, NHS England announced plans that patients aged 16 and over would have prospective access to their primary care records online, by default. By November 2023, one in four general practice surgeries across England still did not offer online record access (ORA).
Why the delay? Part of the answer, according to this paper, is that "Although patients often welcome transparency, studies show many doctors... express scepticism about patient access".
So this study set out to explore the experiences and opinions of English GPs about the potential impact of ORA on both patients and doctors.
There were plenty of negatives. The vast majority (91%) of those surveyed "somewhat agreed" or "agreed" that after obtaining full online access, a majority of patients would "worry more". 85% believed that most patients would "find their GP health records more confusing than helpful". And 95% "somewhat agreed" or "agreed" that after full online access, a majority of patients would "contact me or my practice with questions about their health record".
Against this were some positives. 70% "somewhat agreed" or "agreed" that a majority of patients would "better remember the plan for their care", with 61% believing patients would "feel more in control of their healthcare". Around half (52%) "somewhat agreed" or "agreed" that a majority of patients would "better understand their health and medical conditions" after accessing their online records or "be more likely to take their medications as prescribed" (50%).
Interestingly, 60% "somewhat agreed" or "agreed" that a majority of patients would "find significant errors in their GP record".
For themselves, GPs concerns included that "I will be/already am less candid in my documentation" (72%); that "patients who read their GP record will be/already have been offended" (58%); and that patient online access would "increase my risk of having legal action taken against me" (62%).
The authors state that "we cannot help but observe a trend towards contrastive views between clinicians and patients". And they say that their findings "suggest patients in England may be vulnerable to negative stereotyping with regard to their capacity to understand and emotionally cope with reading their own health information".
A key implication is the importance of supporting GPs and their staff to become better prepared for talking about and writing documentation that patients will now read. The paper concludes that "in England, patients’ online access to their GPs’ records is here to stay. In the coming months, it will be crucial for GPs, primary care staff and patients to adapt to this radical change in practice".
Tuesday February 27th 2024
Constraining co-creation?
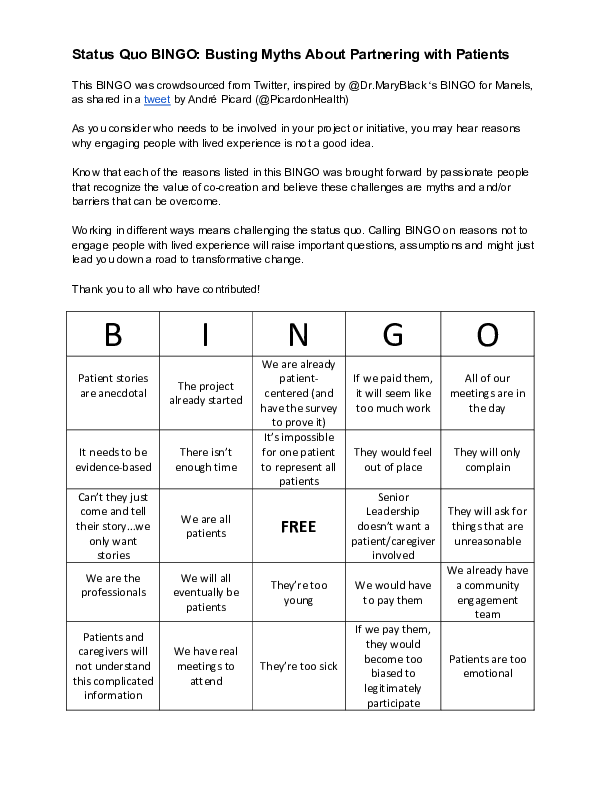
"The last decade has seen an explosion of interest in co-production and co-creation" says this paper. But, it says, "the extent to which these new forms have resulted in meaningful change...is not fully clear".
To explore the issue further, the researchers looked at five local Healthwatch organisations in different parts of England. Local Healthwatch was established to "strengthen the collective voice of local people" and has been described as "a source of genuine co-production".
"The institutional context for co-creation", according to the authors, was "promising". Healthwatch had support at the policy level, and from state agencies, and it drew legitimacy from its status as the "official" conduit for public voice. Additionally, "The ability of Healthwatch to bring the views of marginalized and ‘seldom-heard’ groups to the table formed an important part of their appeal".
The result was that "stakeholders across the whole system had a shared interest in demonstrating that co-creation was happening in a visible, tangible way". So far so good. But here the research team sounds a warming: "this performative need had a strong influence on the activities pursued by the five Healthwatch".
The study found that Healthwatch "took care in how they positioned their organizations... conscious of the need to demonstrate activity and impact". Crucially, "co-creation depended on trusting relationships... which in turn required that they be taken seriously as part of the system rather than be seen as outsiders". From this, they took a view on "which issues were worth pursuing and which were out of bounds".
The approach "seemed to pave the way for constructive dialogue between Healthwatch and others, and secure influence on at least some decisions". "However", say the authors, "this disposition also meant that some activities were shunned". And "Healthwatch maintained a cautious distance from other voices of the public that challenged system organization in a more fundamental way".
Ultimately, "Healthwatch deliberately constrained the scope of their contributions according to their perceptions of acceptability. The full richness of insights, ideas and critique from the breadth of the public that co-creation may offer was carefully filtered before it even reached discussion and decision-making forums: ‘feasible’ solutions took precedence over ‘innovative’ ones".
The paper concludes that "Even though they were not explicitly ruled out-of-bounds, Healthwatch officers knew that to be considered legitimate and serious players in the governance of health and social care, they needed to be selective about which issues they brought to the table". Consequently, "the forms taken by co-creation in practice were largely conservative and constrained".
Tuesday February 20th 2024
A turning point for transparency?
This report is marked "Private and Confidential". It is not hard to see why.
It sets out the findings of an independent review of services at the University Hospitals Sussex Trust, and includes patient safety issues as well as concerns about culture and behaviour.
In spite of that, the report has been posted on the Trust's website, as one of the papers to be discussed at a recent (8th February) Board meeting in public.
That seems like a bold move. The report contains some very worrying findings, including the following:
- A high volume of complaints from patients, and delays in responding.
- Consultant surgeons being dismissive and disrespectful towards other members of staff and displaying hierarchical behaviours towards allied healthcare professionals, particularly junior members of staff.
- Reports of two trainees being physically assaulted by a consultant surgeon in theatre during surgery.
- A culture of fear amongst staff when it came to the executive leadership team, with instances of confrontational meetings where consultant surgeons were told to 'sit down, shut up and listen'.
In the past, and in other Trusts, reviews of this kind have tended to be suppressed. For example, the 2015 Morecambe Bay investigation revealed "the reluctance of the Trust to share the report [of the 2009 Fielding review into the Trust’s maternity services] even when being pressed for it".
It is all the more surprising, therefore, to see the UH Sussex Trust receiving the review team's report in January 2024, then immediately putting it into public Board papers in the first week in February.
In a preamble to the report, the Trust's Chief Executive says "There are some tough messages for staff and us as Trust leaders [but] Problems can’t be solved without first being openly acknowledged".
Everybody knows that things go wrong in healthcare. Far too often, the response is avoidance and denial. This response seems different. Might it be a turning point for transparency? We must, surely, hope so.
Monday February 12th 2024
Groundhog Day strikes again
This review was commissioned in response to a BBC Panorama programme that showed "appalling levels of abuse, humiliation and bullying of patients at the Edenfield Centre in Prestwich". The report says that "The horror of what was shown could not fail to touch anyone who watched the programme".
By the same token, anyone who has read other reports of abusive cultures (Winterbourne View, Whorlton Hall, Muckamore Abbey) cannot fail to get a sense of history repeating itself. All the familiar patterns are there.
We hear that "Some patients and families described not being believed when they raised concerns or complained about the care received... Others shared how they did not always feel safe to disclose concerns, with many accounts of feeling intimidated, undermined, ignored, or fearful that ‘bad news’ was not welcomed".
Another Groundhog Day moment describes "a Trust that was not sufficiently focused on understanding the experience of patients, families and carers... The lack of both curiosity and focus on improvement led to missed opportunities for organisational learning".
In common with health professionals elsewhere, staff at Edenfield talked of "feeling exasperated, tired of not being listened to and disconnected from the Trust leadership... staff have felt fearful to speak up for many years".
Of course some patients and families tried to raise concerns. But "there was a lack of clarity and accountability throughout all the complaints process... making a complaint was discouraged".
The new Chief Executive at the Trust has said 'We cannot change the past, but we are committed to a much-improved future".
It is true that we cannot change the past. But we can learn from the past. From Mid Staffordshire, Morecambe Bay, Gosport, Shrewsbury & Telford, and East Kent. From Cwm Taf in Wales and the hyponatraemia deaths in Northern Ireland. From the widespread harms caused by Primodos, Sodium Valproate and pelvic mesh. From Letby, Paterson and Fuller.
The literature on harm - and harmful cultures - is extensive. It contains all the lessons we need. Healthcare providers need to stop trotting out wearyingly familiar apologies, and start taking seriously the job of learning from patient experience.
Monday February 5th 2024
Misinformed choice
"Informed choice" is a principle enshrined in the NHS Constitution - a document based on medical ethics and law. Informed choice means that patients should have sufficient information and understanding before making decisions about their medical care.
It is surprising, then, to see NHS England announcing a potentially misleading addition to the NHS App. Heralded as a "new feature to improve patient experience", the app will now show mean (average) waiting times for treatments at English acute Trusts.
Official figures published via the NHS England website, however, do not use averages. They use a "92nd percentile" figure. Why? Because under the NHS Constitution, 92% of people waiting are meant to be treated within 18 weeks. And the 92 percentile figure is always higher - much higher - than the average.
NHS England says that the average waiting times information will help "by better informing patients about their care". But unsurprisingly, some disagree.
Patient Safety Learning cites "senior figures close to the project" as saying that "the NHS App will give patients 'disingenuous' and 'misleading' information about how long they can expect to wait for care".
The President of the British Orthopaedic Association agrees. He has said that "as an example, the mean average waiting times for patients could be around 22 weeks whereas the 92nd percentile figure is 63 weeks, showing just how far apart these two metrics are". He goes on to say that "It is unacceptable that patients may be given such false hope".
So there seems to be a double standard at work. Official statistics - aimed at policymakers and practitioners, use the helpful and reliable 92nd percentile figure. But the NHS App, aimed at patients, offers averages that could be misleading.
We think that informed choice is important. So we have taken the more meaningful official figures and made them available via our open access waiting list tracker.
The tracker gives instant access to waiting times for all treatment types at all acute Trusts across England. It enables side-by-side comparisons of waiting times at different Trusts. And it includes a headlines summary that can be printed off as a handy aide-memoire. We think all of that might be more useful to patients than a simple figure on average waits.
By putting averages into the NHS App, NHS England risks undermining the NHS Constitution's promise of informed choice. It also risks undermining public confidence and trust. And that is not something that a struggling NHS can afford to do.
You can use our waiting list tracker here.
Tuesday January 30th 2024
Pharma's levers of power
"The pharmaceutical industry is one of the most powerful industries in the nation" says this US study. The industry has various levers of power, but this report looks at one in particular: "the billions in grants the industry has given out to the most powerful advocacy organizations in the country".
The study was conducted by Public Citizen, which describes itself as "a nonprofit consumer advocacy organization". Its aim is "to ensure that government works for the people - not big corporations".
The authors analysed hundreds of publicly available documents and built a dataset including corporate and foundation grants given out by the Pharmaceutical Research and Manufacturers of America (PhRMA) and its member companies.
They discovered $6 billion in total grants dispersed by the PhRMA Network to more than 20,000 different recipients from 2010 through 2022. 13 of the nation’s largest and most powerful patient advocacy organisations received $266 million between them.
The view of the authors is that "when a patient advocacy organization stays silent on a debate on drug prices, publishes an op-ed supportive of a PhRMA Network position, or endorses a questionable drug, it is reasonable to wonder if the money they received... played any role in their decision making".
This spirit of curiosity led to findings including the following:
- The American Cancer Society received $6 million from AstraZeneca, $4.7 million from Merck, and $3.4 million from Pfizer, all manufacturers of expensive cancer drugs.
- The American Diabetes Association received more than $11 million in grants from Sanofi and more than $7 million from Eli Lilly. Along with Novo Nordisk, the companies control 90% of the insulin market globally.
- One of the nation’s most prominent spinal muscular atrophy organisations, Cure SMA, received more than $5.8 million from Novartis, the manufacturer of the SMA gene therapy that costs $2.25 million per dose.
Additionally, Public Citizen found many op-eds that were published by PhRMA Network grant recipients criticising US government efforts to rein in drug prices. In some cases, the author and grant recipient received a grant around the time of the op-ed’s publication for 'advocacy".
Furthermore, 740 lobbyists were hired by both grant recipients and members of the PhRMA Network. These grant recipients received $577 million from the PhRMA Network.
In conclusion, the authors state that "The PhRMA Network companies are not mission-driven charities. They are some of the largest and most profitable companies in the world, hyper-focused on returning value to shareholders. It’s impossible to know how much the money affects the decision-making process of the grant recipients. But it is hard to believe $6 billion had no effect".
Tuesday January 23rd 2024
Building trust
"The NHS is looking to advances in digital health technologies and data to help tackle current pressures and meet rising demand" says this report from the Health Foundation. "But", it says, "ensuring new uses of technology and data have the backing of the public is critical if they are to become business as usual".
The authors surveyed 7,000 members of the public to test their views.
The good news is that people are generally supportive of technology in healthcare. Over half of those surveyed (51%) said that the NHS should make more use of self-monitoring devices, such as blood pressure or heart rate monitors. And nearly half (48%) said the NHS should be making more use of electronic health records.
There was less support, however, for the use of chatbots to check symptoms or get health advice and less support for video conferencing to speak to a health professional. The authors note the difference between technologies aimed at supporting the public, and those that might be perceived to come between the clinician and patient.
As far as healthcare data is concerned, the survey found that nearly two-thirds (61%) knew ‘very little’ or ‘nothing at all’ about how the NHS is using the health care data it collects.
In spite of this, two-thirds said they trust GP practices, local NHS hospitals and clinics and national NHS organisations with their health data ‘a lot’ or ‘moderately’. But national and local government organisations and health technology companies are less trusted. There is, says the report, a need to "grow trust in organisations with currently low trust levels".
The authors conclude that "Over the coming years, policymakers and NHS leaders will need to prioritise meaningful public engagement on the future of technology in health care". And they say that "it is important that this public engagement is inclusive, seeking out the voices of those who can often be excluded in public consultations".
Tuesday January 16th 2024
Detecting patterns of harm
David Fuller worked for the NHS for 31 years. "His employment", says this inquiry report, "started only two years after he committed the brutal murders of two young women in Kent, whose deceased bodies he sexually assaulted". He went on to commit 140 known offences against deceased women and girls in the mortuaries at Maidstone and Tunbridge Wells NHS Trust.
How can such appalling crimes have gone undetected for so long? The report offers a series of answers - and as with so many instances of large-scale avoidable harm, they fit a recognisable pattern.
The first is that "This is not solely the story of a rogue electrical maintenance supervisor. David Fuller’s victims and their relatives were repeatedly let down by those at all levels whose job it was to protect and care for them".
That statement has echoes in the Cumberlege review of harms from products including pelvic mesh. It said "The issue here is not one of a single or a few rogue medical practitioners... It is system-wide".
The Fuller report notes that "The culture... at Tunbridge Wells Hospital, as observed by the Inquiry, was not one of questioning and curiosity. There was a lack of curiosity about David Fuller’s work behaviour in relation to the mortuary".
That parallels the inquiry into Ian Paterson, the jailed breast surgeon: "While we heard from nurses that 'everyone knew', some professionals told us that they were unaware that Paterson was performing inappropriate treatment until formal investigations were underway. There is, therefore, a question regarding professional curiosity".
There is evidence of siloed working at Maidstone and Tunbridge: "mortuary staff felt ignored by senior managers and separated from the rest of the Trust... mortuary staff were 'functionally isolated'.
Something similar happened at East Kent, the scene of harms in maternity services, where "Canterbury was full of the great and the good consultant-wise, and they sort of looked down at Margate and Ashford and everybody knew that as well".
At Maidstone and Tunbridge there was "a culture... in the mortuary where Standard Operating Procedures were routinely ignored and security breaches were not thoroughly investigated".
That takes us back to Paterson, where "The appraisal processes for Paterson did not pick up his poor practice...There were policies and guidance in place, but these were not implemented".
The report of the Fuller Inquiry offers other examples of harmful cultures at Maidstone and Tunbridge, and they all fit with patterns that are - or should be - well known by now across the NHS.
We need to learn from these patterns. That means rejecting simplistic notions of "rogue operators" and instead taking on the harder work of tackling system-level weaknesses. It means understanding that lack of professional curiosity creates opportunities for wrongdoing. It means acknowledging that siloed practice is dangerous practice. It means knowing that when policies are ignored, harm ensues.
The patterns are clear, and every single inquiry report - Mid Staffs, Morecambe Bay, Shrewsbury and Telford, East Kent, Paterson, Letby, Fuller - makes them clearer. An NHS that keeps promising to learn the lessons needs to start learning what patterns of harm look like.
Tuesday January 9th 2024
Telling stories
'Storytelling' is often seen as an important way to communicate patient experience, and rightly so. But how can storytelling be done well?
In this edition of our quarterly magazine, Sue Robins makes the case for safe spaces for patient storytellers (page 3). In her own experience as a speaker, she has encountered tokenism, a lack of care and sometimes, a lack of common courtesy.
At other times, she has found practical and emotional support, and a genuine recognition that her 'stories' are something more than mere edutainment.
Lynn Laidlaw on page 4 recounts the experience of being part of a research team seeking the stories of people who are clinically vulnerable to Covid. As a clinically vulnerable person herself, this opened up questions of identity and competence.
Could she objectively analyse stories that reflected - or diverged from - her own experiences? And how could she occupy the role of 'expert by experience' and 'researcher' simultaneously? Questions like these are vital to good quality coproduction in research.
A special feature on our evidence mapping work (pages 5 and 6) reveals the patchy way in which people’s healthcare stories are brought into the patient experience evidence base. While medical research has clear prioritisation processes, evidence-gathering on patient experience is, essentially, a free-for-all. We show how inequalities in health are linked to inequalities in research, and suggest some solutions.
As always, we also bring you the latest and best patient experience research, packaged in handy summaries for busy people.
Tuesday December 19th 2023
An opportunity lost
The NHS has no shortage of strategies. Many of them - Transforming Community Services, the Five-Year Forward View, the Long-Term Plan - have made the point that the UK has an ageing population, and a growth in long-term conditions. The strategic response depends in large part on encouraging people to "self-manage" their conditions in their own homes and communities.
Central to self-management are homecare medicines services. These provide up to half a million people with the medicines they need, along with any necessary help to administer them.
This House of Lords report examined these services and found a great deal of room for improvement.
A key concern was safety. "No one", says the report, "not the Government, not NHS England, not patient groups, not regulators - knows how often, nor how seriously patients suffer harm from service failures in homecare".
Another was financial. "The Government does not know how much money is spent on homecare medicines services. It is therefore impossible to make any assessment on value for money. Given that the figure is most likely several billion pounds per year, this lack of awareness is shocking and entirely unacceptable".
The report points to "serious problems with the way services are provided. Some patients are experiencing delays, receiving the wrong medicine, or not being taught how to administer their medicine".
Homecare medicines services are mainly provided by private companies. So in some cases, the taxpayer is effectively paying for the service twice - once for the private provider to deliver it, and again for the NHS to pick up the pieces where private providers fail.
"Most concerningly", say the peers, "we found a complete lack of ownership of these key services... no one person or organisation was willing to take responsibility for driving improvements or exploiting the full potential of homecare medicines services to bring care closer to home. Simply put, no one has a grip on this".
The report makes recommendations on transparency, procurement, enforcement of standards and digital infrastructure. It concludes, with a masterpiece of understatement, by hoping that the analysis will "be of assistance" to NHS England and the Department of Health and Social Care.
Tuesday December 12th 2023
Unequal waiting
After the first wave of the Covid-19 pandemic, NHS England asked integrated care boards (ICBs) and NHS trusts to address health inequalities as part of tackling growing waiting lists for elective care. This report looks at three Trusts and ICBs to see what progress has been made.
A fundamental first step was for providers to disaggregate their waiting list data, to identify patients by ethnicity and deprivation. Two years on from NHS England's ask, only one of the three Trusts had achieved this. None of the ICBs were reporting disaggregated waiting times data to their board.
There were also barriers to the idea of a new approach. In one Trust, "work to reprioritise waiting lists had stalled because of resistance from clinicians". In the other two, "leaders were concerned about how clinicians would react to the work".
Data issues were another problem. These included poor quality ethnicity coding, and limited analytical capability.
Surprisingly, there appear to be no formal performance management or accountability structures for inclusive recovery within NHS Trusts or at ICB level: "health inequalities were not part of accountability conversations with NHS England". Moreover, "Interviewees were uncertain about what a meaningful measure of success would be, and noted that the policy on taking an inclusive approach to reducing the backlog did not set out a clear vision for this".
In spite of all this, there were some pockets of success. But these were more in terms of simple improvement projects than systemic change. And they were led not so much by executive teams as by individuals with a passion for addressing inequalities. The report makes the point that "the NHS needs to harness that enthusiasm and give these leaders the tools and ideas needed to make change in their clinical areas".
The authors conclude that "Waiting lists are one place where the causes, experiences and consequences of health inequalities coalesce. If the NHS is serious about addressing health inequalities, it needs to address inequalities on waiting lists for elective care as part of that".
Tuesday November 28th 2023
Journaling experience
In patient experience work, it is common to hear talk of people who are "hard to reach".
Sometimes the phrase is seen as a convenient excuse for not trying hard enough. But some people really are hard to reach because of severe illness, or mental incapacity.
In this article, David (an intensive care patient), tells how the practice of diary-keeping enabled family members and staff to understand what he was experiencing as he emerged from six weeks of coma, ventilation and proximity to death.
As he recovered, David found himself disorientated and prone to vivid nightmares and hallucinations. At times he was overwhelmed by anxiety and paranoia. Through all of this, his partner Rose's diary, along with his own scrawled questions and notes, helped them both to make sense of their fear and bewilderment.
Rose also documented clinical updates, making her own record of procedures, treatments and clinical signs, along with notes on David's reactions and progress.
The resulting booklet, says David, "helped me to appreciate the outstanding care both I and my family had received in those weeks". It also enabled him to "create some sort of timeline and extract the true memories from my fragmented and delusional recall".
Since leaving hospital, the diary remains a valuable resource, helping David to live with the continuing consequences of his illness. "The power in these entries lies in their ability to help me understand how dire my prognosis was. When I get frustrated with my life situation and residual health issues, finding myself struggling to move forward, I can look back to these early days and see how far I have travelled in my recovery journey."
David comments that "Reading and reflecting on my diary has often grounded me, helped ease my anxiety and prevented me from slipping further into the grip of depression, proving in my case, the ongoing mental health benefits of the diary".
David finishes with a request for health professionals: "In a world where intensive care is provided at huge expense, an ‘ICU diary’ costs a small amount of time, the price of paper and a pen and a moderate amount of teamwork. I hope I have demonstrated that the cost to benefit ratio for your patient is undoubtedly in its favour".
Tuesday November 21st 2023
A struggle every day
"A struggle every day' is how one respondent to a Healthwatch survey on hygiene poverty described her experience of homelessness.
That short phrase no doubt encompasses a multitude of other experiences. Healthcare policymakers and providers need to hear those experiences if they are to improve services for homeless people, in line with NHS England guidance.
This begs a question: where is the evidence on the healthcare experiences of people who are homeless or insecurely housed?
Is it easily accessible, or scattered across multiple websites and hidden behind journal paywalls? Is it comprehensive, or are there gaps? Is new research being steered towards the accumulation of new knowledge, or is there duplication and waste?
To begin answering these questions, we looked through two and a half years’ worth of studies and reports. We found extensive duplication - particularly on the question of homeless people’s access to health services. And we found areas such as hygiene poverty where the evidence was, to say the least, thin.
This latest report in our evidence mapping series looks at the implications for national NHS bodies and for research funders, and suggests ways to get better value and better learning. And if you want to explore the evidence base for yourself, you can skip straight to our interactive map to see what it looks like.
Tuesday November 14th 2023
Slaying dragons
Patient safety seems to be a permanent feature of news headlines these days.
Large scale harm in maternity services has been revealed at Shrewsbury and Telford, and at East Kent. There is an ongoing investigation at Nottingham. There have been deaths of babies at the hands of Lucy Letby. And then there are individual examples, such as the avoidable death from sepsis of Martha Mills.
So what is going wrong with patient safety? How can there be so many calamitous outcomes across so many services and locations?
This commentary from America offers food for thought.
The author argues that in patient safety work, the emphasis should be on "slaying dragons" - eliminating or at least mitigating risks to patients. Instead, he says, "current practice focuses almost exclusively on investigating dragons - tracking reports on the number and type of dragons that appear, how many villagers they eat and where, whether they live in caves or forests, and so on".
Healthcare workers, he says, "invest untold time and effort in incident reporting, incident investigation (eg root cause analysis and its various subcomponents), and the occasional prospective risk assessment". But "We cannot investigate a dragon to death. No more can we risk assess our way to safer care".
He is equally critical of "the ritualistic invocation of plan-do-study-act (PDSA) cycles" on the basis that "the successful use of PDSA in healthcare is vanishingly rare".
Three remedies are offered. The first is structured risk control tools, specifically designed for patient safety improvement.
Secondly, "we need to expand the ranks of dragon slayers. Clinicians cannot go it alone - and should not have to".
Thirdly, the task of slaying dragons means "moving beyond analysis and grappling with the messy work of systems change".
"The patient safety movement", says the author, is "settled into the comfort of an obsolete standard of practice". There is a complacency in which "ongoing patient harm has been treated as 'inevitable' and 'the cost of doing business' despite studies showing that it is possible to do better".
Tuesday November 7th 2023
A better experience for patients
'We need to provide a genuinely better experience for patients.' So says NHS England’s delivery plan for recovering urgent and emergency care services, published in January 2023.
It says that urgent and emergency care will 'embed what works for patients', that services will 'reflect the needs of different groups of people', and that there will be 'proactive steps to tackle known inequalities, particularly for groups who are disproportionate users of UEC services'.
These are good ambitions. But they raise important questions.
How can we know what works for patients? Do we actually understand the needs of different groups of people? And while tackling 'known inequalities' must be a good thing, are there unknown inequalities that we might be missing?
The NHS prides itself on being evidence-based, so to find the answers to these questions, we need to draw on evidence of patient experience in urgent and emergency care. But what does the evidence base look like? Is it robust and comprehensive, or are there gaps needing to be filled?
This latest report in our evidence mapping series describes our attempt to find out. We examine the evidence base to see who is doing the research, who they are talking to, and what topics they are covering.
We make suggestions for how research funders and national NHS bodies could steer the research to get better value and better learning. And if you want to explore the evidence base for yourself, you can skip straight to our interactive map to see what it looks like.
Tuesday October 31st 2023
Storytelling as the foundation of learning
"As with most education, storytelling is often the foundation of learning", says Naomi Shiner, the author of this paper.
Shiner's story is that of a parent navigating the NHS with a child with Down Syndrome. Her educational goal is to "enlighten healthcare professionals about life with Down syndrome".
Her first experience was the 18-week routine scan, at which the very much non-routine appearance of a second sonographer signalled a concern. Shiner quickly found herself ushered to "a beige, empty room, with nothing to do but wait for people to arrive and receive more information".
The next step was an MRI scan of the baby's head, which revealed a shortened corpus callosum. What, wondered the parents, might that mean for her future? There seemed to be no clear answers. If no-one could answer my questions, wonders Shiner, why had they bothered with the MRI?
A rollercoaster of mixed experiences followed. After the birth, one staff member loudly announced that baby Nina might have Down Syndrome. "The sudden silence that fell across the ward", says Shiner, "was deafening".
After a check for possible heart defects, "a neonatal consultant entered our side room holding rolled up leaflets in his left hand. With no words spoken, at that point I already knew we had an issue".
Throughout her early motherhood experience (which included at one point, being suspected of harming her baby) Shiner detected "a noticeable difference in terms of compassion, information giving, time at appointments for discussion and importantly the opportunity to be involved in decision making".
One staff member, the dietitian, "provided the gold standard experience, even being there during emergency admissions and communicating our needs across hospital trusts".
Shiner concludes that "For Nina and I, there is no one solitary experience, each appointment and interaction whether positive or negative bleeds into the next. These engagements at times, can be emotionally and cognitively exhausting for us both".
She asks healthcare professionals to learn more about the modern lives of individuals with Down syndrome, and reminds them that parents have "the determination to fight for our children...please do not make us".
Tuesday October 24th 2023
Who gets heard on Covid?
"Every story matters", says the Covid Inquiry. It goes on to say that "The pandemic affected every single person in the UK", and that "Every one of our experiences is unique".
Personal experiences are, indeed, unique. But sometimes large numbers of people can have similar experiences - of lockdown, say, or anxieties about vaccines, or of being banned from visiting a relative in a care home.
From common experiences, we can learn lessons. Those can help to improve policy and practice - both now, and in preparing for the next pandemic.
In early 2020, the Patient Experience Library started collecting and cataloguing published research on people's experiences of Covid-19. Now, as we head towards three years from the declaration of the first UK lockdown, we find ourselves in possession of a unique archive.
We have combed through the evidence base to try to understand whose experiences were recorded, and which aspects of life under Covid have been documented.
We found a research landscape in which some topics have been covered extensively while others remain virtually untouched. Equally, some communities come through loud and clear while others are almost voiceless.
We look at the implications for national NHS bodies and for research funders, and suggest ways to get better value and better learning. And if you want to explore the evidence base for yourself, you can skip straight to our interactive map to see what it looks like.
Tuesday October 17th 2023
Child protection
This report shows that child and adolescent health is not, for the most part, a matter for hospitals. Their wellbeing relates much more closely to "the environment and social circumstances in which children grow up".
The facts are stark:
- Obesity affects 23% of Year 6 children in 2021/22 in England. 80% of obese young people remain obese as adults.
- In 2022, 29% of five year olds in England had tooth decay.
- Vaccination coverage has decreased in 13 out of 14 of the routine childhood vaccination programmes. The UK lost its WHO measles free status in 2018.
- 86% of UK cities exceed recommended limits for airborne particulate matter. The effects of air pollution have a greater impact on children and young people.
- Rates of poor mental health for children and young people are rising. Suicide is the leading cause of death in children and young people.
It can be hard for children to make their voices heard: conventional NHS mechanisms such as Friends and Family Test or national surveys tend to be hospital-based and can often be unavailable to, or inappropriate for, under 18s.
Reports like this are therefore important in their advocacy for this very large and very vulnerable proportion of the population.
The report makes a series of recommendations - on food regulation, dentistry, vaccinations, air quality and more. And it makes the point that "prevention is better than cure, but we must also recognise that prevention in childhood is better than prevention in adulthood".
Tuesday October 10th 2023
Mostly about the people
Digital healthcare is not just about clever technology. It is also about people and as with other aspects of healthcare, it needs to be patient-centred.
The 2016 Wachter Review, "Making IT Work" put it this way; "digitising effectively is not simply about the technology, it is mostly about the people". Its first recommendation was "Carry Out a Thoughtful Long-Term National Engagement Strategy".
That long-term engagement strategy never happened, so research into patient experience of digital healthcare has been piecemeal and sporadic. We wondered if it might be possible to map the evidence base - to find out which parts of the community have been invited to share their views, and to see what specific topics have been explored.
We found extensive duplication: nearly half of the evidence base is about service access and experience. We were left wondering why so many researchers had gone over the same ground so many times.
On healthcare data sharing, we found only 6 reports - less than 3% of the total. That was a surprise, given well-known public anxieties about the confidentiality and online security of their health records.
Equally, artificial intelligence in healthcare has been big news recently. But we found only 3 reports dealing with public experiences and views on health-related AI.
Our report offers further analysis, and an interactive online visualisation enables users to see for themselves what the evidence base looks like.
We hope that both the report and the visualisation will be explored by national bodies - in particular the National Institute for Health Research, NHS England and the Department for Health and Social Care. They could all help to put an end to the free-for-all in research on people's experiences of digital healthcare.
And, seven years after Wachter, they could, perhaps, "Carry Out a Thoughtful Long-Term National Engagement Strategy".
Tuesday October 3rd 2023
Voice matters
The importance of staff and patient voice has been starkly revealed in recent weeks - first by the sentencing of Lucy Letby, and then by Merope Mills’ call for a new Martha’s rule after the avoidable death of her daughter. In both cases, concerns were raised - and ignored.
The incidents remind us that listening to feedback is not some sort of optional extra. Sometimes it is a matter of life and death.
It is also a matter of justice. On page 3 of the latest edition of our quarterly magazine, we hear from Kath Sansom, a campaigner on the harms caused by pelvic mesh. Efforts by Kath and many others has now resulted in a government consultation on disclosure of industry payments to the healthcare sector. We join Kath in urging readers to have their say.
Patient voice is also an important component of 'epistemic justice': the question of what counts as valid evidence in healthcare. All too often, scientific knowledge is given top billing, while lived experience is dismissed as 'anecdotal evidence'.
On page 4 of the magazine, Nicole Thomas describes the genuine difficulties faced by researchers when trying to hear from patients, and how the Patient Experience Library has helped her to overcome some of the barriers.
As always, we also bring you the latest and best patient experience research, packaged in handy summaries for busy people. And we’re always keen to hear from our readers, so if you know of a standout report that we should be featuring, or if you want to submit a comment piece, get in touch!
Tuesday September 26th 2023
Toolkits mountain
Patient and public involvement (PPI) is, these days, a given in healthcare policy and practice. Providers, commissioners, policymakers and researchers all state the importance of hearing from service users about what matters to them.
This "involvement imperative" has given rise to a plethora of guidance notes, checklists, frameworks and toolkits, all purporting to show what good practice in PPI looks like. So we decided to carry out a mapping exercise, to see how much guidance there is, and to see if we could make sense of it all.
It turns out there is a mountain of the stuff. We found 536 toolkits - a vast landscape of well-meaning advice.
In a ten-year period between 2012 and 2022, PPI toolkits were being published at an average of one every two weeks. In the five years between 2016 and 2020, they were coming out at the rate of one a week.
There is extensive duplication. Over 100 toolkits offer general guidance on patient and public involvement. Another 100 or so offer guidance on involvement in research.
At the same time, there are big gaps. We found just 4 toolkits with a specific focus on engagement with Black and minority ethnic groups, 4 for LGBT patients and service users, and 4 for people with physical disabilities. For people with learning disabilities there was just one.
We might not have mapped the entire mountain. (Indeed, since we completed our analysis, a further 22 PPI toolkits have been published.) But we have seen enough of it to know that there is a serious lack of co-ordination and prioritisation.
Our report tells the full story of how we scaled the toolkits mountain, and what we saw from the top. You can also visit an interactive online visualisation, helping users to see for themselves what the toolkits are, and what topics they cover.
We hope that both the report and the visualisation will be explored by national bodies - in particular the National Institute for Health Research, NHS England's Health Inequalities Team and NHSE Library and Knowledge Services. They could, perhaps, help to end inequalities in healthcare by ending the inequalities in the guidance on involvement.
Tuesday September 19th 2023
Patient Experience in England
As the autumn begins, it is time once again to bring you our annual overview of research into people’s experiences in healthcare.
We summarise a swathe of national patient surveys, and then take a themed look at our top picks from wider evidence gathering - both via academic research and from community-based organisations.
In a health and social care system buckling under multiple pressures, it will come as no surprise to find that patients, too, are struggling.
Satisfaction with GP services is down to its lowest level for six years. In Urgent and Emergency care, survey results are worse than in all previous surveys back to 2016. The British Social Attitudes Survey found that overall satisfaction with the NHS is at the lowest level since the survey began in 1983.
On the plus side, there remains widespread public support for the founding principles of the NHS. In the British Social Attitudes Survey, 93% agreed that the NHS should be free of charge when you need it, and 82% said the NHS should primarily be funded through taxes.
Wider research covers topics such as waiting list challenges, patient safety and digital healthcare. But in a sign of the times, we also have a section on engagement and misinformation. Public attitudes these days are shaped as much by 'fake news' as by reliable information sources - and as the research indicates, professional attitudes can also succumb.
Our final section covers financial matters, including the fact that the local Healthwatch network now receives less funding than its predecessor (the Local Involvement Network) did over ten years ago. Healthwatch, in the wake of the Mid Staffordshire disaster, was meant to strengthen patient voice. Financially, however, it has been weakened.
In a healthcare system beset with difficulties, that does not seem like good policy.
Tuesday September 12th 2023
Whispers on the wind
This rapid review is a response to concerns about information to support patient safety in mental health inpatient care. In particular, it sought to understand how data and evidence was collected, and then used to identify and mitigate risks.
The good news is that "There was a consensus that hearing from patients, carers and staff was essential". However, that consensus was frustrated by practical and organisational barriers.
The review found that routes to give feedback were not clear or were difficult or time-consuming to use. Patients, carers and staff felt that their feedback was not listened to or acted on. They also sometimes felt unable to raise concerns for fear of the repercussions to themselves and others.
There were further problems with data quality. The review found that for data to be effective in providing early alerts on patient safety, it had to be available in as close to real time as possible. However, it "often has a time lag of weeks or months before it reaches frontline teams and local leaders".
One particularly worrying finding was that "At all levels, staff could recall almost no feedback from reports from national or regional data sets... that was useful to help them do their jobs".
The review saw good practice as well - for example, where providers had experts by experience on their boards and in their leadership meetings. Some used apps to allow patients, carers and staff the opportunity to give quick, real time feedback, and some had "high quality dashboards that gathered and triangulated data". Alongside all of this were "outstanding examples of action-orientated daily reviews in ward safety huddles".
A key learning point is "the importance of ‘soft’ intelligence - as one leader put it, 'whispers on the wind' - and the need for leaders to act on information from all sources, rather than relying on one dashboard or data set". And beyond that is the fact that "data on its own is not enough - it has to lead to action".
Tuesday September 5th 2023
First, speak no harm
In July 2020, Baroness Cumberlege published First Do No Harm, the review of medicines and medical devices, including pelvic mesh. Three years on, the pain continues.
This Scottish review of case records relating to transvaginal mesh details some of the pain. Women affected by it talk of physical pain, sometimes acute, sometimes chronic, in hips, groin, legs and back. They talk of the mental toll of anxiety and insomnia. And they talk of the emotional anguish of feeling a loss of trust in healthcare professionals, and a loss of their own identities - the sense that they have become a different, and diminished, person.
One section of the report discusses communication and clarity of language. It says that "The importance of communication which is accurate, transparent and understood is the foundation of good clinical care", but then goes on to describe ways in which that foundation was undermined by misleading communication.
The two key mesh devices differ in how they are surgically placed, with variation in procedures and risk. But the differences were not always made clear. Sometimes polypropylene mesh was described as "tape", giving women the impression of something that "didn't sound too bad". They were not informed of the size of the device, and not always told that the device would be permanent. None of the women involved in the Case Record Review had been shown an example of the device.
Many women were told that mesh surgery was a "gold standard" treatment. Why? Because, says the report, "the early information that was given to patients [was] largely informed and written by the industry... [and] was described using only positive language. This was because there appears to be no requirement for the information to be explicit regarding disclosure of potential risks".
The review is clear that a "consequence of a failure to clearly communicate is the impact that this will have on the patient-clinician relationship. Trust may be diminished or eroded altogether". It goes on to say that "we cannot underestimate the lasting impact of the erosion of trust or the patient’s willingness to engage in the future with healthcare".
Wednesday August 30th 2023
Advance care planning: what patients think.
This paper starts with the observation that advance care planning (ACP) helps people with serious illnesses or deteriorating health to think ahead and plan for what might happen. However "uptake remains low internationally". To find out why, the researchers explored public perceptions of ACP.
The study team carried out a rapid scoping review, and grouped their findings into four domains, as follows:
- Knowledge and engagement. Public knowledge of ACP is low. The literature indicates that patients and public have often never heard of ACP, and would not know how to find out about it. Even with good knowledge, engagement with ACP may be poor. The paper states that "Familiarity with ACP concepts did not necessarily translate into active participation in ACP".
- Fear, mistrust and avoidance. Some patients feared they would be ‘tempting fate’ if they became more open to ACP conversations. Many studies described ACP as being too emotional or distressing for patients and families to engage with. Other studies revealed patients' fears that their expressed preferences and wishes would not be carried out irrespective of having a documented ACP.
- Misconceptions and misinformation. Some patients seem to confuse advance care planning with end of life care. And end of life care itself is seen as care in the last days or hours before death. Accordingly, patients can see attempts to discuss ACP as coming too soon.
- Public expectations of healthcare practitioners. Patients can hold an expectation that it is up to healthcare staff to initiate conversations about ACP. This could lead patients not to raise the topic themselves.
The authors note that "Current debates around future directions for ACP... concentrate on professional and policy perspectives". But, they say, "Although ACP research includes patient and public perceptions, more attention needs to be paid to them in future ACP developments".
Tuesday August 22nd 2023
Still waiting for parity of esteem
This report from the House of Commons Public Accounts Committee acknowledges that NHS England (NHSE) has made progress in improving and expanding mental health services. But, it says, this was "from a low base".
Only around one in three people with a mental health need have access to mental health services. Around 1.2 million people are on the waiting list for community mental health services. Rising demand continues to outstrip service provision.
The Committee makes the point that "Many stakeholders have welcomed the introduction of new access targets and waiting times standards". But, it says, "the standards only cover a minority of people who are referred to mental health services and, despite defining further standards more than a year ago, there are still no plans to roll these out".
In the meantime, data for NHS mental health services (described by the report as "vital for managing performance, developing new services and addressing inequalities") lags behind that available for physical health services. Furthermore, "many service providers [are] still not submitting data as required".
The data gap includes patient experience. "Of 29 integrated care boards surveyed by the NAO [National Audit Office], only four said they had all or most of the data they needed to assess patient and user experiences, and none of them felt this in relation to patient outcomes".
The Committee reminds us that "In 2011, the government set out its goal of achieving 'parity of esteem' between mental and physical health services". But it did so "without setting out what achieving it meant in practical terms".
It recalls that in 2019, the Committee highlighted the need for the government to define 'parity of esteem' clearly, including setting out the criteria it will use to measure progress. But, it says, "The government...has still not done so".
Other groups too, according to the report, want to know what parity of esteem actually means. "Many stakeholders told us that a clear definition, objectives and roadmap are important to understand progress towards this end goal". It says that NHSE would also welcome a definition, but "the Department’s current position is not to specify one".
Tuesday August 15th 2023
Unheard voices of staff
It is well known that there are close alignments between staff experience and patient experience in the NHS. So as health services struggle under multiple pressures, the voices of staff, as well as patients, need to be loud and clear.
This report on the latest survey of Freedom to Speak Up Guardians reinforces the point. "Speaking up is a gift", it says. But it warns that "The benefits of Freedom to Speak Up can only be realised if leaders and board members are inquisitive about what is presented to them and are keen to embrace the learning".
Unfortunately, a readiness to listen and learn is not always apparent.
Two thirds (66%) of survey respondents saw "fear of detriment" as having a noticeable or very strong impact as a barrier to workers speaking up. Barriers included professional hierarchies and seniority. Added to this, one third (34%) of respondents thought that "attitudes towards protected characteristics" (such as gender, ethnicity or sexual orientation) could also affect workers' ability to speak up.
A further dampening effect comes from "futility" - the concern that nothing will be done. Here, two-thirds of respondents (67%) saw futility as a 'noticeable' or 'very strong' barrier to workers in their organisation speaking up. Disturbingly, this represents an eight percentage point increase over the previous survey (58% in 2021).
The report notes that the survey findings are in line with the most recent NHS Staff Survey, which identified "a deterioration in the confidence to speak up by healthcare workers". It also, ominously, states that "Many organisations still do not have a Freedom to Speak Up Guardian registered with and trained by the National Guardian’s Office".
The National Guardian's assessment is blunt: "This decline in perceptions concerns me, as it should all leaders, whether they are providers, regulators, or government". And, she says, "I fear that in this atmosphere of huge challenge for the sector, we are not always hearing what matters, and what can help us improve - the voices of our people".
Tuesday August 8th 2023
Broken trust
"There is no shortage of programmes, policies, new initiatives and roles to try to reduce instances of avoidable harm", says this report from the Parliamentary and Health Service Ombudsman. But, it says, "there is a disconnect between the increasing levels of activity... and the level of progress we see on the frontline".
The report states that the statistics on patient harm "remain stark". It refers to the estimated 11,000 avoidable deaths every year in the NHS, and the "thousands more" patients seriously harmed. Behind these numbers are "the stories of individuals and their families and friends, whose lives have been shattered as a result of avoidable harm".
The PHSO recognises that healthcare staff, too, are affected by harmful organisational cultures: "nearly 40% reported they did not feel safe to speak up about anything that concerns them in their organisation. More worrying still, less than half of staff felt confident their organisation would address their concern".
The report makes a number of recommendations, one of which is "creating a system that is coherent and easier to navigate". This is based on the observation that "Political leaders have created a confusing landscape of organisations", including the Healthcare Safety Investigation Branch (HSIB), the Patient Safety Commissioner, PHSO, NHS England, NHS Resolution and "at least a dozen different health and care regulators". There are, says the report, "significant overlaps in functions, which create uncertainty about who is responsible for what".
But the biggest threat to patient safety, according to the PHSO, is "a system at breaking point". The Ombudsman recognises that "the NHS itself can only go so far in improving patient safety". It also needs "concerted and sustained action from Government... getting past politics to put patient safety at the very top of the agenda".
"The NHS cannot wait any longer", says the report, "Nor can the people who use it or work in it".
Tuesday August 1st 2023
Life with Long Covid
The crisis phase of the Covid-19 pandemic might be over. But the long tail persists - not least for the up to 2 million people experiencing Long Covid.
This study, commissioned by NHS England's Insight and Feedback Team, looked at enablers and barriers to care for Long Covid, and examined public attitudes towards the condition.
Lack of awareness is a particular problem. While people are generally aware that Long Covid exists, they are much less clear about what it actually is. Turning to advocacy and support groups may give mixed results: "advocates reported very low or non-existent awareness of Long COVID services, making it difficult for them to signpost people to services".
The pathway to Long Covid services relies on GPs. But, says the report, "patient access to appointments are well-known challenges...this produces a perceived bottleneck however and places GPs in a ‘gatekeeping’ role, which impacts on how equitable and accessible Long COVID services are perceived to be".
One consequence is that people "tended to find the referral process complex and time consuming, particularly in cases where they felt they had to chase or drive progress".
Another consequence is that patents are self-managing their symptoms outside the support structures of the NHS. The report notes that "People had experimented with lifestyle changes... either because they had given up hope of finding a cure, or while they waited for treatments". And while peer support groups and online forums provide an important source of fellowship and learning, the report warns that "misinformation is rife".
People who can get to a Long Covid clinic are positive about the experience. "They described feeling a mixture of gratitude and relief... particularly that their condition had a name and that others were also experiencing similar ongoing symptoms".
The report makes various recommendations - on advice and information, on outreach to vulnerable groups, and on good practice in clinics. It also recommends partnership between the NHS and non-NHS groups, including community organisations and peer support networks.
For a nation learning to "live with Covid", this report is a worthwhile read.
Tuesday July 25th 2023
Women's burden of care
"The COVID-19 pandemic created a crisis of care" says this paper, "with millions of people now more reliant on unpaid caregiving". It goes on to say that "The burden of unpaid care needs continues to disproportionately fall on women, with devastating effects on health, well-being, and labor force participation".
The analysis is from the US, but contains much that will be familiar to UK readers. The authors make the point that "deep-rooted norms result in family caregiving still being widely perceived as so-called women’s work... Accordingly, US women provide 2.2 times more unpaid family caregiving on a time-per-day basis relative to men".
Unpaid care is also becoming more complicated: "More than half of all caregivers perform medical tasks typically done by health care workers [and] are also expected to help navigate complicated health care and social service systems, understand and track complex health information, and serve as surrogate care coordinators, advocates, and decision-makers".
At least some of this is driven by healthcare reforms, which are decentralising care away from inpatient settings toward the home and community. This is "based on the implicit assumption that family caregivers - the majority of whom are women - will provide this increasingly complex care at home without additional support".
The paper states that caregiving can be personally rewarding. But it also notes harmful consequences: depression, anxiety, and social isolation; impaired physical health; decreased preventive and self-care behaviours; greater acute care use; and even increased mortality. At least some of this arises from the fact that "60% of caregivers are juggling unpaid caregiving with paid job responsibilities".
The authors see a pressing need for reforms to policies that largely exclude family caregivers from receiving direct services or financial and other support, limiting them instead to the person directly receiving care. "This", they say, "is detrimental to both patient and caregiver health".
The paper concludes that "The COVID-19 pandemic has spotlighted the critical role of unpaid family caregiving [and] how women disproportionately assume these responsibilities". "Challenging this gendered dimension of family life", it says, "is essential to better supporting caregivers".
Tuesday July 18th 2023
Glaring gaps in mental health
In 2011, the coalition government published "No Health Without Mental Health". Described as a cross-government strategy, it had a central ambition: "establish parity of esteem between services for people with mental and physical health problems".
Twelve years later, this report from the House of Commons Environment, Food and Rural Affairs Committee is clear that, in rural areas at least, "parity of esteem" is still a very long way off.
The starting point is that the picture of rural mental health across England is "complicated and incomplete due to gaps in health data, the suppression of demand by over-centralised services, and the under-reporting of rural deprivation which is inextricably linked to poor mental well-being".
The Committee points out that "access to nature and the countryside is consistently identified as beneficial for people’s mental health". But "the isolation inherent in rural living represents a significant challenge to the mental health of adults, children, and young people living in rural areas".
A key aspect of isolation is that "NHS mental health services are often not fairly accessible for rural communities, with services largely centred in towns and cities creating barriers to access, compounded by the limitations and weaknesses of rural public transport and digital connectivity".
Inadequate services and opportunities for young people is another feature: "Far too much avoidable demand ends up at the door of Child and Adolescent Mental Health Services (CAMHS) in rural areas because of a fundamental lack of social infrastructure and youth services".
The report notes that "The Government’s flagship levelling up agenda includes over-arching reference to the 'rural proofing' of policy". It says that "The fundamental need to provide equitable access to effective services for mental health and well-being must be part of this picture".
The Committee does not suggest that there is a mental health crisis in rural England. But, it says, "there are more than enough glaring gaps, and obvious red flags, to warrant urgent and meaningful action... rather than having to wait for an inevitable crisis to create a political imperative and free the necessary resource".
Tuesday July 11th 2023
Invisible no more
This paper starts with a frank statement: "Covid-19 brought radical shifts in healthcare policies and practice, including the abandonment of families as partners in care".
Can such a statement be justified? Yes, say the authors, who all have experience of informal or unpaid caring. Their home countries of England, Canada and Australia all saw the swift imposition of strict visiting bans during the crisis phase of the pandemic. In England, the practice of blanket bans on visiting in hospital and care homes was subsequently condemned by the House of Lords.
The bans were introduced as part of well-intended infection control measures. But they had unintended consequences, including poorer patient experience and a greater burden on overstretched staff. The burden was not just physical: "Service providers experienced the moral anguish of turning families away and maintaining forced separation between people who were in clear distress".
The authors argue that the exclusion of family carers flies in the face of evidence that they bolster patient health and healthcare systems. In all three countries, the financial value of informal care runs into billions of dollars or pounds every year. Additionally, patients with supportive families are more likely to adhere to treatment plans, have better communication with their clinicians, and have better clinical outcomes and quality of life.
While visiting bans have eased, wider exclusion continues. "Debates within health systems about 'living with Covid-19' focus on matters such as workforce, delivery models, and funding, but not on the role of families". To counter this, "government policies should formally recognise families as care givers, including paying for their labour, offering universal respite funding and services, and providing care giver benefits".
The authors conclude that "Valuing family care giving will finally make unpaid care giving visible, enable families to improve patient care and outcomes, support health systems, and better prepare systems for future healthcare crises".
Tuesday July 4th 2023
Partners in learning
The idea of patients as "partners in care" has been gaining ground for a while. With a growth in long term conditions, and with more and more people "self-managing" their health and wellbeing, it makes sense for clinicians and patients to work closely together.
So when it comes to patient experience work, should we think of patients and service users as "partners in learning"?
In the summer edition of our quarterly magazine, Maddie describes the experience of being disbelieved when she tried to share her own knowledge of her own condition. She calls for "trustful conversations" through co-production, where power dynamics between professionals and patients are actively examined, and people work together as one team, with everyone’s knowledge valuable and valued.
Our second contributor, Karl Roberts, picks up the theme of learning with patients. He describes an approach developed by the NHS Leadership Academy's Patient Faculty, in which patient partners and staff "plan together, train together and work together". As the Leadership Academy merges with NHS England, Karl makes the case for the Patient Faculty's legacy to be remembered and built on, and for the NHS to learn "with" patients, as much as "from" them.
As always, we also bring you the latest and best patient experience research, packaged in handy summaries for busy people. And we’re always keen to hear from our readers, so if you know of a standout report that we should be featuring, or if you want to submit a comment piece, get in touch!
Tuesday June 27th 2023
The hidden realities of personal budgets
"For us and many disabled people", say the authors of this paper, "personal budgets are a tool for liberation". But, they say, "this comes at a cost to the individual in terms of practical and emotional labour".
Liberation comes in the form of "self-determination over our lives". Personal budgets can give disabled people freedom from institutionalised care, as well as freedom to buy services and support to suit their own priorities. But within these freedoms are "hidden realities".
The authors reflect on how words like ‘fight’ and ‘battle’ are associated with the process of gaining a budget and maintaining the support they need. They have had to educate themselves about rights, laws and policies, in order to advocate for themselves. Even so, their advocacy is from a position of "being seen as inferior because we do not hold a professional status". It is also on top of the task of managing the disabling conditions that they are trying to get support for in the first place.
After winning a personal budget, the work continues. Recruiting a personal assistant involves advertising and interviewing, along with the difficulty of selling a job that is underpaid, and undervalued by society.
Then there is the task of managing the support: producing staff rotas, recording leave, maintaining timesheets, seeking training, managing employees, and submitting spending proof to the council.
"The relentlessness of this work", they say, "can and does cause burnout". Indeed, some disabled people have abandoned self-directed support in spite of the increased quality of life a personal budget provided.
The authors call for the voices and experiences of disabled people to be heard in order to inform the approaches of commissioners, social workers, policy makers and other individual employers. "Person-centred support is rightly celebrated for the choice and control it affords disabled people but managing this should not come at a cost to our health and well-being and more support needs to be in place."
Tuesday June 20th 2023
Fair care for diabetes
There are, says this report, "stark inequalities in diabetes care and management, which ultimately lead to worse health outcomes for those in the most deprived areas".
People from South Asian, Black African, and Black Caribbean backgrounds, for example, are two to four times more likely to develop type 2 diabetes, frequently at a younger age and lower BMI than White Europeans.
Deprivation is also key factor in diabetes inequality, with 24% of people diagnosed with type 2 diabetes living in the most deprived areas, compared to 15% in the least deprived.
A further factor is geographical variations. In some parts of England, health services have restored their diabetes care to above pre-pandemic levels. But the majority have not, with the lowest performing areas seeing only 1 in 10 people with diabetes get all of their checks.
The consequences can be serious - including amputation, stroke, heart attack and heart failure. There are emotional costs too - not just from lack of access to health services, but also from issues such as the increased cost of living and difficulties maintaining healthy diets.
The report makes a series of recommendations - both for government and for Integrated Care Boards. It concludes that "With the right care and support, people living with diabetes can lead healthy, productive lives". And, it says, "NHS England and ICBs could shift the focus of healthcare to empowering people with long-term conditions to stay well, rather than treating the devastating and complex consequences down the line".
Tuesday June 13th 2023
Hearing from bereaved families
In 2021, the Justice Select Committee called for major reform of the inquest system, and stated that much more needs to be done to put bereaved families at the heart of the process.
This report from a Family Consultation Day shows why. It looks at the experiences of people whose relatives died under the care of mental health services. It says that "Too many families told us they felt marginalised from before their loved one died, right up until the inquest hearing and after".
Key findings from the Family Consultation Day included:
- Inadequate communication. One example was that after a death, care providers were already looking to protect their own reputations and positions. This was described as lacking respect for those that had died and for grieving families.
- Poor information and support. There was a lack of advice on bereavement support, what to expect of investigations and inquests, and the coroner’s role. Some did not know they could request a post-mortem.
- Opaque investigations. Families described flaws in the independence, impartiality and quality of investigations. Many families remain angry, suspicious and distressed at the ways care providers conducted investigations.
Once inquests got underway, families felt "utterly unprepared for what was to come". The onus fell on them to work out their rights to legal representation, and to find the money to pay for it. Some found inquests taking place in venues that were hard to travel to. Some found the process itself unnecessarily adversarial. Some found themselves having to deal with the press and media.
When asked what needs to change, the families' comments echoed those of so many others who have experienced harm in healthcare: "If one thing united the group it was the desire to ensure others were not placed in the same position as them in the years to come".
There are many recommendations in the report, all coming from the families who took part in the Consultation Day. And all stem from the sense that "Ultimately, families are faced with a completely alien system that has inconsistent levels of information, empathy, openness and sensitivity".
Tuesday June 6th 2023
Who's excluded?
Discussions about digital healthcare tend to focus on the technology: the platforms through which patients can book appointments, the apps that help them with physical and emotional wellbeing, or the increasing role of AI in helping clinicians to make sense of big data.
But digital healthcare is not just about fancy tech and clever software. It's also about how patients organise and mobilise online. This article, by BMJ editor and cancer patient Tessa Richards, is a case in point.
It describes a webinar flagged by Richards' cancer Facebook group. She admits approaching it with a degree of cynicism, anticipating an "experts talk at patients" experience. Instead, she found a conference organised and moderated by patients, where the debate was assertive, informed and supportive.
In a reversal of the standard "patients included" approach to big healthcare jamborees, this conference featured professionals who were included not by right, but because they had been hand picked and invited by the patients.
This is part of a growing trend. Patients these days are not waiting to be invited to engage. They are doing things for themselves, in online communities. Other examples are the Melanoma Patient Network of Europe, featured in this edition of our quarterly magazine (page 4), and the Light Collective, shown here (page 4).
There is a lot of talk in digital healthcare about digital exclusion. Usually the assumption is that the people at risk of exclusion are the patients. Rarely, if ever, do health professionals consider their own risk of exclusion from online debates and initiatives being run by patients.
When patients organise online, they can travel light and move fast, in ways that large healthcare institutions can't. Health professionals need to keep up - or risk being left out.
Wednesday May 31st 2023
How restrictive practices affect women
The Mental Health Act allows a person to be detained in hospital in order to protect their safety or the safety of others. Alongside this are restrictive practices, ranging from restraint, seclusion and rapid tranquilisation to more subtle practices such as locked doors or restricted mobile phone access.
There is a difficult balance: restrictive practices are in place to promote safety but they can also limit a person's freedom, rights and daily activities.
The starting point for this study was that although the potentially damaging effect of restrictive practices is likely to be experienced by both men and women, it is possible that restrictive practices are harder for women. That is because restrictions in inpatient settings could mirror the lack of power and control that women hold in society as well as abusive life experiences they might have experienced. Further, women accessing mental health services are more likely than men to have suffered abuse both in childhood and as adults, and female inpatients are significantly more likely to have a history of sexual abuse than male inpatients.
From semi-structured interviews, an overarching theme of powerlessness emerged. Within that were four sub-themes:
- Restrictions perceived as punitive. Women felt that threats of restrictive practices were used to ensure they followed the rules. Loss of privileges were seen as ways for staff to keep control.
- Not being heard. One example was ward rounds where women felt unable to contribute to decisions that were made about restrictions. Some women described having to speak aggressively, or protest in an attempt to be heard.
- Impact of restrictions on relationships. Restrictions on visitors or mobile phone access affected the ability to form and maintain relationships. Some women felt 'awkward and ashamed' in front of their friends and families because of the restrictions placed upon them.
- Safety and support. Women felt that some rules needed to be in place to keep the ward calm and settled. Rules providing structure and routine were seen as good for patients' mental health. However, as their mental health improved, they perceived restrictions as more punitive.
The authors emphasise the importance of reflecting on how gender might influence treatment; of being aware of women's different experiences of trauma; and of wider social and political issues resulting in the oppression of women.
Tuesday May 23rd 2023
An unusual step
Sir Brian Langstaff, Chair of the Infected Blood Inquiry, describes this interim report as "an unusual step".
It is unusual because even before the Inquiry has completed its work and presented its findings, it is recommending a compensation scheme for people harmed by infected blood.
The scandal has been described as "the worst treatment disaster in the history of the NHS". People with haemophilia were particularly affected but so were many others, given transfusions for a range of conditions and circumstances.
One woman was infected in utero with HIV after her mother had a transfusion. Her sisters died, aged five and three, then her father, then her mother.
Around 380 children with bleeding disorders were infected with HIV and more than half have now died.
Other people were infected with Hepatitis C or Hepatitis B. The latter aggravates both Hep C and HIV, making the effects of those diseases worse. As well as losing their health, many lost their jobs. Family members have turned into carers.
Successive Secretaries of State - Andy Burnham, Jeremy Hunt, Matt Hancock - acknowledge the harm caused not just by the treatment, but by a persistent failure of response at the government level, which has compounded the harm.
Sir Brian has this to say: "People infected and affected have over decades sought recognition that wrongs had been done to them, and had been rejected". He goes on, "Once it is accepted, as it has been, that compensation should be paid, then it should plainly be paid as soon as possible. Many who should benefit from compensation are now on borrowed time. They know too many who have already died".
"I cannot in conscience", he says, "contribute to that further harm...This is why I am taking the unusual step of issuing one set of recommendations in advance of all others".
His recommendation? "It is time to put this right... a compensation scheme should be set up now and it should begin work this year".
Tuesday May 16th 2023
Technology-enabled lives
"Technology is central to our everyday lives" says this challenge paper from the TEC Action Alliance. But "all too often we separate it out for special treatment when it comes to supporting our care or health needs, as opposed to viewing it as a core tool which can help us live the lives we want to lead".
The focus of the report is technology-enabled care, or TEC for short. There are various examples of how it works in practice, including the case of "George" (a fictional persona) who has cancer. TEC can help George with pre-admissions screening, virtual appointments and remote monitoring. It can help him to manage multiple medications, and to manage his direct payments. Importantly for person-centred and holistic care, it can also help him to stay connected with family and friends who are central to his wellbeing and recovery.
The report also offers real-life case studies, as well as survey findings on public attitudes to TEC. But it notes that debates on digital healthcare are often about "digitising social care, health and housing: re-engineering systems and processes".
We don't hear so much about "technology-enabled lives, where the ambitions and aspirations of the individual come first, made possible by digital". The debate is "over-focused on the needs of the NHS", with less attention paid to the benefits to social care systems and even less on the benefits to people and their communities.
"To change this mindset", say the authors, "we must amplify the voice of people with lived experience so that we deploy technology to support what they want rather than what suits the system".
Their conclusion is that "It should go without saying that a better understanding of the needs and aspirations of people means that products and services can be developed that are more successful in meeting their needs".
Wednesday May 10th 2023
Self-rationing healthcare
To understand patient experience, we sometimes have to go beyond the basic "how was it for you?" approach of things like the Friends and Family Test.
Long term conditions are a case in point. NHS strategies from the Long Term plan downwards say that with a growth in long term conditions, we need to encourage "self-management", with people looking after themselves in their own homes and communities. But how well do we understand people's experiences of self-management?
This report looks at one important aspect: prescription charges. It starts with some useful facts:
- England is the only UK country where prescription charges still exist, having been abolished in Wales, Northern Ireland and Scotland.
- Charges have risen almost every year since 1979.
- Most of the income to the NHS from prescription charges comes from working-age people with long term conditions.
- Aside from the addition of cancer in 2009, the list of exempt conditions has not changed since 1968, even though there are new conditions like HIV, and some, like cystic fibrosis, which people can now live with for much longer.
Some people can get help with the costs - but only if they know help is available. In this survey, 83% of respondents had not heard of the NHS Low Income Scheme, and 38% only found out about the Prescription Prepayment Certificate more than a year after their diagnosis with a long term condition.
30% of respondents reported missing, or taking a lower dose of their medication, and 64% said they would be more likely to take medicine as prescribed if prescriptions were free.
The authors conclude that "charging working-age people with long term conditions for prescriptions is leading to self-rationing of medications". And they say that "This, in turn, is leading to increased pressure on the NHS and poorer health outcomes".
Access to medication is a vital part of self-management, and self-management is a key thrust of NHS strategies. So it is hard to argue with the report's finding that "the prescription charge exemption system needs urgent reform".
Wednesday May 3rd 2023
A familiar pattern
Last week's Featured Report was a paper which asked whether the NHS - ten years after Mid Staffordshire and the Francis Inquiry - is safer and more open.
This week, sadly, we feature a report which shows just how much work remains to be done.
The report sets out the findings of an investigation into safety and quality issues in Child and Adolescent Mental Health Services (CAMHS) at the Tees, Esk and Wear Valleys NHS Foundation Trust. Issues included multiple instances of inappropriate restraint and, worst of all, the deaths of three young women.
The events occurred in a care environment in which there was "insufficient attention and importance being applied to risk". Family members and carers said they "could not safely raise concerns", and "felt actively judged and undermined by staff". There was "a fundamental and consistent failure to inform parents about incidents involving their children under Duty of Candour".
There is a great deal more in this report, and it all fits with a pattern that, after Mid Staffs, Morecambe Bay, Gosport, East Kent and others, has become all too familiar.
Elements of the pattern include the fact that the key unit - West Lane Hospital - was geographically isolated, and a closed culture developed. There was a constant turnover of staff, and tension between different staff teams. Risk registers were poorly maintained. Actions, when required, lacked urgency. Staff training was inadequate. Local observation rules were applied, inconsistent with established Trust-wide policy.
Over and above all of this was a complacent governance. The Board was "overly accepting of verbal reassurance in relation to quality and safety" and displayed "insufficient curiosity". Reporting was "disjointed" and the Board Assurance Framework was "detached from the reality of the organisation".
The investigators state that "It is clear from our research that patients and their families (and some staff) were ignored and that their concerns and complaints are now found to be, on the whole, justified". This, too, is the kind of statement that we have seen too many times before.
The message for Boards and senior NHS managers is clear: dismissive attitudes towards patient experience lie at the heart of harm. Two years ago, our Inadmissible Evidence report called for an end to this double standard in evidence-based practice. Sadly, there is still no end in sight.
Tuesday April 25th 2023
Listening. Learning. Leading.
Ten years have now passed since the publication of the Francis Inquiry's findings on avoidable harm at the Mid Staffordshire NHS Foundation Trust.
The government's response, says this paper, "promised wide ranging interventions and legal and regulatory reforms". The question posed by the authors is "What is the legacy for the safety of patients in England?".
There has undoubtedly been action. The duty of candour has been introduced, along with Freedom to Speak Up Guardians. There have been changes to Care Quality Commission inspections, and the Healthcare Safety Investigation Branch has been set up.
In spite of all this, "Recurrent organisational catastrophes remain a disheartening reality". Oddly, the paper does not name any. But the roll call includes maternity services at Morecambe Bay, Shrewsbury & Telford and East Kent. The authors might also be thinking of medicines and medical devices - notably Primodos, Sodium Valproate and pelvic mesh. Perhaps they are also considering individual actors such as breast surgeon Ian Paterson, whose criminal activities went largely unchallenged by his employers.
The authors point to a common thread: "Failure to listen to the voices of patients and carers is a recurrent theme... and one that the system seems incapable of heeding".
There are three simple recommendations:
Listening. "Psychological safety - a sense among staff and patients that it is safe to speak up without fear of retaliation or being undermined - is critical."
Learning. "Collating, and acting on intelligence, quantitative and qualitative."
Leadership. "Making patients 'the first and foremost consideration' [with] an uncompromising focus on addressing cultural and behavioural problems."
With the ink still fresh on the East Kent report, and as we brace ourselves for the Ockenden report on Nottingham, these points need to be taken seriously.
Sunday April 16th 2023
Strong support for the NHS
The nurses' and junior doctors' strikes continue to rumble on, with Pat Cullen of the RCN warning of strikes until Christmas, and the government looking to tough it out.
So we know the positions of the key players - but what do patients and public think?
This paper from the Health Foundation finds, unsurprisingly, that "people are deeply concerned about the state of the NHS". Only a third think the NHS is providing a good service nationally, down from previous polling in 2022 and 2021.
63% think the general standard of care has deteriorated in the last 12 months, and only 9% expect standards to improve.
Across the nations of the UK, just 10% think their own national government has the right policies for the NHS.
In spite of all this, public support for the founding principles of the NHS remains, according to the Health Foundation, "rock solid". 90% want access free at the point of delivery, 89% want a comprehensive service and 84% want the NHS funded through taxation. "Each of these principles", says the report, "commands majority support right across the party-political spectrum".
Asked about priorities, 39% wanted to see more staff in the NHS, 35% wanted shorter waiting times for routine tests and operations,and 31% wanted shorter waits in A&E.
The authors state that "While both main parties have so far preferred to talk about reforming the health service rather than tax rises or spending increases, 82% of the public think the NHS needs an increase in funding, including 63% of Conservative voters". They warn that "With just 8% of people in England convinced the UK government has the right approach to the NHS, our latest survey should ring alarm bells for the Sunak government".
Wednesday April 12th 2023
Prison healthcare and families
"Individuals in our criminal justice system represent some of the most vulnerable people in our communities", says this report. It adds that "contrary to prison providing an opportunity to address health inequalities, evidence suggests that it often has a significant detrimental impact on health and wellbeing".
Families can help - not just through supportive relationships but also by alerting prison officers to matters such as "mental health, drug use (prescription and illicit), propensity to violence and risk to self". Indeed, NHS England states that "families are important to recovery and carers often hold information that allows services to work more effectively".
This study, based on interviews with families supporting patients in custody, offers useful insight, starting with the fact that most had witnessed "a significant decline in their loved ones’ mental and physical health during their custodial sentence". However, their ability to intervene was hampered by a lack of recognition for their role as carers, advocates, sources of information and vital support.
The report suggests a need to engage families at all stages in the criminal justice system, including arrest and police custody, during the judicial process, at reception into prison and during prison transfer, and at the point of release and during resettlement.
Through all of this, families themselves need to remain resilient. This can be hard when they "face the dual impact of losing a loved one to imprisonment as well as the anxiety associated with a loved one’s poor health". Their needs include provision of accurate information about prison life and how to support a loved one in custody; information and guidance about how to support their loved ones’ health and wellbeing needs; and family-friendly, non-judgemental support.
Tuesday April 4th 2023
People and politics in healthcare
Is healthcare personal or political? The answer, of course, is that it is both, and the contributors to the latest edition of our quarterly magazine unpick both strands.
Charlotte Augst, until recently the CEO of the National Voices coalition of health and care charities, argues that an NHS creaking from years of underinvestment needs a 'laser sharp focus on the experience of people using services'.
NHS strategists, she says, like to talk about ICBs, place-based strategies and provider collaboratives. But these mean nothing to people stuck in ambulance queues, or on waiting lists, or in GP call handling systems. Augst makes the point that patients are also voters, and NHS leaders need to offer pragmatic solutions to stave off political as well as personal discontent.
Andrea Downing is founder of the Light Collective, which campaigns for the rights of patients in the digital health sphere. She looks at the advertising and marketing tactics used by digital medicine companies to extract health information from users. Who sees what data, and how are specific patient populations targeted? And to what extent do those companies comply with their own privacy policies?
The answers should be of concern to legislators and regulators, as well as to patients.
As always, we also bring you the latest and best patient experience research, packaged in handy summaries for busy people. And we’re always keen to hear from our readers, so if you know of a standout report that we should be featuring, or if you want to submit a comment piece, get in touch!
Tuesday March 28th 2023
Openness in healthcare
"Openness, transparency and candour are recognised as ethical responsibilities of health care organisations", says this paper, and yet "delivering on these commitments in health care systems has often proved challenging".
The authors point to Mid-Staffordshire as a prompt for extensive policy interventions to promote openness. But they go on to say that subsequent scandals "have continued to identify pathological organisational behaviours and norms, including marked deficits in openness".
The paper identifies four necessary conditions for change:
- Authentic integration into organisational mission. Organisations that had made greater progress framed openness as part of mainstream business, not an optional bolt-on. Freedom to Speak Up Guardians were given significant investment to ensure that they had sufficient time to deliver the role. Interventions such as behavioural standards frameworks were actively promoted "to ensure that they were more than rarely visited webpages or documents to gather dust".
- Functional and effective administrative systems. These included tight oversight of disclosure and investigation processes, rapid dissemination of learning and implementation of recommendations, and integration of different sources of organisational intelligence about concerns and risks.
- Flexibility and sensitivity in implementation. "Coldly efficient systems" for investigation of concerns could be seen seen by staff, patients and families as unhelpful and even upsetting. There is a need to "soften systems by giving them a human touch" via judgement, flexibility, discretion, and the occasional workaround.
- Continuous inquiry, learning and improvement. This involved "protracted and dogged efforts to improve, sometimes using formal improvement approaches, sometimes more ad hoc". The approach to implementation was open-ended and extended beyond discrete, time-limited improvement projects.
Against these, the paper lists four persistent challenges, including:
- Reliance on goodwill, for example from underfunded Freedom to Speak Up Guardians.
- A lack of care for staff, patients and families - for example, if they sense that raising concerns could be risky.
- Reliance on values, which can be ineffective against staff who remain resistant to greater openness.
- The continued marginality of patients and families. Here, the paper makes the point that "openness policies... focus primarily on organisations and staff. We found that patients and families were mainly bit-part players in enacting the policies".
This last point is important. The authors comment that "Disappointing, and perhaps surprising given their prominence in unearthing problems at Stafford Hospital and elsewhere... the principal mechanisms through which patients and family members can raise concerns about quality and safety remain largely the same as they were in the 2000s".
So there is much in this paper that individual providers could learn from. And we must hope that national bodies are also paying attention.
Tuesday March 21st 2023
Safe relationships, safe care
Patient safety has been identified as a key pillar of high quality healthcare, alongside patient experience and clinical effectiveness. According to this study, patients can play an active role - not least as "vigilant monitors": asking questions, raising concerns and double-checking things like medication timings and doses.
There is a problem, however: patients can be reluctant to raise safety concerns if it means challenging staff - over infection risks from poor handwashing, for example. Key to this is vulnerability: patients are dependent on, and place their trust in, healthcare staff. Fear of damaging their relationship with staff has been identified as a significant barrier to patients' involvement.
When patients are admitted urgently to hospital, vulnerability is increased. There is a loss of integrity and dignity, and, at worst, a profound fear of the unknown, or of dying. In these situations, patients seek reassurance that the hospital is a place of safety, and that they can entrust themselves to the care of the staff. Signs of safety are both contextual (impressions of order, cleanliness and sufficient staffing) and relational (the perceived competence and responsiveness of staff).
One implication, say the authors, is the importance of relational work for patients as a way of keeping themselves safe. To demonstrate that they are 'good patients', they avoid being too demanding, comply with instructions, and display gratitude to staff for the care that they receive.
For patients, then, safety is about vulnerability to harm from both their health status, and from their dependence on the healthcare organisation and the professionals within it. They conduct risk work by seeking reassurance and undertaking relational work - but this can conflict with their additional need for vigilance, and double-checking aspects of their care.
"The difficulty for patients", says the paper, "is that both options may increase their vulnerability, one from harm if trust is misplaced and another from potential damage to relationships from challenging healthcare professional expertise".
The authors suggest that we need to rethink the idea of the 'good patient' - recognising and valuing vigilance alongside compliance. "Both patients and healthcare professionals", they say, "need to recognise how their interactions co-produce safety at the point of care. Seeing safety as co-produced by patients and professionals... might allow risk work to take place without disrupting relationships".
Tuesday March 14th 2023
Taking patient engagement onstage
Traditionally, patient feedback is channelled through mechanisms such as the Friends and Family Test, or patient surveys. Either way, it is healthcare staff who decide how and where the feedback is presented and reported.
Online platforms such as Care Opinion bring patient feedback into the limelight. They challenge providers to play out their responses in real time and in front of a live public audience.
This study uses the analogy of performance to unpick the ways in which providers deal with online feedback. In this analysis, healthcare staff are "actors" who work "backstage" on script development and rehearsals for handling feedback, before going "frontstage" to display their public response.
Three NHS Trusts were studied in the context of their handling of feedback via Care Opinion: a non-responding organisation (site A), a generic responding organisation (site B) and an organisation that provided transparent, conversational responses (site C). Comparisons included the following:
- Audience interaction. Site A had 2,120 patient narratives via Care Opinion during the study period, and at the start, had a response rate of 0%. Site C had 6,500 patient narratives in the same period, and by the end had posted over 7,500 staff responses which had been read more than 1,787,900 times.
- Script. Standardised scripts were used at site B, to post generic responses. Conversely, site C staff were guided by "stage directions", crafted to encourage conversational responding, and giving "actors" freedom to improvise.
- Spotlight. Site C aimed to ensure that all patient experience information was made publicly available. Site A staff were keen to remain in the shadows where possible, turning a blind eye to what was perceived as the "booing online crowds". Site B were intrigued to peer onstage and understand how the audience were receiving their services while taking comfort in handling responses offline and behind the scenes.
- Cast list. Site C had a team of over 890 staff able to monitor and respond to online patient feedback, in comparison to a maximum of two at sites A and B.
The paper addresses the fears felt by some organisations about having their interactions with patients out in public view where "the whole world and their dog can see". But it counters with some powerful quotes from Site C staff:
"If you’re not hearing negative feedback, it’s because it’s being said elsewhere."
"It’s one of the strongest forms of governance... You can think, 'Well I’ve heard this from the staff and I’m hearing this from the patients. What is this all really telling me?".
"Two years, and nothing really happened. But when the story was placed on Care Opinion we were able to resolve it in 6 weeks."
Tuesday March 7th 2023
Follow the money
"We will put patients at the heart of the NHS."
Back in 2010, this was the bold promise of the newly elected coalition government, set out in its paper "Equity and Excellence: Liberating the NHS".
The paper was published as the Francis Inquiry was shocking the nation with revelations of large scale harm at the Mid Staffordshire Trust. That inquiry was highly critical of the Local Involvement Network (LINk) - the government-funded patient voice body which should have spoken up for patients but had manifestly failed to do so.
The government's response was to abolish the England-wide LINk network and replace it with a more effective version. "Liberating the NHS" said "We will strengthen the collective voice of patients and the public... through a powerful new consumer champion, HealthWatch England".
The government recognised that the weakness of the LINks was in part due to inadequate funding, at just £27 million per year for the entire national network. So when Healthwatch was established in 2012/13, it was given a considerably increased allocation of £40.5 million.
But the network had hardly got started before the funding began to be cut. It has been whittled down in each and every year of the Healthwatch network's existence and, according to Healthwatch England's latest "state of funding" report, now stands at £25.4 million.
Far from strengthening patient voice in England, the government has reduced its financial strength to below that of the LINKs, over a decade ago.
In this context, the promises to learn from the Mid Staffordshire disaster seem empty. So too does the promise to put patients at the heart of the NHS.
There is, however, one key lesson. To really understand the government's intentions in respect of patient voice, follow the money.
Tuesday February 28th 2023
Mutual healing and patient safety
"It is well known that healthcare workers make decisions that affect patients’ lives while under pressure to do better, faster and with fewer resources", says this research paper from Canada. It continues: "These circumstances can lead to medical errors, often because of a system failure, and occasionally due to human error".
The authors recognise that for patients, caregivers and family, the consequences of medical error can be profound, encompassing physical, emotional and psychological harm. And they note that healthcare workers too, can feel guilt, shame and distress.
Organisations such as Patients for Patient Safety Canada believe that healing can be possible if healthcare workers and patients are able to meet, work together and explore harmful events and the feelings associated with them. However, "Research in this area is scant".
In this context, the researchers asked "How might purposeful conversations between patients and HCWs promote mutual healing and wellness after the disclosure of a medical error?". They carried out a literature review backed up with semistructured interviews to draw out relevant insights.
One finding was that in the aftermath of harm, patients and healthcare workers have considerable common ground. "Both want to tell their stories - and to listen and be heard... both desire to learn from the experience and make sure it does not happen again".
But there are also clear barriers: healthcare workers may be afraid of legal action, or of a psychologically unsafe culture within their organisation. Patients, for their part, can feel a sense of betrayal and mistrust, or can fear that re-opening discussion of the error might retraumatise them.
The key to unlocking a healing dialogue, say the authors, is to bring the common ground and common barriers into the open. This can help all parties to understand "how, why and under what circumstances these purposeful conversations could be most valuable and effective". The goal, ultimately, is to "breach barriers and foster the desired outcomes of apology, understanding and learning from the experience, ultimately improving the quality and safety of healthcare".
Tuesday February 21st 2023
A national imperative for care
This House of Lords report on adult social care opens with a stark fact: around 10 million of us are affected by the adult social care system in England at any one time. In spite of this, "adult social care continues to be largely out of sight and off the public agenda", and our understanding of adult social care "is partial and often flawed".
The report, by the Adult Social Care Committee, says that "Drawing on adult social care should not be seen as a disaster" but it is also clear that the state of adult care is verging on disastrous. It says that:
- The last ten years have seen a 29% real-terms reduction in local government spending power, and an estimated 12% drop in spending per person on adult social care.
- An estimated 44% of working age adults who were caring 35 hours or more a week live in poverty.
- The average person now has a 50% chance of becoming an unpaid carer by the time they reach 50.
The report covers the testimonies of unpaid carers - the people who have to "step up to provide care and support when the system is failing". It describes the exhaustion of people living with the assumption that social care happens first and foremost in the family circle. An assumption which means the work of unpaid carers is "largely invisible, unrecognised and unsupported".
The Committee calls for adult social care to become a national imperative with an appropriate and long-term funding settlement. It says that people who draw on care should have the same choice and control over their lives as other people. Thirdly, it wants an end to the assumption that families will automatically provide care and support for each other because no other choice is open to them.
The report notes that:
- The government's social care funding reforms were supposed to be introduced in 2023 but have now been delayed to 2025.
- There is a government commitment to a comprehensive workforce plan for the NHS, but silence on the need for an adult social care workforce plan.
- The Chancellor's autumn 2022 statement "does nothing to raise confidence that disabled adults and older people will be able to get the care and support they need to live good lives, or that the often forgotten unpaid carers who support them will be better off".
The Committee finds that "Without a fundamental rethinking of how we understand, approach and design social care... we will keep failing disabled adults, older people, unpaid carers, and ourselves".
Tuesday February 14th 2023
Vaccine compliance and defiance
In June 2021, with both the pandemic and the vaccination roll out in full swing, we featured a study of vaccine hesitancy in Bradford.
Misinformation was a key factor - but the study participants were not naïve victims of conspiracy theories. They had good reasons to be confused by information coming from multiple sources, anxious about rapid development of a new vaccine, and mistrustful of government.
Eighteen months further on, the authors have published a follow-up.
11 of the twelve original participants had had at least two COVID‐19 vaccines, and most were intending to get their booster. In spite of this, they still harboured doubts.
A common concern was safety: "most were keen to make clear that they did not believe any ‘conspiracy’ stories about the vaccines, yet common tropes about the vaccines' safety, such as them changing your DNA or causing infertility, were part of their narratives".
Confusion continued to arise from discussion and rumour among friends and online groups, and some felt overwhelmed by conflicting accounts. The paper states that "Making sense of the deluge of information about COVID‐19 since March 2020 appeared to have had an emotional and mental toll, which led to people purposefully choosing to disengage". It goes on to say that "this disengagement had led to people being less informed about what the current official guidance on vaccines was".
Mistrust had not been helped by the conduct of people in positions of responsibility: "at the time of the interviews, there had been several reports about those in the Government not abiding by lockdown rules". One participant also believed that the Government had allowed private companies to "monetise the pandemic".
The authors say that their findings "illustrate the continuum of vaccine hesitancy and acceptance and recognize that those who have chosen to have the vaccine may still have doubts and concerns". This, they say, is important because "it means that we cannot take their current vaccine acceptance for granted".
Encouragingly, the study found that while trust in the national government was low, the participants' most trusted health source was the local council. Positive discussion about COVID‐19 vaccines with family and friends was also persuasive.
The authors conclude that "Although the misinformation machine is global, continuing to foster and develop strong and trusting relationships locally can help erode some of its impacts... This further underlines the importance of health messaging that leverages personal relationships and positive emotions".
Tuesday February 7th 2023
Donations and disclosure
Understanding financial relationships between patient groups and pharmaceutical companies is, according to this Canadian study, necessary for understanding the position that patient groups take when the interests of companies are involved.
In one example from Canada, 87% of patient groups making submissions to an official drug review declared conflicts of interest. The groups also supported funding in over 90% of their submissions to the review.
Correlation is not causation. But the example highlights the need for transparency.
Unfortunately, transparency is somewhat lacking. The paper states that "Innovative Medicines Canada (IMC), the lobby group representing brand-name manufacturers, has included a voluntary guideline for its membership stating that they should disclose... a list of all stakeholders to which they provide direct funding'. But it goes on to say that "there are no penalties for not disclosing and no evaluation has been undertaken to determine if companies are voluntarily complying with this provision".
Patient groups, for their part, tend to be registered charities, and therefore file annual financial reports. But "those publicly available reports do not contain information about individual donations".
The study searched the websites of IMC members and patient groups. It found that "only a quarter of IMC members... reported making donations to patient groups on their websites and frequently only the names of the patient groups were given and the value of the donation and its purpose were omitted". In spite of this, "There were no reports on the IMC website about companies failing to comply with the guideline".
Almost one-third of patient groups did not report receiving donations from companies that claimed that they donated. Patient groups also infrequently reported the year the donations were made, and no patient group reported the exact value of the donation. Only 4 groups reported the purpose of the donations.
The results are, according to the author, "broadly in line with studies in other countries". For example, "The percent of the membership of the Association of the British Pharmaceutical Industry that reported making donations to patient groups varied from 45% to 66% depending on the year". Indeed, "Based on the experience in the United Kingdom, voluntary reporting of industry donations on the websites of charity regulators results in significant under-reporting".
The author argues for mandatory reporting by patient groups, possibly as a requirement for retention of their charitable status. And, he says, "Providing more information about donations will increase the accountability of both companies and patient groups and heighten transparency about their activities".
Tuesday January 31st 2023
The lazy language of lifestyles
One of our previous Featured Reports looked at the ways in which health inequalities are understood and addressed in NHS policy documents. It found a widespread use of value judgements applied to local populations - revealed through discussion of lifestyle and behaviour being major determinants of health.
This editorial addresses similar problems in Australian healthcare policy. It states that "the influence of one's ‘lifestyle’ in the prevention of chronic disease... continues to permeate national and jurisdictional public health policies, and the professional and public discourse". This is in spite of the fact that "it is the social, cultural and commercial forces that have the strongest influence on a population's health".
The authors contend that the lazy language of lifestyles "perpetuates the myth that improving the public's health is a personal responsibility". But, they say, the myth is not just based on lazy thinking. "In some cases... this is explicit - a deliberate 'pollution of health discourse', driven by commercial industries with vested interests, or by those with particular ideological standpoints."
Taking obesity as an example, the paper sees it as "implausible that the dramatic rise in the prevalence of overweight and obesity across most high-income countries... has been due to a sudden, concurrent, generational shift in everyone's personal responsibility". And yet, "this narrative continues to pervade, leading to weight stigma among those experiencing overweight and obesity and preserving the belief that improving knowledge and redressing a supposed lack of individual motivation is the obvious solution".
The effect of an overemphasis on individual lifestyle can be "a diversion of attention away from those upstream primary preventive actions that are likely to be most effective at bringing about equitable, sustained improvements in health".
"Language matters", say the authors, and we need to avoid "the ‘zombie hypothesis’ that one's health is simply down to one's choices". They argue that we need to reframe the narrative, "challenging the dominant public discourse on personal responsibility; preferencing evidence that addresses the social, ecological, cultural and commercial determinants of health".
"Avoiding the lazy language of lifestyles", they say, "would be a good start".
Tuesday January 24th 2023
Government foot-dragging on harm to women
In July 2020, Baroness Cumberlege published her First Do No Harm report on avoidable harm arising from medicines and medical devices - specifically, Primodos, Sodium Valproate and pelvic mesh. The harms were well known because the many thousands of women affected had been speaking up for years, even decades. But no-one had wanted to hear them.
This report from the House of Commons Health and Social Care Committee comes two and a half years after the Cumberlege Review, and documents an evidence session to consider the government's response. The members heard "heart-breaking accounts of how the health system had failed to provide proper guidance, care and support, even when it was known that harm was occurring".
The Committee's assessment of the government response includes the following:
- "Without records of which patient has undergone which procedure, or been prescribed which drug, the health system will continue to... fly blind."
- "Although the retrospective audit of mesh implants is an encouraging first step, it will be unlikely to reflect... all of the adverse effects women have experienced due to the nature of data used in the audit."
- "We were encouraged to hear that the Government is going ahead with pilots of a register of clinicians’ interests, but we are disappointed by the speed at which the Government is acting on this recommendation."
- "Although the Government has also given itself the powers to set up a register of industry payments to clinicians, no decision has been made yet about how to implement it, and officials were not able to share a plan of when the register would be active."
- "Although the vision for what the role of Patient Safety Commissioner will achieve is publicised by the Department, no statement of specific assignments or areas of responsibility, have been published yet."
There is more besides, but it is clear that the government response is, at best, sluggish. Worse still, it seems detached from the needs - and knowledge - of the tens of thousands of women who continue to live with mesh-induced injuries, and in the case of valproate, birth defects and developmental issues for their children.
The Committee states that "We... urge the Department to reflect on the experience of some of the stakeholders with lived experience in this instance, and to consider how to improve engagement with them in the future".
Tuesday January 17th 2023
Access to records? Not yet.
Back in 2019, the NHS Long Term Plan called on health services to deliver more person-centred care. Part of the follow-through was that all GP patients would have "online access to their full record, including the ability to add their own information, as the default position from April 2020".
This paper looks at what has happened since then.
According to the authors, NHS England planned to provide citizen access to general practice records in December 2021. But the launch was put back to April 2022, and then further deferred to November 2022. Then, just two days before the November deadline, the BMA called for a total rethink of the programme.
"It remains unclear", says the paper, "when default access will be available for everyone".
In the absence of default access, patients still have a legal right to apply for access to their own health information. But "those who request it often face barriers or are given only limited data". Similarly, information on things like consultations and test results is technically accessible through the NHS app. But "most patients have not been 'enabled' to see it, and many are unaware that this is possible".
The paper makes the point that "Incomplete and uneven access to personal health information makes little sense to patients and their carers. Lack of timely access adds to their healthcare burdens".
The authors conclude that " With access to care in the UK among the worst in Europe, patients have little choice but to be more self-reliant". They argue that "Ready online access to their full health record would help them and also reduce demand on the health system. The commitment to provide it", they say, "should be realised".
Tuesday January 10th 2023
Engaging engagement
People in healthcare talk a lot about engagement with patients and public.
Sometimes they call it 'involvement' or 'participation'. Other terms are 'co-production', 'co-creation' and 'co-design'. What does it all mean? The answer seems to be that nobody is quite sure.
Back in 2018, NIHR Involve described a lack of consensus around the concept of co-production. In the same year, an academic paper spoke of 'a lack of a common language' for patient and public involvement (PPI) and said that 'the term PPI is not universal in its application or definition'. More recently, the Social Care Institute for Excellence has said that "There is no single formula for co-production".
If anyone does know about co-production, however, it is Gill Phillips, who has huge experience in bringing patients and professionals together in common cause. Her prescription for good engagement? Make it engaging! In the latest edition of our quarterly magazine, she offers some great tips for what that looks like in practice.
Of course engagement is not always about 'professionals' seeking to involve 'service users'. Patients are perfectly capable of acting for themselves - through peer support, education, shared experience and more. Our other contributor, Liza Morton, describes her journey from congenital heart disease in infancy to a career as a psychologist and advocate for psychologically informed medicine. And she explains how engagement with both hearts and minds is essential for healing.
Monday December 19th 2022
Data-driven inequality
"Data saves lives" says the Department for Health and Social Care, in a document advocating better use of data for purposes including "tackling unequal outcomes and access".
The Ada Lovelace Institute agrees that data-driven systems can provide better health and wellbeing outcomes but warns in this report that they also risk exacerbating existing inequalities in health. In particular, "Data-driven systems can both alleviate and entrench inequalities - but the latter may be more likely when people’s needs are sidelined in service of an overreliance on data".
The report aims to describe the "complex interplay between data and inequalities" by looking at the pipelines of data that power health technologies. Its premise is that the ‘smooth’ data pipeline is a "hypothetical ideal that does not reflect the complexity and imperfection of reality". In real life, it says, data pipelines are knotted, with complexities and flaws including the following:
- Inequalities can be poorly understood, described and measured.
- There can be tension between local and national priorities for design and delivery of data-driven systems.
- Datasets can be of variable quality, or incomplete, or out of date.
- Data curation involves a tension between making data digestible for busy professionals, and making it nuanced and meaningful.
- Data is a proxy for truth and reality - some people's lived experience might be different from the numbers.
- Data that is devoid of local and historical context can lead to misinterpretation and poorly targeted interventions.
The report makes the important point that " data-driven systems are more than just the technology: they also include the people who develop, design and use these technologies - engineers, product teams, clinicians, hospital administration staff and others". Those people risk building in inequality while designing data systems, or compounding inequality via their interpretation of the data produced by those systems.
Accordingly, there is a need for system designers and users to take a people-centred approach - always considering the context in which data is collected, used and understood, and considering who is involved in decisions.
Monday December 12th 2022
Open access training for patient experience

Patient experience work is not easy. Not least because evidence on people's experience of care comes from so many different sources: patient surveys, local Healthwatch reports, academic research, online feedback and more. How are patient experience staff and patient reps meant to keep track of it all - and to start making sense of it?
Matters are not helped by the fact that there is no standard training for patient experience staff, and no professional development pathway. The Parliamentary and Health Service Ombudsman's "Making Complaints Count" report has made the point that complaints managers, for example, 'often receive limited access to training and are asked to address serious and complex issues with little assistance'.
So we have been working with the NHS Leadership Academy to start tackling the training deficit in patient experience work.
An online course is now available via the Academy's website, covering:
- Who does what in patient experience evidence gathering.
- Key concepts in patient experience work.
- Why patient experience matters.
- Challenges of hearing from patients.
- How to find different types of patient experience evidence.
- How to start making sense of patient experience evidence.
The course is free, and learners can log in at times that suit them, with the ability to pause part way and carry on at another time if they want.
It is designed to be helpful for people who are new to patient experience work, as well as for people who are familiar with the basics but need to consolidate their knowledge.
As well as people in PALS teams, complaints, local Healthwatch etc, the course could be helpful for patient reps on engagement committees - and for any nursing directorate staff or Trust Board members who need a good grounding in patient experience work.
To find the course, simply go to https://leadershipnhs.uk/, select your region and create an account (free), or log in if you are already a user of the Leadership Academy website.
After that, look for "Patient Experience" in "Leadership Modules" and get started!
Tuesday December 6th 2022
Backlogs and ethnicity
The starting point for this report is the "huge backlog in routine hospital care (known as the ‘elective backlog’), with more than 7 million patients in England waiting to begin hospital treatment".
The authors go on to note that the NHS has a legal duty to "have regard" to reducing health inequalities, and that it has specifically committed to taking account of inequalities in how it addresses the elective backlog.
The report analyses hospital data from March 2019 to February 2022 and finds that while the number of operations and procedures fell during the Covis crisis, "the falls in activity were not uniform across the different ethnic groups".
The "Asian group" saw the largest overall fall in the first year of the pandemic (a fall of 49% for all procedures compared with 44% for the White and Black groups). There was a less consistent pattern for the "Black group", who had larger rate falls than the "White group" for cardiac and cataract procedures, but otherwise saw similar changes to the White group.
The most deprived groups in the population also experienced larger rate falls overall, and this matters because "There is a strong link between health need and deprivation, which has a disproportionate impact upon people from ethnic minorities".
The report offers considerable further detail, but says that more analysis is needed to better understand the variations. In particular, "Inconsistent, incorrect and incomplete coding of ethnicity in health records means that our understanding of this complex picture is limited".
Limitations include restricted ability to look at particular ethnic groups within the broad categories examined in the research. "Understanding how this variation maps across subgroups experiencing deprivation, like Bangladeshi and Pakistani people, would be illuminating".
"More broadly", says the report, "the lack of data also limits progress in understanding how to reduce health inequalities across health care - something the NHS has a legal obligation to do". One important consequence is that "Quite simply, patchy data means that the NHS is flying blind in its attempts to meet this legal, and moral, obligation".
Tuesday November 29th 2022
How and why people use A&E
Accident and emergency (A&E) departments have been in the news all year, with photographs of long ambulance queues, and debate over whether or not to scrap the four-hour target for admission, transfer or discharge.
As part of efforts to understand the causes, and possible remedies for the crisis, NHS England commissioned a number of organisations including the Patient Experience Library to look at patient experience in urgent and emergency care (UEC).
We reviewed four years' worth of studies from sources including government bodies, policy think tanks and academic institutions, alongside the biggest single source - the local Healthwatch network. Some key findings were as follows:
- Awareness of the range of UEC options is generally good but patients and public are sometimes confused about the difference between A&E and walk-in centres, minor injuries units and urgent treatment centres. Confusion is compounded by the patchy availability of some of these, in terms of both locations and opening times.
- A key driver of attendance at A&E is the difficulty of getting appointments or advice from GPs and NHS 111. Another is that people are not getting the support they need in the community - for example to manage long term conditions. Some of those going to A&E are clear that they would have preferred a GP appointment.
- Some evidence suggests that referrals to UEC might not always be appropriate. Between 2019 and 2021, GP referrals in general increased significantly (179%), but avoidable attendances from GP referrals more than doubled (255%). Care homes might be taking an overly cautious approach - 41% of care home referrals may be avoidable. NHS 111 might also be over-cautious.
- Patients enduring long waits in A&E seem less concerned about adherence to the four hour target (if they are even aware of it) than about unpleasant experiences in waiting areas - some with possible clinical or patient safety risks. Some discomfort could be mitigated by better communication - for example regular updates on anticipated waiting times.
Our report fed into wider research, including social media tracking and face to face engagement with patients and public. Further details of the wider project can be found here.
Tuesday November 22nd 2022
Breaking the menopause taboo
'Despite the fact that 51% of the population will experience the menopause, the entrenched taboo around women’s health issues, at times underpinned by sexism and ageism, has meant that the support for the 13 million women currently going through peri-menopause or menopause is completely inadequate.'
So says the All Party Parliamentary Group on Menopause whose aim, in writing this report, was to assess the level of understanding and consider how government can drive policy change.
A key finding was that women themselves are often not equipped with the information they need to understand what is happening to them. Similarly, a 'lack of awareness and understanding within the medical profession, has meant that many suffer without their symptoms being recognised'. The report notes that 'It is astounding that 41% of the UK’s medical schools do not have mandatory menopause education on their curriculum'.
The consequences are not just medical - they are social and economic as well. The report states that 'Evidence shows that those experiencing menopause at work... are less likely to go for a promotion, and are more likely to leave their roles before retirement'. It says that 'With women often at the peak of their careers during the menopause transition, this exacerbates gender inequality in senior roles and adds to the gender pay-gap'. In spite of this, 'the majority of employers do not consider menopause a proper health condition and do not have policies in place to support staff going through it'.
As in other areas of health care, there are inequalities. The cost of Hormone Replacement Therapy, for example, 'remains a barrier for some women'. Another is that 'women face a postcode lottery on whether they can access the right treatment from their GP'. A third is that 'there is an assumption that menopause is the same for all those who go through it, and culture and ethnic differences are not accounted for'. But 'some South Asian communities don’t even have a word for menopause... given the taboo in talking about health conditions generally - particularly women’s health'.
The report makes a series of recommendations, while acknowledging that 'There is much that needs to be changed around the menopause, and unfortunately there is not a simple legislative lever that can be pulled to do so'. But, it says, with 'more widespread conversations and policies in the workplace; better education of healthcare providers and improved healthcare pathways; we can start to make the menopause taboo a thing of the past'.
Tuesday November 15th 2022
Caring for carers
Unpaid carers provide essential care worth more than £132 billion a year. Their support to vulnerable adults and children has become a fundamental part of the health and care system. Indeed, evidence suggests that the UK relies more heavily on unpaid carers to provide social care than many other countries do.
In spite of this, however, many carers are struggling without adequate recognition or support.
This report measures progress made against policy commitments set out in a series of government strategies, action plans, White Papers and legislative measures from 2008 onwards. It finds that 'Despite the laudable policy statements in support of carers... the reality for unpaid carers has been one of diminishing help over time'.
There are a number of facets to this, starting with the fact that we do not actually know how many unpaid carers there are. According to the report, 'we lack robust up-to-date data'.
In the meantime, local authority assessments of carers’ support needs seem to be lower in number than might be expected, and among those who have had a carer’s assessment, substantially fewer are now receiving direct support. An increasing number are getting only ‘advice and guidance’.
Breaks from caring are essential to protect carers’ physical health, and also their mental wellbeing. But, says the report, access to breaks for carers is declining.
People’s satisfaction with support is low and has been getting worse.
So why is the policy vision not being achieved? Partly because of a lack of accountability and agreement on who is responsible for policy success and failure. And partly because strategies can be unclear on how success should be measured. But also because of a failure to actively consider carers in wider policy decision-making. And that’s before you get to lack of funding...
The report addresses these via a series of recommendations. Ultimately, though, the fact remains that in spite of policy pledges, 'Carers report finding it harder to access adequate advice and support, and satisfaction with carer support services is declining'.
Tuesday November 8th 2022
The wall of beliefs
This guide is aimed at policymakers and communicators whose efforts may be frustrated by false narratives and misinformation.
In healthcare, that can apply to important issues such as vaccination and mask-wearing, as well as to spurious 'cures' for serious illnesses. But the techniques explored in the guide can also apply to more day-to-day matters such as handwashing in healthcare settings.
The starting point is the 'wall of beliefs' - the various influences from which we construct our belief systems, and, to some extent, our personal identities. The point here is that belief is not simply built on facts. It also comes from social conventions, peer pressure, religious faith and more.
Because of this, myth-busting approaches can often fail to change people’s minds. The arguments for mask-wearing might be scientifically persuasive - but if none of your family or friends use a mask, you probably won’t either.
Rebuttals can also fail to cut through when people hold onto beliefs because they form a foundational part of their identity and worldview. In this case, a counter argument - however strongly evidenced - can threaten people’s self-esteem and cause defensiveness rather than a change of mind.
The guide offers a strategy matrix, based on understanding how strongly or weakly beliefs are held, and whether the resulting behaviour is harmful or not. A corresponding set of tactics looks at incentives and barriers for desired behaviour, along with communications that can address harmful beliefs without backing the intended audience into a corner.
'Overturning false beliefs', says the guide, 'is not as straightforward as simply supplying true information, or debunking falsehoods'. That advice - and the solutions presented in the guide - could be very useful to healthcare practitioners and policymakers.
Tuesday November 1st 2022
Speaking well
Last week, we featured the East Kent report on avoidable deaths in maternity services. It revealed an organisational culture characterised by 'denial, deflection, concealment and aggressive responses to challenge', along with 'bullying to such an extent that the maternity services were not safe'.
But what does a good healthcare culture look like? This report from the Health Foundation offers some clues. Based on an evaluative study of five English NHS Trusts, the focus is on quality improvement, and how good culture can enable organisation-wide learning.
First of all, stability matters: the report notes differences between one of the Trusts it studied, which had had the same Chief Executive since 2010, against another, which had three Chief Executives in quick succession.
The framing of improvement efforts also has an influence. An initiative seen largely as a technical exercise led by experts is unlikely to enter the 'mainstream consciousness' of the organisation. But if it is seen as core to the organisation’s identity and strategic vision, it stands a much better chance of having impact at scale.
Values are important too. One of the Trusts that performed well on quality improvement had co-produced a set of values with its front-line staff. The outcome (which might feel challenging to some NHS Boards) was to 'put the patient and quality of care first, above that of finance'.
Alongside all of that is the 'social connectedness' of staff. The study found 'stark differences' between the Trusts it looked at, with Surrey and Sussex, a Trust rated as outstanding by the CQC, having a much higher level of social connectedness among staff than the two Trusts with the lowest CQC ratings. It states that 'Whereas the former was characterised by ‘close relationships, mutual collaboration and feedback’, the latter had a high level of simple, one-directional exchanges, suggesting a lack of collaboration between individuals'.
The reports says that 'organisations wanting to strengthen their capacity to innovate and improve should put the creation of peer learning and knowledge exchange networks at the heart of their strategy, and treat it as an essential component, rather than simply a desirable one'.
It adds that 'One of the first steps on Surrey and Sussex’s improvement journey was to make sure that staff were, as Michael Wilson, the trust’s former chief executive, put it, ‘speaking well of ourselves, well of each other, well of our organisation and well of our community’. Once this becomes the norm, it becomes easier for people to have meaningful conversations about improvement'.
Monday October 24th 2022
Responding to challenge with honesty
The report on avoidable harm in maternity services at East Kent has now been published.
There is of course a terrible sense of déjà vu. Not just because it follows hard on the heels of the Shrewsbury and Telford report, nor because it is authored by Bill Kirkup, who led the Morecambe Bay investigation.
The déjà vu also comes from the litany of avoidance and denial that we have heard so many times before - at Mid Staffs and Southern Health and Gosport and Cwm Taf and beyond. Bereaved families have had yet again to fight for justice in the teeth of a healthcare provider determined to resist them.
But there is, this time, a vitally important difference. Kirkup says 'It is too late to pretend that this is just another one-off, isolated failure, a freak event that will never happen again'. There is, he says, a pattern.
Back in 2020, we made exactly this point in our Inadmissible Evidence report. We said 'There are no bad apples'.
Our point was that dysfunctional organisational cultures do not arise in isolation. It is not enough to set up inquiry after inquiry, looking at culpable organisations one after another. And it is not enough to say that we will 'learn from mistakes' when we see over and over again that the undermining and gaslighting of bereaved relatives is not mistaken, but intentional.
At the heart of the pattern of malfeasance is a problem summed up by Kirkup as follows:
'The default response of almost every organisation subject to public scrutiny or criticism is to think first of managing its reputation... the experience of many NHS organisational failures shows that it is the whole basis of the response in many cases. Further, it has clearly led to denial, deflection, concealment and aggressive responses to challenge... Not only does this prevent learning and improvement, it is no way to treat families, who are heartlessly denied the truth about what has happened when something has obviously gone wrong'.
Brilliantly, Kirkup refuses to add to the mountain of recommendations that have come out of previous inquiries and investigations. Why not? Because 'The answer cannot be to hope that... multiple recommendations prevent recurrences elsewhere. If that approach were the right one, it would have worked by now. It hasn’t.'
Instead, he points to four areas for action, one of which is 'responding to challenge with honesty'. That, surely, is not too much to ask. But, says Kirkup, 'if we are to break the cycle of endlessly repeating supposedly one-off catastrophic failures', it is essential.
Tuesday October 18th 2022
What the government should know
It might seem like an age ago, but it was only on the 6th September that Liz Truss was confirmed as the UK’s new Prime Minister. With commendable speed, the Health Foundation then published this briefing on what the new government should know.
The briefing is based on rigorous public polling, and the Health Foundation’s message is that 'As the new prime minister sets out her agenda for government, understanding what the public thinks should inform policy'.
So what does the public think? Key findings include the following:
- People are pessimistic about the state of the NHS. Most (55%) think the general standard of care has got worse in the past 12 months, and less than half (43%) think the NHS is providing a good service nationally.
- Just 13% think the government has the right policies for the NHS. Priorities, for the general public, are reducing waiting times for routine hospital treatment and expanding and supporting the workforce - even if it means extra public spending.
- People want a better health service, not a different health system. 77% believe the NHS is crucial to British society, and 71% think greater government investment in the NHS is necessary.
- A minority believe the government is effectively addressing the leading risk factors for ill health. Fewer than 1 in 5 people believe the government is working effectively to improve physical activity (19%), improve diets (17%), reduce alcohol-related harm (16%) and reduce obesity (14%)
The authors remind us that 'Liz Truss promised Conservative party members that she will cut taxes and shrink the state'. In what now seems like a masterpiece of understatement, they go on to say that 'It is hard to see how the new prime minister can reconcile these commitments with addressing the public’s concerns'. Finally, they say 'Failing to do so risks leaving the government out of step with the public as we head towards the next general election'.
Tuesday October 11th 2022
Barnsley chops and baby talk
Patient experience is all about how people feel treated. Not just in terms of their medical treatment and clinical outcomes, but in how they feel treated as human beings.
That is why NHS strategies repeatedly talk about 'respect and dignity' and why patient experience surveys also ask about those two important aspects of care.
In the latest edition of our quarterly magazine, Mark Gamsu looks at the South Yorkshire Integrated Care Board’s 'Start with people' strategy. It features a prominent photo of Mark’s local butcher who, it turns out, was completely unaware that his image was being used to promote good practice in involvement.
Mark wonders whether the picture (along with others in the document) was used to provide 'local colour' rather than as a way of respecting the views of the people of South Yorkshire.
Our other contributor, Bettina Ryll, argues for a more respectful way of communicating with people about their illnesses. Medical language is complicated, and there can be a temptation to simplify. But perhaps we should treat patients as adults, with a desire and capacity to learn. Feeding them baby language can create confusion and anxiety and is, perhaps, disrespectful.
We - the Patient Experience Library - continue to do what we can to help people make sense of the complicated world of patient experience and engagement. As always, we have been picking through some of the latest and best patient experience research, and summarising it through the rest of this magazine. And we’re always keen to hear from our readers, so if you know of a standout report that we should be featuring, or if you want to submit a comment piece, get in touch!
Tuesday October 4th 2022
If you agree, you’re in
A common debate in patient and public involvement (PPI) concerns the "representativeness" of public contributors. They can get caught in a "paradox of representation" in which they are seen as either too naïve to meaningfully contribute, or too knowledgeable to represent "the average patient".
This can be seen as a form of 'boundary defence' in which professionals (in research or quality improvement) resist the encroachment of 'lay people' into their territory.
The authors of this study point to an area of neglect in this debate, which is 'the absence of the voice of contributors themselves'. They say that 'Critiques of representation in PPI have largely been written by researchers - and tend to favour their perspectives as opposed to those of public contributors'.
The study looked at how representation is discussed and conceptualised. It found an underlying 'confirmation logic'. The starting point is that 'when contributor input provides confirmation of researcher work, it is drawn upon as representative of ‘the’ patient experience and not contested in terms of representation'.
When, on the other hand, contributor input seeks to change or debate researcher work, 'representation is drawn upon to dismiss input'. Through this logic, say the authors, 'only confirmation of the researcher's perspective is possible'.
The point here is that judgements about the supposed representativeness of patients are not just a matter of how naïve or knowledgeable they are. It also depends on whether they are confirming or contesting professionals’ views. The paper states that 'Problematically, contributors are representative as long as they agree'.
The study concludes that 'relative expertise is not the deciding factor in whether representation is critiqued or not. Instead, the driver behind this appears to be the confirmation logic, whereby representation is assumed or revoked by researchers based on whether their own decisions are supported or critiqued'.
Exposing tensions like this is, according to the authors, 'essential to move beyond misleading debates about representation'. And, they say, 'Involving contributors themselves in these debates is both a necessity for making progress and, we suggest, an ethical responsibility'.
Tuesday September 27th 2022
Rights in care
We have observed before now that 'patient experience' is not simply a matter of 'satisfaction with services'. Sometimes it is a matter of human rights.
This report from the House of Commons and House of Lords Joint Committee on Human Rights makes the point with some force.
It starts by noting that the UK government is bound by domestic and international obligations to ensure that people in care settings have access to the highest attainable standard of health, and protection against inhuman or degrading treatment. However, it says that 'too often these standards are not met, and individuals suffer'.
One example is 'Do Not Attempt Cardio-Pulmonary Resuscitation' notices (DNACPR). The committee states that 'During the pandemic we were hugely concerned to hear that these were being applied to care users without their knowledge, in a blanket fashion, contrary to the right to life'.
The report highlights 'ongoing issues" with Deprivation of Liberty Safeguards (DoLS) - a system that is meant to ensure that detention in care settings does not involve inhuman or degrading treatment. It says that 'There are often unacceptable delays in authorisation of DoLS and there is often no access to legal aid if care users wish to challenge their deprivation of liberty'. And although the DoLS system is meant to be replaced by a new Liberty Protection Safeguards System, there is no timetable for this to be rolled out.
A further concern is visiting arrangements for those in care settings during the pandemic, and 'the harm caused by blanket bans on visiting'.
The report makes various recommendations, including that:
- Training on human rights must be given by all registered providers to their staff.
- Government should work with stakeholders to raise awareness about the appropriate use of DNACPR notices.
- Government should set a timetable for rollout of the Liberty Protection Safeguards System.
- Government should introduce legislation to give care users the right to nominate one or more individuals to visit and to provide support or care.
Beyond this, the committee calls for privately funded care users to have the same legally enforceable rights as publicly funded users, and for the complaints system to be simplified.
Wednesday September 21st 2022
The feedback safety valve
The imminent publication of the Kirkup investigation into harms at East Kent, and the launch of the Ockenden review of harms at Nottingham are reminders, yet again, of the fact that 'patient voice' is a crucial component of healthcare safety.
The difficulty, however, is that large scale harm tends to come to light far too late - sometimes only after years of campaigning by patients and bereaved relatives.
This paper looks at the potential for patient feedback to be a proactive force for good. The authors propose online patient feedback as a kind of safety valve - 'especially valuable for monitoring unnoticed and unresolved safety incidents'.
But why would safety incidents go unnoticed and unresolved? The paper suggests three reasons:
- Healthcare staff have difficult-to-monitor 'blindspots' such as problems in patients accessing care, errors in clinical notes, errors in post-care planning, and miscommunication issues.
- Organisational culture can allow defensiveness, low safety standards, and concealing errors due to fear of consequences.
- Where healthcare staff do not believe safety reporting systems are effective, prioritised, or drivers of change, they are less likely to use them.
Patients, on the other hand, can more easily see the blindspots because they are directly affected by them - they have a greater 'proximity to error'. They are also independent of organisational culture, so 'may report on incidents that staff overlook or are reluctant to report'. Finally, if mainstream reporting systems (eg formal complaints) seem ineffective, online platforms can 'provide patients and families with a forum to make public incidents they believe have been dismissed or otherwise 'unresolved' within hospitals'.
The study conducted a retrospective analysis of online patient feedback for all acute NHS Trusts in England for the years 2013-2019. This amounted to 146,685 individual items of feedback pertaining to 134 acute English NHS Trusts over 7 years. The key findings were:
- Online patient feedback can provide information on unnoticed and unresolved safety incidents within hospitals, with these data being independent of staff-reported incidents and predictive of patient safety outcomes.
- Over a quarter of high-scoring feedback was related to patients and families reporting safety concerns that, from their perspective, had been dismissed, or asking safety questions that should have been addressed by hospital staff.
- The automated measure of patient-reported safety incidents was associated with hospital mortality, whereas staff-reported incidents were not.
The combined result could be that online patient feedback can function as a safety valve, revealing hospitals that are poor at detecting and responding to safety incidents. The authors make the point that 'neither staff nor patients have complete information, each group has unique insights and blindspots, and thus combining their perspectives is beneficial'.
They conclude that 'Augmenting staff reports with patient reports may be especially valuable when there is uncertainty about staff reporting. In such contexts patients reporting freely online (e.g., anonymously, without consequence) may act as a safety valve, revealing safety incidents that have been unnoticed or unresolved'.
Tuesday September 13th 2022
Patient Experience in England
It is now six years since we began producing our annual overview of patient experience evidence, and we never cease to be impressed by the quality and quantity of published research.
The national patient surveys are produced with a commendable rigour in both the evidence gathering and the analysis. Their findings are always illuminating, and as the years pass, the trends and patterns in patient experience become clearer.
The research studies, by patient voice organisations, health charities, academic institutions and policy think tanks, show a variety of approaches. Formal research is grounded in theory, and quality assured through clarity of method and peer review. Other evidence gathering is less formal, but is based on long-term relationship building in local communities, leading to trusted dialogue and deep insight.
Put together, all of these sources and methods create a rich source of knowledge for an NHS that wants to be both person-centred and evidence based.
But challenges remain.
The last year has seen publication of avoidable harm investigations from the Ockenden review and, in Northern Ireland, the Independent Neurology Inquiry. Both, yet again, reveal a reluctance to take patient feedback seriously, with terrible consequences.
We can tackle this - indeed many people already are, as evidenced by the wealth of ingenuity and effort that has gone into the work featured in this report. The part the Patient Experience Library plays is to help people find their way through the mountain of feedback. Here, once again, we present our top picks from the last twelve months of evidence gathering, with summaries of the key points to help you make sense of it and, we hope, to encourage you to dig deeper.
As always, we are driven by Baroness Cumberlege’s demand that patient experience must 'no longer be considered anecdotal and weighted least in the hierarchy of evidence-based medicine'
Tuesday September 6th 2022
What actually is person-centred care?
'A great deal of ink has been spilt over person-centred care', says this paper - 'a bewildering array of definitions, interpretations, and operationalised accounts exist'. The authors add that 'it is no small irony that many researchers lamenting the absence of a clear definition themselves offer new models and definitions... thus adding to the already crowded conceptual space'.
The problem perhaps starts with terminology. The paper notes that the term ‘person-centred’ is not definitive - it 'sits alongside and overlaps with other terms, including ‘patient-centred,’ ‘people-centred,’ and ‘personalised’'.
There have been many attempts to define person-centredness. The authors point to a series of studies, among which are definitions of the 'Seven dimensions of person-centred care', the 'Four Interactive Components of the Patient-Centred Clinical Method', the 'Five person-centred processes' and the 'Four principles of person-centred care'.
The result of this plethora of conceptual frameworks is that the scope of person-centred care is unclear, the dimensions of person-centred care are ambiguous, and the distinctions between different dimensions are uncertain. Beyond this, 'it is unclear whether person-centred care is best understood to describe a process or the end state of a process'.
In spite of all this, the authors do not dismiss the idea of trying to define person-centred care. 'There are', they say, 'good reasons to give the idea of person-centredness some definite shape and to indicate and illustrate what it means in certain contexts... [this] can help both to critique practice and... provide evaluative frameworks and measures to compare, monitor, and measure healthcare that aspires to be person-centred'.
At the same time, they welcome vagueness and variability. 'Central to person-centred care is a critical, questioning, reflective attitude... Maintaining both vagueness and variety in person-centred care is an essential part of... this reflective attitude, because it enables and upholds its responsiveness to particular people and circumstances'.
'Vagueness' and 'responsiveness' go hand in hand, because 'To adopt a fixed definition is to pre-judge in some sense what is required by particular patients and healthcare contexts, which is liable to impede the enactment and achievement of person-centred care'.
The paper recognises that 'vagueness and variety' might not sit well with the biomedical model of healthcare, on which, for example, clinical guidelines are based. It states that the pursuit of person-centred care might involve 'uncomfortable and costly compromises' even if 'this is not often recognised in the policy documents which largely commend person-centred care as an unqualified good'.
The authors conclude that 'Person-centred care challenges us to think again about what medicine is for and, on more radical interpretations, can recentre and destabilise established medical practices and frameworks'.
Wednesday August 31st 2022
Getting it wrong?
'Randomised trials are conducted to provide evidence to support better and more informed decisions about medicine' says this paper.
Generally, around 70% of trial data relates to outcomes. However, say the authors, 'Not all outcomes are created equal'. Trial teams (researchers), patients and healthcare professionals can all have different ideas about what matters most. But it tends to be trial teams who decide what is to be designated as the 'primary' outcome.
This designation matters because the primary outcome generally drives the size of the trial, and judgements as to whether the trial intervention is effective. Other outcomes are, by definition, less important.
The study showed a series of published trials relating to breast cancer and kidney disease to patients with lived experience of those conditions, and to healthcare professionals with relevant expertise. The question was whether their view of what was most important in each trial matched the trial teams’ own choice of primary outcome.
The answer was that in just 28% of cases, patients and healthcare professionals agreed with trial teams. 'Given that so much hinges on the primary outcome', says the paper, 'even our small study should give some pause'. It goes on to say that in the collective view of patients and professionals, 'trial teams got the choice of primary outcome wrong more often than they got it right'.
The authors discuss the implications. 'Making a mistake in the choice of primary outcome', they say, 'could mean that the trial is too small to say something meaningful about what really matters to patients and healthcare professionals, or the trial could be bigger than it needs to be. The trial might say nothing at all about what matters most'.
Reflecting further, they state that 'The kindest thing that can be said about this is that it represents research waste. Less kindly, it means patients and healthcare staff have spent their time, energy, goodwill and perhaps hope on a trial that has failed to provide the key information that people like them need in order to make better treatment decisions'.
'The solution', they conclude, 'is not difficult: ask people with lived experience of an illness or condition, and their healthcare professionals, what they want to know most'.
Their prescription is not limited to trial teams: 'Funders, ethics committees and others involved in study approval have a role to play too. All should be asking to see researchers’ rationale for the choice of primary and other outcomes to ensure that the choices made are the right ones'.
Tuesday August 23rd 2022
Compassionate communication
NHS waiting lists are growing across the board, with longstanding problems massively exacerbated by the Covid pandemic. This paper describes how one hospital Trust reduced the waiting list of a paediatric service from 1109 to 212. Waiting times were reduced from a maximum of 36 months to a 70-day average.
The first part of the improvement process tackled administrative inefficiencies. Workplace observation found that clinicians lacked time to verify and cleanse waiting list data, so the primary target list of patients was not up to date and it was hard to know who was waiting for an appointment and who had been discharged.
Another problem was the need to gather various reports - school reports, speech and language therapy (SaLT) reports and opt-in/consent forms - in order to progress patients to assessment and treatment. Bottlenecks were arising because 'Too many people were involved in chasing too many reports and too much valuable clinician time was being used on clerical tasks'.
Cleansing the data, improving ways to verify reports, and confirming discharge status resulted in a reduction of the primary target list from 1109 to 556 children.
Alongside administrative improvements, the team took a 'compassionate communication' approach to dealing with patients. This has three components: acknowledging the suffering of another person; expressing caring, kindness and understanding; and withholding judgement. It also requires action: compassionate communication is seen as an active process that puts the needs of others first.
The existing system had failed to do this for patients. As one staff member said, 'A lot of people just don’t want to do the data cleansing - a lot of these children then don’t get diagnosed and they get forgotten about in the system... What if that was my child?'
There was a similar problem with SaLT reports, which could only be actioned once patients or carers had responded to a letter inviting them to submit a formal opt-in. Many patients/carers had been unaware of this, and assumed delays were due to COVID-19. The compassionate communication approach introduced follow-up calls to check that patients had received the invitation letter, and whether they wanted to opt in. Improved flow to clinical assessment panels got the waiting list down to 212, with average waiting times reduced from 421 days to 70.
The approach acknowledged the situation of 'children and their parents stuck in a system of disconnected processes'. Importantly, it also acknowledged 'burden and stress on both administrative and clinical staff'. One comment was that 'I’ve seen the personal impact this has... streamlining the process, removing the waste, having people focused specifically on their job role, and how much that has actually benefited and added value to [them] emotionally'.
The authors state that 'Compassionate interactions between staff and patients are necessary to operate responsive, inclusive processes'. Their view is that 'If compassionate leaders can reframe [quality improvement] from ‘eliminating waste’ and ‘increasing productivity’ to ‘unburdening staff to deliver high quality care’, perhaps this potential can be realised more broadly across the NHS'.
Tuesday August 16th 2022
Creative Engagement
This paper states that 'Consumers are a crucial source of healthcare knowledge and solutions', and their participation in decision-making contributes to the 'political legitimacy' of healthcare systems. In spite of this, 'the international literature suggests that the participation of consumers and the broader community in COVID‐19 responses was very limited. In the urgent rush to respond to outbreaks, healthcare services tended to rely on biomedical and bureaucrat‐controlled approaches with limited community involvement'.
Consumers commonly saw the health service response to Covid-19 as 'command and control', with most services halting their consumer engagement activities, and introducing significant policy and service design decisions without consumer representatives. One example was the management of family visits in healthcare facilities, with visitors seen as an infection risk, leading to blanket bans on nonpatients entering facilities.
This 'resulted in poorer patient experiences', according to the authors. 'Without family visitors, backgrounding patient information... was less comprehensive; discharge home was less informed and co‐ordinated; and patients suffered poorer mental and emotional health.'
As some consumer representatives 'lamented the almost overnight reversal of decades of improvement of consumer participation', others started to rethink their role and purpose. One group set up an online forum, organised workshop sessions, and collected feedback and experiences via Care Opinion. Others developed community‐led initiatives to support socially isolated older people, campaigned to include birth partners for labouring women, and got a Covid testing site moved to a location that was safer for people and traffic.
The collaborative approach required consumer representatives to adapt to working with each other. Until then, most were unknown to each other, having predominantly attended meetings with health services alone and disconnected from one another. The pandemic was seen as a 'circuit breaker' that 'forced them to be creative in rethinking and resetting their ways of operating'.
The authors conclude that 'The response to the COVID‐19 pandemic made visible the brittle nature of previous engagement processes'. However, they say, 'the momentum for proactive self‐organization in an unexpected crisis created space for consumer representatives to reset and reimagine their role as active partners in health services'.
This matters, they say, because consumers’ 'ability to adapt and adjust ways of working are key assets for a resilient health system'.
Tuesday August 2nd 2022
Learn from this
This report covers the events which led to the largest ever recall of patients within Northern Ireland’s healthcare system. Over 5,000 people were subject to potential misdiagnosis, mistreatment and avoidable harm at the hands of neurologist Dr. Michael Watt.
Failures outlined by the inquiry report include:
- Definitive diagnoses being given in the absence of objective imaging.
- Using treatment procedures in a manner which was outside the guidelines.
- The prescription of treatment in grey area cases to the point where, for many years, Dr Watt was an obvious outlier.
- A willingness to circumvent established procedures for transfer between the independent sector and the NHS.
The case has uncomfortable echoes of the inquiry into the rogue breast surgeon (now jailed) Ian Paterson. Except that like Paterson, Dr. Watt was not 'rogue'. He was acting in plain sight, not least because patients were reporting their concerns.
The report makes the point that 'The failure to learn from complaints was one of the more disturbing aspects of the investigation conducted by this Inquiry. Time after time, information was raised in a patient complaint, which needed to be independently investigated. Consistently the answer given to the complainant was obtuse and unhelpful'.
Here we see parallels with the Shrewsbury and Telford investigation, where Donna Ockenden commented that 'So many families have explained to me that for more than two decades they have tried to raise concerns but were brushed aside, ignored and not listened to'.
Another case of déjà vu comes from this comment: 'Generally, the inability of the systems then in place to identify a pattern of concern was a conspicuous problem. Information was essentially retained in silos'. This is exactly the point that Baroness Cumberlege raised in her First Do No Harm report on valproate, Primodos and mesh: 'the healthcare system...is disjointed, siloed, unresponsive...'.
A further, depressingly familiar observation is that 'there was no consistent method of dealing with clinical complaints and the emphasis remains on timely resolution... the approach was focused on responding within stipulated time periods and ‘resolving’ complaints'. The result was that 'the opportunity for learning from complaints often seems to have been missed'.
The Inquiry Panel says that it was 'struck by the determination of the patients of Dr Watt to ensure that issues were properly investigated and that lessons will be learned from this Inquiry'.
It says that 'when patients describe issues that may reflect a lack of safety, they must be heard, and appropriate action initiated'. But it also states that 'Patients are not, and cannot be, responsible for the safety of the health system. That sits with those responsible for governing the system'.
Tuesday July 26th 2022
Emergency waits: transparency please
'Emergency Department [ED] crowding is one of the most serious policy challenges facing the NHS' says this report from the Royal College of Emergency Medicine (RCEM).
It goes on to say that 'crowding is not only dangerous, but also inhumane and undignified for patients who have no option but to stay for treatment in precarious conditions'.
The report concentrates on a key measure: the numbers of patients waiting 12 hours or more beyond a decision to admit (DTA). It describes the numbers as 'staggering' and says that in the first four months of 2022 alone there were more than 79,000 12-hour DTA waits; nearly as many as the cumulative total of the 11 years since data collection began (83,000 12-hour DTA waits from August 2010 to December 2021).
In any case, says the RCEM, the 12 hour DTA measure 'does not capture the true extent of the delays experienced by the patient'. A better measure, they say, would be 12 hours from time of arrival (TOA). This tracks performance 'from the moment the patient steps foot into the ED' and would be 'a clear, patient centred measure, which brings performance measurement in England in line with the rest of the devolved nations'.
The report makes the point that 'While hospitals currently have access to their own performance data, the Government and NHS England have still not indicated when the data on 12 hours TOA will be publicly available'.
Publishing these figures matters because 'Behind every single metric is a patient and the NHS is failing its commitment to provide care to the public without any unnecessary delay; a key pledge outlined in the NHS Constitution'.
'This data', says the RCEM, 'must be published immediately'.
Tuesday July 19th 2022
Eliminating out of area placements
'The lack of capacity within the mental health system is well established', says this report from the Royal College of Psychiatrists (RCP). It adds that 'services all over the country are struggling to meet demand'.
One consequence is inappropriate out of area placements, where a patient is admitted to an inpatient unit far from home because no appropriate bed is available locally.
Inappropriate out of area placements 'were always intended to be the absolute last resort'. However, 'NHS data shows that inappropriate out of area placements are still heavily relied on to manage pressure on the system'.
The report says that 'Patients... have been left paying the price. Sometimes hundreds of miles away from home, they are unable to access their usual support networks while at their most vulnerable, often finding their care seriously disrupted with long term implications for their recovery.'
The RCP recognises NHS Long Term Plan commitments to tackle the problem. But, it says, 'The government’s deadline to eliminate inappropriate out of area placements... by the end of March 2021 has now been missed by a full year'. And in March 2022, 'over half of all inappropriate out of area placements saw patients travel more than 100km from home because a local bed was unavailable for the eighth month running'.
The report makes a series of recommendations, taking in staffing, improved therapies and the condition of the mental health estate. But with increased demand on mental health services as a result of the pandemic, there is a sense of urgency. 'Systems must be put in place that bridge the gap between the current status quo and the full delivery of the Long Term Plan, to ensure that all patients requiring intense treatment and support receive the best possible standard of care'.
Ultimately, the RCP’s position is clear: 'This situation is unacceptable, and patients experiencing an acute mental health crisis can’t afford to wait any longer'.
Tuesday July 12th 2022
Do complaints improve quality?
'Most patients and families submit complaints to prevent harm from occurring to others' says this paper. And from the provider perspective, complaints 'are increasingly recognised as a critical source of insight for quality improvement'.
But does complaints handling actually lead to improvement? This study considered how national policies shaped practice in one English Trust, and looked for any discrepancies between policies-as-intended and their reality in local practice.
It found four areas where 'the design of national rules and policies functioned to undermine a patient-centric and improvement-focused approach to complaints'. These were as follows:
- Muddled routes. The paper cites a 'confusing landscape of routes for raising concerns' and confusion over the role of PALS (Patient Advice and Liaison Service) as against the complaints team.
- Asymmetry. Investigative procedures at the Trust were 'predominantly structured to judge the ‘well-foundedness’ of complaints'. Internal evidence was regarded as superior, reflecting 'a persistent belief that complaints are subjective and subordinate to clinical perspectives and hospital data'.
- False information. Complaints administrators considered the KO41a official complaints data collection system to be inappropriate, with one describing it as supplying 'false information'.
- Adverse incentives. Performance targets for complaint handling led to pressure not to exceed response timelines set out by national policy. This could create adverse incentives such as a focus on reducing complaints volumes.
The authors emphasise that procedural problems like these are not necessarily 'a consequence of sinister or malign organisational actors seeking to impose silence'. Instead, they can be seen as case of 'well-intentioned staff confined by an overly formalised and bureaucratic system'.
The paper finishes with recommendations for change, including patient involvement in complaints investigations, the establishment of independent investigation bodies, and more meaningful data analysis.
Monday July 4th 2022
Computer says…?
Patient experience is often thought of as a kind of 'customer satisfaction' exercise. An obvious example is the NHS Friends and Family Test, which is described as a way to help service providers and commissioners understand whether patients are happy with the service provided.
But patient experience is also about human rights. And in this edition of our quarterly magazine, we hear about something very fundamental: the right of patients to maintain their closest personal relationships and be supported by someone who loves them.
In the crisis period of the pandemic, that basic human need was sometimes forgotten, with compassion and person-centredness being overtaken by a 'computer says no' mentality. Julia Jones, co-founder of John’s Campaign, describes how she is now winning support from MPs for a change to the law.
A third aspect of patient experience is the experience of self managing a long term health condition. Ceinwen Giles shows how that is not just about understanding medications and self-care. It is also about weaving your way through the tangles of health service administration, where again, too many computers say 'no'. Her tale might have you laughing or crying, or both.
As always, the magazine features some of the latest and best patient experience research, published over the last few months. The events page has some excellent forthcoming courses and conferences. And the magazine is distributed free of charge - so feel free to share as widely as you like!
Tuesday June 28th 2022
Dementia disproportionate for women
Dementia has been the leading cause of death for women in the UK for over a decade. Nearly two thirds of the UK citizens living with dementia are women. And the lifetime risk of developing dementia is one in five for women, against one in ten for men.
Even so, says this report, 'it is still not fully understood why dementia is more prevalent in women'.
One possible reason is that low levels of physical activity can be a contributory factor, and women in the UK have one of the lowest physical activity rates in the world. Another risk factor is loneliness, and almost double the number of women over 70 live alone compared to men.
Alongside individual lifestyle issues are more systemic problems.
One example is that the UK has the largest difference in male and female healthcare experiences in the G20 countries, with women receiving worse healthcare than men. To compound the problem, women with dementia receive less health monitoring and fewer GP visits than men.
Another is that women experience drug effects differently from men, with higher risks of negative side effects. But 72% of randomised controlled trials do not report sex-specific outcomes. Moreover, female volunteers for dementia research studies are likely to be excluded because of old age and multiple health conditions.
The disproportionate effect of dementia on women extends to the fact that around two thirds of unpaid carers of people with dementia are women. More than one million unpaid carers live in poverty in the UK, and 81% experience isolation, depression and anxiety. These are all contributory factors for cognitive decline.
The report makes three recommendations:
The UK government’s Dementia and Women’s Health strategies should recognise the disproportionate effect of dementia on women.
Regulators and funders should set out expectations for reducing the gender gap in clinical trials.
Research organisations should have plans to 'break the bias' and demonstrate that female researchers can participate on an equal basis with male researchers.
Tuesday June 21st 2022
Invisible illness and citizen science
This study is unique, say the authors, in being the first citizen science qualitative study in the UK. Both the data and the analysis have been driven by an online patient community.
The community in question comes from the 1.5 million UK residents living with self-reported Long Covid. Although recognised as a condition by the National Institute for Health and Care Excellence (NICE), Long Covid symptoms are 'poorly explained by objective medical tests'.
The study notes that 'Without objective indicators... Long Covid patients rely on having their illness testimonies believed and taken seriously to access treatment and support'. But in an era of evidence-based practice, this can make them vulnerable to 'epistemic injustice', whereby they are seen as 'unreliable informants of their own illness experiences'.
The study revealed three themes in people’s experiences of Long Covid:
- Life changing: People with previously fit and active lifestyles facing the end of normality, rollercoaster symptoms and uncertainty and fear.
- Validation: Patients with confirmed or suspected Covid-19 feeling that they were not always heard or believed.
- Seeking alternatives: A desire to seek alternatives to formal healthcare, including online support groups, self-help and exercise.
Running through all of this is the gap between lived experience and medical science. In common with other 'invisible illnesses' such as fibromyalgia, endometriosis, depression, chronic pain and depression, Long Covid patients found that clinicians 'did not recognise their condition, did not believe that it existed, did not know how to diagnose it, did not empathise or acknowledge their suffering, [and] did not know how to manage it'.
Addressing this gap must, say the authors, 'be a priority as guidelines for complex, chronic illnesses like ME and Long Covid require a compassionate and empathic patient‐centred approach fundamental to which are advanced communication and interpersonal skills'.
Tuesday June 14th 2022
Women’s health in prison
'Prisons are not healthy environments. They are unable to address the physical and mental health needs of women and in fact exacerbate them.'
This frank assessment comes from the All Party Parliamentary Group (APPG) on Women in the Penal System. Their report pulls no punches in its analysis of health-related harm in women’s prisons.
Contributory factors include the following:
- Imprisonment compounds the victimisation of women, the majority of whom have experienced violence or abuse prior to prison.
- The prison system as a whole is designed around the needs of a male majority. Prison rules and prison policy neither support nor prioritise women’s health and well-being.
- Most women in prison do not need to be there. Over half are on remand and a third are serving short sentences.
- The prison environment exacerbates health inequalities for Black and minority ethnic women.
- The lack of continuity for women coming in and going out of prison is detrimental to their care.
These issues, and others, are summarised in this concise and compelling document, which finishes by considering the government’s Prisons Strategy White Paper.
It finds that 'The white paper rightly recognises that women in the criminal justice system have complex needs'. However, it says, 'the proposals will lead to an expansion of the prison estate, resulting in more women and children experiencing the harms of prison when it is not necessary or appropriate'. Instead, 'The focus should be on reducing the unnecessary use of prison for women and on improving and expanding provision for women in the community'.
The APPG concludes that the white paper is 'a missed opportunity to address the needs of women in the criminal justice system and to reduce the harm caused by imprisonment'.
Tuesday June 7th 2022
Woman-centred care?
The UK debate about the quality of maternity care rumbles on, fuelled by the investigations at Shrewsbury & Telford, East Kent and Nottingham. But similar debates are happening elsewhere, and this paper usefully compares strategic responses from different countries around the world.
The starting point is the mixed reaction to Australia's 2019 "Woman-centred care" strategy, which set the direction for the country's maternity services. Following the release, "disappointment and frustration was voiced by consumers and maternity service providers (especially midwives) due to the minimal incorporation of midwifery continuity of care and out of hospital birth place options".
To try to understand the reaction, the authors of this paper compared the Australian plan with maternity strategies from England, Wales, Scotland, Ireland, Northern Ireland, Canada, and New Zealand. The analysis concentrates on the Australian healthcare system, but it also includes some wider insights into maternity politics, culture and strategy. These include the following:
In the Australian strategy, the term "woman-centred" encompassed the values of safety, respect, choice, and access. The essence of these values appeared in every other plan reviewed.
Continuity of midwifery carer appeared to be an add-on to the Australian strategy, following substantial consumer protests. It stands at odds in this respect with the English, Scottish, and Welsh plans, which advocate for continuity of midwifery care for all women.
There was significant variation in the positioning and professional autonomy of midwifery in the reviewed plans and guidelines. However, where the midwifery profession is strong, midwifery models of care and place of birth options were more likely to be discussed and recommended.
In countries where birth at home and in birth centres is widely accepted, the recommendations in maternity plans were more in line with evidence, human rights, and consumer demands.
There were inconsistencies in all the documents reviewed around where the final decision making lay when it came to choice and autonomy in maternity care. This is in spite of the fact that the right of people to make autonomous decisions about their own bodies is enshrined in the Universal Declaration on Human Rights and applies, without exception, to pregnant and birthing women. This, say the authors, "leaves women in a vulnerable position when it comes to choice and autonomy in nearly every strategy/plan we reviewed".
The authors conclude that "In countries with an established, valued and autonomous midwifery profession, maternity guidelines appear to better align with evidence". Their suggestion is that "Priority must be given to the choices women make and the best available evidence, not the power and interests of organisations and individuals".
Tuesday May 31st 2022
Involvement and innovation in digital healthcare
"The COVID-19 pandemic arguably led to an unprecedented increase in both the innovation and the implementation of digital health technologies", says this paper. However, "this was often at the expense of meaningful involvement".
The study, conducted by Plymouth University with support from the Patient Experience Library, looked at patient and public involvement (PPI) in digital health innovation, aiming to identify factors that enable or inhibit meaningful involvement.
Its starting point was that "despite a strong policy rhetoric supported by national agendas such as the UK Long Term Plan and the Digital First Strategy, the extent to which patients and the public are involved in digital health innovations... remains largely unknown". This matters because "evidence‐based guidance on how to carry out meaningful PPI in the rapidly evolving field of digital health is lacking".
The study found that published articles on PPI in digital healthcare reported multiple benefits, including improved useability; insight into patients' needs and preferences and increased credibility and likelihood of app recommendation and use.
In spite of this, there were also many barriers to meaningful involvement. These included time and financial constraints; involvement not being seen as a priority by stakeholders; not involving patients early enough in the process; and a disconnect between developers and end users. For their part, patients were sometimes reluctant to engage because of fears about data privacy and security.
Enablers for participation included clarity about who has the final design say (patient led vs researcher/designer led); allowing time to account for delays and setbacks; providing a named point of contact; and reimbursing expenses in a timely manner.
To these barriers and enablers is added a further consideration: an unequal distribution of power. This, say the authors, rests on "traditional, often hierarchical ways of working, with patient insights and suggestions often seen as inferior during the innovation and implementation process". A possible solution is "More creative methods that enable patients and innovators to voice their suggestions and ideas in their own words, as opposed to those that have already been defined for them".
The authors conclude that "Some reported barriers and enablers such as the importance of data privacy and security appear to be unique to PPI in digital health". They call for "Multi‐ disciplinary consensus on the principles and practicalities that underpin meaningful PPI in digital health innovation".
Tuesday May 24th 2022
Out of sight - who cares?
The government's programme for the next parliament promises draft legislation to reform the Mental Health Act. The purpose is to give patients suffering from mental health conditions greater control over their treatment and to make it easier for people with learning disabilities and autism to be discharged from hospital.
This report from the Care Quality Commission is clear that both objectives are much needed.
According to the authors, "there are still too many people in mental health inpatient services. They often stay too long, do not experience therapeutic care and are still subject to too many restrictive interventions, which cause trauma. Families have told us clearly that the pain and harm for them and their family member continues".
The reasons for this include a "lack of community services" and the fact that "the right housing is not available, nor the right support in place.... People end up moving around the system from one service to another because their needs are not being met".
This progress report updates the original "Out of Sight" document, published in October 2020. It finds that 13 of the original report's recommendations have not been achieved. Four have been partly achieved. There are no recommendations that have been fully achieved.
Recommendation 10 is about people’s experience of person-centred care. Here we find that "People and their families still tell us that it is not always easy to raise and escalate concerns to providers or commissioners. Where they do, they can feel labelled as difficult or persistent complainers and are concerned that it will have a negative impact on how providers see and treat them or their loved one". Moreover, "Advocacy providers have been concerned about the lack of funding for the provision of advocacy for a long time, and progress has been too slow".
It is now five years since Prime Minister Theresa May described mental illness as a "hidden injustice", and called for "parity of esteem" between mental and physical health services. We can only hope that the government's latest promise brings us closer to that goal.
Tuesday May 17th 2022
Health inequalities: Clearing the fog
"Despite health inequalities being a priority for many countries, the gap in access and quality of healthcare and health outcomes between the most and least disadvantaged groups is widening". So says the opener to this study, which examined healthcare policy documents to see how health inequalities are understood and addressed.
The authors looked at plans published by Sustainability and Transformation Partnerships and Integrated Care Systems. The average length of the plans was 167 pages, and all of them mentioned health inequalities. Five common themes emerged:
- "Vagueness" was exemplified by a lack of detail of the key healthcare and health outcome inequalities within and across different groups. This led to a lack of clear goals to reduce health inequalities.
- "Variation" throughout the documents was demonstrated in three ways: variation in definitions of terms, groups being compared and the use of metrics and indicators.
- "Lack of prior conceptualisation and approach" refers to the way that local healthcare systems appeared not have an established approach or work programme. Documents frequently mentioned gaps in awareness of what inequalities were present.
- "Use of value judgements" was revealed through widespread discussion of lifestyle and behaviour being a major determinant of health, as well as in how certain populations were more frequently included, whilst others were consistently left out.
- "Lack of commitment to action" meant that while there was a high level of commitment to the notion of tackling health inequalities, there was a lack of concrete and accountable targets or actions.
The authors argue that healthcare systems should agree on a coherent national conceptualisation or framework for health inequalities. This needs to go hand in hand with clear guiding principles about how to reduce inequalities. Any such framework should also be part of a partnership between multiple governmental bodies. And, importantly, it should "allow local healthcare systems to prioritise according to their local needs... and contain specified population groups and outcomes measures to focus on".
Tuesday May 10th 2022
Facing up to patient choice
Last autumn, Health Secretary Sajid Javid told MPs it was 'high time' GPs offered in-person appointments to anyone who wants one - claiming life was 'almost back to completely normal'.
The ensuing war of words drew in the British Medical Association, the Royal College of GPs and various sections of the media. But what do patients think?
This study from the Health Foundation looked at 7.5million patient-initiated requests for primary care made using the askmyGP online consultation system at 146 general practices in England. Their findings challenge some basic assumptions about patient preferences.
A key finding was that only a minority of requests at the practices in this study requested a face-to-face consultation. Importantly, this was true even before the pandemic.
Unsurprisingly, Covid then accelerated online requests - from 60% in June 2019 up to 72% during 2021.
Further analysis shows different behaviour across different groups. Men, for example, were over 10% less likely to contact the practice online than women. Patients requesting a response via SMS/online messaging were more than 35 times as likely to use the online channel than those asking for a telephone consultation. And during 2021, patients asking about new medical problems were twice as likely to contact the practice online as those asking about an existing medical problem.
So how many people are looking for face-to-face consultations? The study found that the proportion of requests indicating a preference for face-to-face dipped from an average of 29.7% before the pandemic to less than 4% at the start of the pandemic. It steadily recovered after that but was only at 10% by the end of the study period in September 2021.
In terms of alternatives to face-to-face, telephone consultation was the most popular, favoured on average in 44% of requests pre-pandemic, and by 55% in both 2020 and 2021.
Requests for a response via SMS/online messaging accounted for on average 26% of requests pre-pandemic, rising to over a third in 2020 and 2021.
Fewer than 1% of requests asked for a video consultation.
The authors note that "The October 2021 NHS support plan for improving access for patients and supporting general practice set out a concern that a level of face-to-face care less than 20% may be contrary to good clinical practice".
However, they say that "136 of 146 practices we studied would have been included in this criticism". Consequently, they believe that "simple numerical targets on the use of remote vs face-to-face consultations would be inappropriate, and a more holistic view should be taken".
Wednesday May 4th 2022
Living in a Covid World
Last February - two years on from the start of the pandemic - the UK government announced its plan for living with Covid. The main thrust of it seems to be that vaccines will be the "first line of defence". Other than that, we are all "encouraged" to follow public health advice, "as with all infectious diseases such as the flu".
At the same time, the House of Lords Covid-19 Committee has been taking a somewhat deeper view. Their report recognises that while the crisis stage of the pandemic might be drawing to a close, the longer term impact is "far-reaching, profound and permanent". The authors state that "we must adapt our lives, and world, to the economic, social and health consequences of the pandemic".
The learning points start with an admission: that "our current understanding of resilience and preparedness is not fit-for-purpose". In particular, "a focus on robust supply chains and critical national infrastructure alone will not secure the national resilience that we so desperately need".
For the Committee, social considerations matter just as much as economic necessities. "The pandemic has shown that national level resilience is undermined by financial inequalities and health inequalities, which are often exacerbated by racial injustice. To be resilient, we must have strong social capital and community connection within, and between, diverse communities, higher levels of social and economic equity, and resilient and adaptable public services."
The report calls for "a new resilience agenda", taking in inequality, digital inclusion and public health. This must be tied to systems of government that look beyond short term electoral cycles to longer term challenges such as ageing population, technological change and climate risk. Importantly, "any new system of government must have the wellbeing of its people at its heart".
The Committee proposes a move to a "Wellbeing State", whose purpose would be "to secure the wellbeing of all its citizens, and tackle those inequalities that hold back specific groups and communities".
In a statement that will gladden the hearts of public engagement teams, the report states that "It is only by reaching into every part of our society, and actively engaging with them about the interventions that will improve their wellbeing, that we can improve our resilience". Equally importantly, "We cannot claim to be resilient, until all groups, communities and neighbourhoods are resilient, and continuing vulnerability amongst specific groups, communities and neighbourhoods will make us all vulnerable to the upheavals of the future".
Tuesday April 26th 2022
Communicating better with patients and staff
"At the end of December 2021, 6.07 million patients were waiting for elective care, the biggest waiting list since records began." So says the House of Commons Committee of Public Accounts in the opening sentence of its report on waiting list backlogs.
There is a direct link between waiting times and people's experiences of care, and the report confronts this issue head-on.
It makes the point that "People will face serious health consequences as a result of delays in treatment, with some dying earlier than they otherwise would, and many living with pain or discomfort for longer than they otherwise would". It also states that "Waiting times for elective and cancer treatment are too dependent on where people live and there is no national plan to address this postcode lottery".
The committee is clear that the huge backlogs predate the Covid crisis: "The Department of Health and Social Care (the Department) and NHS England and NHS Improvement (NHSE&I) oversaw declines in waiting time performance for cancer care from 2014 and elective care from 2016 as they did not increase capacity sufficiently to meet growing demand for NHS services". It recognises that "despite the heroic efforts of the NHS workforce", the pandemic has exacerbated "these previous failures".
There is concern about a lack of transparency in how the crisis is being tackled. The report states that "the Department allowed NHS England to be selective about which standards it focused on, reducing accountability". It also says that "the Department and NHSE&I appeared unwilling to make measurable commitments about what new funding for elective recovery would achieve".
The committee finds that "The Department needs to be better at communicating with NHS staff and patients about what the NHS will be able to deliver in the coming years". And it calls for a "transparent and realistic assessment of... how patients will be kept informed about their own progress through waiting lists".
We agree that transparency and accountability are vital, which is why we have made our waiting list tracker available free of charge across all English acute Trusts. We will continue doing so, and once again invite NHS England and the Department for Health and Social Care to work with us on this, and similar initiatives.
Wednesday April 20th 2022
Rebuilding relationships
In the wake of the Ockenden review of maternity harms at Shrewsbury and Telford, Secretary of State Sajid Javid has vowed to "go after" those responsible.
Accountability certainly matters at times like these - but is a tough or punitive approach the most appropriate?
This paper states that "taking responsibility is not the same as accepting culpability" - indeed, "The endurance of retributive approaches to investigations is a barrier to responsibility taking".
As the authors see it, "Safety investigations are increasingly characterized by... the criminalization of human error, despite assurances from safety scientists that individuals are rarely solely culpable". Furthermore, "The adversarial conditions and entrenched positions of lengthy investigations usually prevent opportunities to bring patients, families and health providers together".
This matters because "When an incident occurs... relationships are affected". So "If harm is to be adequately addressed... well-being must be restored, and trust and relationships rebuilt".
The paper advocates a restorative justice approach, based on "active participation, respectful dialogue, truthfulness, accountability, empowerment and equal concern for all the people involved". The aim is to "restore well-being and relationships alongside understanding what happened", so the dialogue is guided by "a concern to address harms, meet needs, restore trust and promote repair".
The authors state that this is "a far more comprehensive and complex response than one which seeks to identify a victim, a perpetrator and a punishment; or indeed, one which simply assumes that system learning is the overwhelming priority". They argue that "It has the potential to result in a meaningful apology because of the focus on essential apology characteristics; respectful dialogue, acknowledgement of responsibility and actions that address justice needs".
Mr. Javid's tough talk might play well with some audiences. But for anyone interested in bringing healing from harm, this paper is worth a read.
Tuesday April 12th 2022
Here be dragons
Medieval maps are a wonderful blend of scientific observation and pure fantasy. Early cartographers did their best to show what the world looked like. But in areas that were too hard to reach, they abandoned facts and relied on imagination instead. Sometimes they gave up altogether and simply left blank spaces - freely acknowledging large gaps in knowledge.
The UK patient experience evidence base is similar. We too have an awareness of people and places that are "hard to reach". But unlike the map makers of old, we not good at openly displaying the gaps in our understanding.
The fact is that nobody has ever mapped the patient experience evidence base. No-one really knows where the strengths and weaknesses are, and that leaves us unable to direct the evidence gathering effort to where it is really needed.
Against this background, we set out to explore. Taking two samples - people's experiences of Covid-19 and people experiences of digital healthcare, we created visualisations, offering insights into the scale and nature of the evidence gathering.
We found that some parts of the evidence base (for example on access to services) were saturated, with studies adding more to the pile of reports than to the sum of knowledge. Other parts (particularly around areas of health inequality) were persistently thin. You can see what we discovered in a short video here.
Our mapping methodology can help researchers to see what is in the existing evidence base before embarking on new studies. It can help funders to see how to get better value for money, by avoiding time-wasting and duplication. And it can help patient advocates to see how and whether different sections of society are represented in patient experience evidence-gathering.
The mapping project - carried out in partnership with Plymouth University - was simply a "proof of concept" exercise, to see if such a thing could even be done. Now that we know it can be, we want to do more.
We could envisage mapping the evidence base by:
- Condition: For example, patient experience of autism, or Parkinson's, or cancer.
- Service type: For example, patient experience of maternity services, taking in labour and birth, perinatal mental health, antenatal education etc.
- Socioeconomic group: For example, end of life experiences for different faiths, the healthcare experiences of homeless people etc.
Finally, our video (as per the link above) allows viewers to see what the maps can do, but does not give them direct access. We would like to improve functionality within the Patient Experience Library so that users could manipulate and interrogate the maps for themselves, democratising the knowledge contained within them.
We'll be approaching national NHS bodies to ask if they'd like to work with us on this. We'll let you know how we get on.
Tuesday April 5th 2022
Patient experience in the spotlight
The Ockenden review of maternity harms at the Shrewsbury and Telford Trust has put patient experience firmly back in the spotlight.
The report must, we hope, offer some consolation to the hundreds of families who have suffered such grievous harm. 'For more than two decades' it says, 'they have tried to raise concerns but were brushed aside, ignored and not listened to".
That will sound familiar to Kath Sansom, one of our contributors to the latest edition of our quarterly magazine. As the founder of the Sling the Mesh campaign, Kath speaks for the thousands of women who spoke out about the harms of pelvic mesh and who, for years, were ignored. She describes continuing government inaction which, she says, 'sends an insidious message to women - to put up and shut up'.
Our other contributor, Sue Robins, has her own stories about life with cancer, life with a son who has Downs Syndrome, and life as a patient advocate. For her, 'health care should be based on relationships, and dare I say, love'. As an activist, her message is clear: 'We don’t have to wait for the CEO to give us permission; we can start now'.
As always, the magazine features some of the latest and best patient experience research, published over the last few months. The events page has some excellent forthcoming courses and conferences. And the magazine is distributed free of charge - so feel free to share as widely as you like!
Tuesday March 29th 2022
Person-centred care: Knowing where to look
This paper begins by casting an eye back over the history of quality measurement in healthcare. It notes that the increased "industrialisation" of health systems brought with it audit and feedback systems whose main purpose was quality control.
But "with the rise in advocacy groups and patient-representative organisations, the... managerialist ideology was challenged". Quality control gave way to quality improvement, accompanied by notions of "person-centred" care.
In spite of this, argues the author, approaches to quality measurement have not changed much. They "continue to privilege standardised, quantifiable data and... Despite more than 30 years of developments in patient-centred and then person-centred care, the focus on quantitative measurement has continued to dominate, even though it does little to inform stakeholders about the person-centredness of a health system".
The paper points out the limitations of Patient-Centred Outcome Measures (PCOMs), which, it says, need to "extend far beyond a narrow perspective of pre-determined indicators of clinical effectiveness".
Widening the perspective means looking at organisational culture - ideally, "a culture that is developed and sustained by person-centred staff and supported by person-centred organisational values and systems". A failure to do so "only serves to ‘blame’ individual staff for not being person-centred in their care practices without recognising organisational responsibilities".
There are "a variety of qualitative methods" that can help to take account of individual experience alongside the measurement of clinical effectiveness. But are qualitative methods taken seriously enough? The author states that "It is always interesting to me that rigour in the use of quantitative data is assumed, while in qualitative methods it has to be defended".
The paper concludes that "We need to respect the integrity of both traditions", given the "urgent need to demonstrate the value of person-centred cultures to health care organisations". And, says the author, "The more we are able to see, the better we get at knowing where to look".
Tuesday March 22nd 2022
Fundamental care and difficult patients
"Missed fundamental care in hospital can have serious consequences", says this paper. It references the Mid Staffordshire inquiry, whose Chair, Sir Robert Francis QC, described apparently minor failures (personal cleansing, dressing, toileting, eating and drinking etc) as the "early warning signs" of what turned into "appalling suffering".
The authors cite other research, indicating that when patient need exceeds labour resources (ie at at time of workforce shortages), medical care tends to be prioritised, with implicit rationing of both emotional support and aspects of 'fundamental care'. In spite of this, "patients can be reluctant to ask for care for fear of being labelled difficult".
The study explored these issues, and found that patients talked about "staying out of trouble" and "not wanting to make a nuisance" or "pester staff". They tended to keep an eye on nursing staff to decide whether and how to ask for help with their fundamental care needs.
Patients' views of staff behaviour fell into three types: "engaged" nurses were seen as genuinely attentive and caring. "Distracted" nurses could be caring but were not generally attentive. "Dismissive" nurses were seen as neither caring nor attentive.
The nurses' work environment seems to have played a part. They were seen as less "engaged" on a ward which had a high number of beds, a high turnover of patients and was undergoing a significant reorganisation during data collection. Staff were more "engaged" on a long stay ward, where patients had existing relationships with many members of staff. Importantly, "dismissive" care was most closely identifiable with aspects of the "Total Institution", where "batch living", standardised routines and institutional efficiency can come to override personalised care.
The consequences for patients are worryingly reminiscent of Mid Staffs. In some cases, "they would wait to make fundamental care requests... waiting until the next shift if necessary". But sometimes "they stopped asking for care because they felt it would not be given".
The study notes that "patients who were most in need of physical support and patients with cognitive impairments experienced serious omissions of care". And it finishes by stating that unless nursing staff can maintain an "engaged" interaction with patients, the idea of "patient involvement in hospital care decisions will remain at the level of rhetoric".
Monday March 14th 2022
Covid inquiry limbers up
It is good to see the launch of a public consultation on the Covid Inquiry's draft terms of reference. The inquiry will make a formal assessment of the government's pandemic preparedness and response.
So now seems a good time to revisit the report of a Covid inquiry that has already taken place. Published in December 2021, the People's Covid Inquiry makes no bones about its conclusions. The title alone: "Misconduct in Public Office" indicates its main thrust.
On preparedeness, some key findings are as follows:
- Austerity policies from 2010 onwards resulted in widening health inequalities. Once Covid struck, there was a "very, very high differential mortality gradient where the most disadvantaged groups have clearly been most vulnerable".
- Contingency planning for emergencies such as pandemics was "stripped out" after 2010, with "local agencies left to make their own arrangements".
- Austerity and marketisation meant that by 2019 the NHS was short of 100,000 staff and had "one of the lowest beds-to-patient population ratios in Europe".
On responsiveness, the inquiry found that:
- For a long period there was no functioning "Find, Test, Trace, Isolate and Support" system. The Government had already abandoned widespread testing by March 2020, due to a lack of capacity.
- Stocks of personal protective equipment (PPE) were "massively run down" before the pandemic. Staff were photographed wearing bin bags and other makeshift items, and this played "a significant role in hospital acquired infection".
- Government messaging was often unclear, confusing, contradictory or just plain wrong. Messaging for minority ethnic groups had been "poor to non-existent".
There is much more in this report - on corrupt contract processes, the experiences of "at risk" groups, human rights issues and more. In spite of all this, the report states that "It is not too late for some good to emerge from the pandemic".
It says that "Lessons are clear, and can and should be learned. With political will and public support, social and health inequalities could be tackled. We could see the NHS and other public services properly funded saved from the brink of collapse. Only in this way can we keep the nation safe and protect it from a repeat of the current catastrophic public health disaster we have documented here".
Monday March 7th 2022
Patient experience makes the cut
An NHS that aims to be both person-centred and evidence-based needs an evidence base for patient experience.
That might seem obvious, but before we set up the Patient Experience Library, no such thing existed. In an NHS amply provided with medical research databases, there was no equivalent for patient experience.
Since launching the library, we have been calling on Health Education England to include it as part of the National Core Content - the suite of research databases made available to all NHS staff because they are deemed essential to underpin evidence-based practice. Within the core content, patient experience has been noticeable by its absence.
So it is hugely encouraging to see that the new NHS Knowledge and Library Hub does, in fact, mention the Patient Experience Library. Granted, we're not actually in the Hub itself. Instead, we're halfway down the "Other" list at the bottom of the Hub's welcome page. But even to get acknowledgement that a patient experience research database exists is a major step forward.
By the same token, we were delighted with the response to our Patient Experience and Engagement symposium last week, co-hosted with Leeds Beckett University.
We had expected a niche audience of around 40-50, and were amazed to see 136 people logging in. Our speakers were excellent, as were the questions and observations posed by the audience. But it was also great to see people using the chat to talk to one another directly - making connections and sharing information.
There is a growing appetite for an evidence-based approach to understanding patient experience. We will be working with Leeds Beckett University and NHS England to build on the ideas and enthusiasm generated at last week's symposium. And we will keep talking with Health Education England about the need for patient experience evidence to be fully integrated within the National Core Content.
In the meantime, we'll keep bringing you handy summaries of the latest and best in patient experience research via this newsletter!
Monday February 28th 2022
Patients or politics?
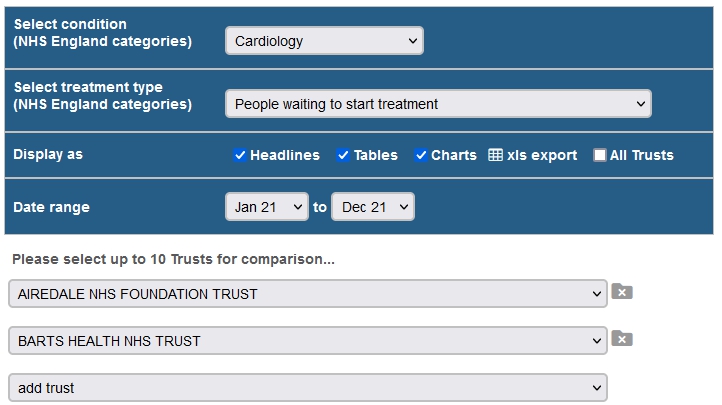
Last week, NHS England launched the My Planned Care platform, a centrepiece of the elective care recovery plan.
One part of the platform will offer support information for patients stuck on lengthy waiting lists. Unfortunately though, that part of the platform is incomplete. (A letter sent to providers has given them until the end of March to submit their support information, but says nothing about what will happen if they miss the deadline.)
The other key part of the platform is a waiting list tracker. Announcing this on the BBC Radio 4 Today programme, Secretary of State Sajid Javid said "For the first time, every patient in England will be able to go on line and see where they are on the waiting list". He said it would offer "a level of transparency that has never been provided before".
Unfortunately My Planned Care does nothing of the sort. All it can offer patients is one rather unhelpful statistic: average waiting times for treatments at local Trusts.
Our own waiting list tracker has been available free of charge across all English acute Trusts since the middle of last year. It offers median waiting times, trends data, numbers waiting at the 18 and 52 week thresholds - and all of this with instant Trust-by-Trust comparisons. NHS managers can download data to Excel spreadsheets for further analysis. Patients can print off headlines as a handy aide-memoire.
When we launched our tracker last June, we asked NHS England officials to work with us on raising awareness of it. Instead they have spent eight long months creating their own much less useful version.
We have asked how much the My Planned Care tracker cost to develop, but to no avail. But in case anyone in government is looking for value for money benchmarks, we can reveal that our waiting list tracker was developed with funding of £5,000. That's right - £5k to build brand new IT functionality and make it available entirely free of charge for every acute Trust in England.
So what is the point of My Planned Care? We think the story goes something like this...
In July 2021, the Secretary of State declared that waiting lists were his priority. By October, waiting lists were breaking through the 6 million mark. A couple of weeks ago a recovery plan was finally published. And so now, Something Must Be Done - even if this particular something already has been done.
It is hard to resist the conclusion that My Planned Care is more about political window-dressing than a genuine attempt to help patients.
Our offer to NHS England remains open: please work with us. Our waiting list tracker sits alongside our surveys tracker and, of course, the Patient Experience Library itself, as major innovations that support development of truly patient-centred healthcare services. We will continue to innovate, but will do so with patients in mind, not politics.
Tuesday February 22nd 2022
Who examines whom?
We are all becoming increasingly familiar with digital healthcare. The pandemic has of course accelerated adoption of "remote consultations" as a routine feature of clinical practice. At the same time, patients have been increasing their own adoption of online platforms as a means of giving feedback to providers.
With the emergence of the "digital health citizen", the authors of this paper detect a shift in what they call "surveillance".
At heart is the question of who is examining whom. Traditionally, the "clinical gaze" has been turned by healthcare professionals on patients. Bodies and minds are the subjects of research, physical examination, diagnosis and discussion. But according to the paper, "the gaze is turning, not simply from the patient to the health-care provider, but additionally to the body politic of the NHS".
This can be uncomfortable for healthcare staff. The paper refers to professionals who "almost universally spoke about the negative feelings online patient feedback elicited in them. This is in spite of evidence showing that most online feedback is positive".
Other staff were dismissive. By "not engaging with online feedback, staff retained control over... their own account of what good care looked like".
A further response was to "take control" - for example by directing patients to leave feedback on "legitimate platforms" such as NHS Choices; developing a social media strategy; and designating a staff member with responsibility for managing patient feedback.
But however staff choose to respond, the fact remains that clinicians' examination of patients is increasingly being matched by patients' examination of clinicians - and of healthcare as a whole.
Rather than speaking only for the "silent pathology inside their body", (ie personal illness discussed with the clinician) the patient now also speaks for the "silent pathology inside the body politic".
By this the authors mean the way that online feedback can be used to air issues that healthcare professionals might feel unable to speak openly about. Examples are waiting times to get an appointment, triaging by reception staff, problems with prescriptions - things that are "indicative of a system straining from years of underinvestment, staff recruitment challenges and increasing workload demands".
The paper finds that "online review and rating sites, then, are undoubtedly a form of surveillance". So it is important to remain attentive to how they shift knowledge and power relationships, and, potentially, turn the observers into the observed.
Tuesday February 15th 2022
A&E - relieving the pressure
Accident and Emergency departments have been making the headlines in recent months, with pictures of ambulances queuing outside hospitals, and reports of patients waiting up to eleven hours to be seen - far beyond the four hour target.
In this context, this report from the British Red Cross looks at the one percent of the population who account for more than 16 per cent of A&E attendances, 29 per cent of ambulance journeys, and 26 per cent of hospital admissions.
High intensity use costs the NHS £2.5bn per year - but what is driving that cost, and that behaviour?
The study combined literature reviews, data analysis and patient experience work. It showed a clear link between high intensity use and wider inequalities, being associated with areas of deprivation, and issues such as homelessness, unemployment, mental health conditions, drug and alcohol problems, criminality, and loneliness and social isolation.
It turns out that the key to addressing high intensity use of A&E is not so much about "patient flow" or hospital staffing or ambulance services. Instead it is a matter of "addressing the practical, social and emotional issues that can exacerbate people’s physical and mental health conditions, and ensuring that people have timely and appropriate access to support in the community".
One suggestion is to tackle the "high eligibility thresholds" which can prevent people with serious mental illness from accessing support in the community before reaching crisis point.
Another is to keep an eye on GP attendances. People who attend A&E frequently tend to do the same with other health services, so frequent use of GP services can be an early warning sign of high intensity A&E use.
The report offers a series of recommendations for Integrated Care Systems and national bodies. But it also points to missed opportunities - not least "an ever-shifting, but still widespread, disregard for the importance of addressing people’s wider social determinants of health through de-medicalised care and support".
Tuesday February 8th 2022
Low confidence in government
The millions of people on NHS waiting lists will be unhappy to hear this week's announcement of yet another delay to publication of the elective care recovery plan.
In this context, the Health Foundation's report on public perceptions and expectations of the NHS is timely.
It reveals that the public is pessimistic about the state of the NHS and social care. 57% think the general standard of care provided by the NHS has got worse in the last 12 months, while 69% think the standard of social care services has deteriorated.
Worryingly, less than half think the NHS is providing a good service nationally or locally.
The report states that people’s top priorities for the NHS include addressing the workload pressures on NHS staff and increasing the number of staff in the NHS. Clearly, people understand that workforce shortages are a pressing problem. In light of this, say the report's authors, "the continued absence of a comprehensive workforce strategy in England is a glaring omission in the government’s plans".
Confidence in government is low: in England, only 9% think the government has the right policies for the NHS, even as it progresses with a major programme of NHS reforms. 58% of the public support raising taxes to spend more on the NHS and social care. But "in the context of a cost-of-living crisis the government will need to keep making the case for the new tax - especially among those who will be paying the most towards it".
The report is the first from a new 2-year partnership between the Health Foundation and Ipsos. They will continue to track public views on health and social care every 6 months.
Tuesday February 1st 2022
A hidden injustice
The opener to this report is stark: "Around a third of people who find themselves in police custody have some form of mental health difficulty, as do 48% of men and 70% of women in prison". And the follow-up is clear: "people with a mental illness need and deserve treatment".
The report looks at how - and whether - people in contact with the criminal justice system (CJS) are getting the mental health services they need. The answers include these findings:
- There is no common definition of mental health used across the CJS.
- The mental health flagging system used by probation services is muddled.
- Significant problems in information exchange occur in every agency in the CJS.
- Probation practitioners are often hindered by community mental health service providers who do not allow them access to information held on individuals they are working with.
- Prison officers are not supported well in their continuous professional development in working with prisoners with mental health vulnerabilities.
- Prisons continue to be used as a place of safety, and Mental Health Act transfers out of prison custody are taking far too long.
The report contains 22 recommendations which address these, and many other, failings. It calls for most of the recommendations to be completed within 12 months.
The authors cite the 2009 Bradley report, which stated that "failure to adequately address the mental health needs of offenders is a fundamental cause of the chronic dysfunction of our criminal justice system". They go on to say that "not enough progress has been made in the 12 years since the Bradley review".
They could also, perhaps, have mentioned Prime Minister Theresa May's 2017 description of mental illness as a "hidden injustice", and her call for "parity of esteem" between mental and physical health services. Five years have passed since then, and the goal of parity still seems a long way off.
Tuesday January 25th 2022
Building back better for babies
The UK Government’s investment in the Best Start for Life vision is, say the authors of this report, welcome. However, "there remains a 'baby blindspot' in COVID-19 recovery efforts and a shortage of funding for voluntary sector organisations and core services like health visiting to offer the level of support required to meet families’ needs".
The report builds on research from 2020 which showed that COVID-19 and the lockdown affected parents, babies and the services that support them in diverse ways. While some families thrived, others struggled, and in particular, "families already facing greater adversity were often hardest hit by the pandemic".
This update finds once again that some families are adapting well, and are feeling the benefits of time together. At the same time, 87% of parents were more anxious as a result of COVID-19 and the lockdown, with families from Black and Asian communities, young parents and those on low incomes reporting higher levels of anxiety.
Many find it difficult to access care, particularly from universal health care professionals like GPs and health visitors. Over a quarter of respondents reported that health visiting routine contacts remain mainly on the phone or online. Nearly a third report that health visitor drop-in clinics that existed before the pandemic no longer operate.
While digital support has an important role to play, remote consultations can make interactions difficult. People wished someone could see their babies in order to provide them with the reassurance that they, as parents, wanted.
The report makes three demands:
- The UK Government must support local authorities to invest in and rebuild health visiting services.
- Babies and the services that support them must be included in COVID-19 recovery policy and investment at a national and local level. This must include investment in community and voluntary sector support.
- An evidence-based approach must be taken to ensure the appropriate use of digital and phone-based service delivery, and investment in relational, face-to-face support where this is needed.
"Without urgent action to secure recovery", says the report, "we fear that the pandemic will leave permanent scars on the provision of support for babies and young children".
Monday January 17th 2022
Online records - what patients want
This paper starts with a simple statement: "The general practitioner (GP) contract in England states all patients should have online access to their full primary care record".
Scratch the surface, however, and things are not so simple. Clinicians worry that online records access (ORA) could cause unnecessary anxiety, increase complaints and threaten confidentiality. There are also fears of widening health inequalities and increased clinician workload.
Against that background, this paper asks what patients want. It found four main themes:
- Awareness: Study participants felt ORA was poorly advertised, and suggested promoting it via media advertisements, posters in surgeries and during GP consultations.
- Capabilities: ORA enabled patients to view test results, medication lists, appointment details, and consultation notes. But participants wanted better presentation, including plain English, links to trusted sources of information, and access via one fully integrated system.
- Consequences: Some felt that ORA could improve safety by reducing the likelihood that test results would go unnoticed, or enabling them to spot errors in their record. However, others feared safety risks such as unreliable self-diagnosis, self-medication or discouraging clinicians from documenting concerns about mental health or abuse, for fear of upsetting patients.
- Inevitability: While there was some resistance to the move towards online services, there was an acknowledgement that much personal data is already held online - for example in the postal system, aviation and online banking.
The authors note further potential for online records access, taking in links with wearable devices, ordering of repeat prescriptions, and the ability to choose between remote and face to face appointments.
The potential, they say, needs to be developed through collaboration between patients, clinicians, policymakers and IT developers. And they conclude that "If we are to meet patient expectations regarding ORA, we need to go beyond simply enabling patients to view information".
Tuesday January 11th 2022
Know we're here
In June last year, just two days after being appointed Secretary of State for Health and Social Care, Sajid Javid was telling the House of Commons that we must learn to live with Covid.
Six months later, the arrival of the Omicron variant has been a sharp reminder that the Covid pandemic is far from over.
As various levels of Covid restrictions come and go, we need to remember that for some people, those restrictions are more or less permanent. As a heart transplant recipient, Tania Daniels is one of them. In the latest edition of our quarterly magazine, she offers a glimpse of the "financial, physical, and psychosocial toll of this ongoing quarantine for the immunocompromised".
People who continue to self isolate need more than "pat advice about masks and staying 6 feet part". They have lives to lead, bills to pay, family obligations to meet, and health needs to attend to. Tania's message is simple: "Know we're here - still waiting to connect fully back into life".
Another contributor is Cancer Mum, who has the task of "managing the health of a family member with serious health problems". For her, part of the solution is ready access to health records - and part of the challenge is persistent barriers to access.
This is partly a matter of our rights, as citizens, to our own healthcare data. But for patients with multiple complex conditions, it can also be a matter of life and death.
Technical issues can be solved, says Cancer Mum, but "Until the NHS... accepts the patient has a moral and legal right to access their health information there will be limited progress".
Tuesday December 14th 2021
Sleep and noise in hospitals
There is nothing new about the issue of noise and sleep in hospital. As long ago as 1859, Florence Nightingale remarked that 'Unnecessary noise is the cruellest absence of care'.
Hospitals continue to look for ways to reduce noise at night - recognising that disrupted sleep not only affects patients' experience, but also their ability to recover well from illness and surgery. Our recently completed literature review for the Royal Cornwall Hospitals Trust sheds light on some of the issues.
At heart is the simple fact that hospitals are noisy places. Sounds come from "conversations between and among patients, staff, and visitors, as well as the sounds of slammed doors, carts that are in need of repair, phones, beepers, buzzers, and paging". Beepers and buzzers can be unrelenting, with one study detecting 350 alarms per patient per day.
There are practical measures that can be taken: slow door closures can be fitted, foam pads can be added to bin lids, call bell volumes can be reduced.
However, noise is not just a matter of decibels. Those beepers and buzzers might not actually be very loud - but "Electronic sounds were consistently more arousing than other sounds at the same noise dose". Additionally, "perceptions and tolerance of noise can be very personal". One person's background chatter can be another person's sleep destroying irritant.
Key to noise control is a recognition that "noise does not happen by accident". One paper notes that disruptive noise "exists only because there are underlying cultural norms that permit and tolerate the disturbance".
Staff participation is therefore crucial to successful noise control. It should not, for example, be assumed that staff know how to control call bell and alarm volumes. And one study that compared noise control measures with and without staff involvement found that "addition of nursing education and empowerment... was associated with fewer nocturnal room entries and improvements in patient-reported outcomes".
Ultimately, noise is cultural as well as practical - and "Unless...the accountability for the auditory environment is with the staff, the noise issue will belong to no one".
Tuesday December 7th 2021
Trust and data sharing
"In most health systems at present, the point of care is also a point at which health data are generated." So say the authors of this paper, who also note that "In some cases, healthcare practitioners are being asked to act as points of contact for the consent or opt out process for data-sharing".
The scale of data gathering is immense: NHS England has personal data on more than 55 million people. And the volume of data increases daily because the service deals with over 1 million patients every 36 hours. The value is also huge: "NHS data have begun to be discussed as representing a 'goldmine' variously valued at GB£9.6 billion annually".
There is, however, growing evidence of "data-related harms, such that certain groups (e.g. people living in poverty, trans people, and ethnic minorities) face particular threats from...datasharing within administrative, health, welfare, and/or social care systems, including, but not limited to, intensification of discrimination".
The study, based on ethnographic research in North East England, identified three areas of concerns about sharing sensitive health data: substance misuse, sexual health, and mental health.
Concerns were most acute for asylum seekers, those experiencing domestic violence, transgender people, offenders, and ex-offenders. The authors remark that "those who are vulnerable to the greatest potential harms and discrimination from data-sharing are already those in society who are most marginalized and disadvantaged".
The authors are careful to balance their assessment: "This is not to say that people with vulnerabilities do not see the potential benefits to be had in terms of improved direct care". But the question of control remains: "...even those who have the most positive views of data-sharing do not want others to have unfettered access to data in their NHS records".
There is criticism of data sharing engagement approaches which propose "hypothetically based trade-off scenarios where risks (privacy violation) must be considered alongside benefits (new drugs being developed)". This, say the authors, "does not allow a flexible engagement of the participants with the premises on which the trade-off is based".
The paper suggests that "public engagement work should not be so focused on majoritarian perspectives that it ignores the concerns about potential harms for vulnerable groups. Public engagement can be enriched by careful consideration of the wider context that surrounds the topic of interest and the wider lives of those with whom we seek to engage".
Tuesday November 30th 2021
Lines in the sand
We recently featured a paper discussing the hidden web of influence exerted through the funding of All Party Parliamentary Groups by pharmaceutical companies.
This Australian paper picks up similar themes, looking at the extent to which pharmaceutical industry money might compromise the independence of patient groups.
It references a Finnish study showing that 71% of 55 surveyed groups received pharmaceutical company money and a study of US patient groups showing that 83% received funding from drug, device and biotechnology companies.
The consequences can be troubling - for example, "patient groups in the USA that advocated to maintain ready public access to opioids were more likely to be funded by opioid manufacturers than groups that advocated for restricted access".
Against this background the authors considered the risk of harm to patient groups' independence and asked what practices and policies are currently in use by patient groups to mitigate such risks.
Study participants described "pressure from pharmaceutical company funders to act in ways that prioritise company interests over their group’s interests". This raised concerns over independence - however, "there was little consensus around what constituted an acceptable behaviour limit or ‘line in the sand’".
Transparency was another risk area, but "Ways of declaring industry funding were variable, sometimes inadequate. In particular, there was an over-reliance on industry declarations, which may be hard to find, lacking detail or absent altogether".
Further risks - and mitigations - included "sponsor exclusivity, brand marketing, agenda setting, advocacy partnerships and content of patient group communications and events". On these, the authors "identified variation between patient groups in where they drew the line between acceptable and unacceptable practices".
All of this, say the authors, "is part of the increasingly recognised link between industry sponsorship of healthcare stakeholders and outcomes that favour the sponsor’s interests". This, they say, is "a pattern that is being repeated across clinical practice, medical education, guideline development and medical research". There is "urgency about identifying and managing financial conflicts of interests in the health sector in order to protect the public’s interests, including their health".
Tuesday November 23rd 2021
Maternity Voices
The crisis in maternity services is, perhaps, exemplified by two recent happenings.
The recent March with Midwives brought people onto the streets all over the country to stand in solidarity with midwifery staff. Alongside that, we have seen the announcement of yet another inquiry into poor maternity care - this time at Nottingham University Hospitals Trust.
Against this background, a report from the Care Quality Commission shines further light on the crisis.
The report is frank. It states that "Issues such as the quality of staff training; poor working relationships between obstetric and midwifery teams, and hospital and community-based midwifery teams; a lack of robust risk assessment; and a failure to engage with, learn from and listen to the needs of local women all continue to affect the safety of some hospital maternity services".
The latter point about listening to the needs of women is vital. Avoidable harm inquiries into maternity services at Morecambe Bay, Cwm Taf, Shrewsbury & Telford and East Kent have all pointed to a failure to take patient experience seriously.
The report looks at Maternity Voices Partnerships - a key link between maternity services and patients. It finds that working relationships between MVPs and maternity services vary - some are good, others less so.
Where relationships are good, MVPs can help with information materials and public outreach, and can also help with internal provider matters such as safety reviews. Importantly, they have "direct channels of contact" with the Head of midwifery, and "felt confident that they would be able to raise safety concerns".
On the downside, some MVPs felt that their role was not well understood by providers. This includes "the MVP not being involved early enough in the process to give meaningful feedback and the trust being defensive to suggestions from the MVP". In one example, an MVP "was sometimes only given sight of documents after they had already been shared with the public in what felt like a tick-box exercise".
Alongside variations in relationships is a disparity in funding between different MVPs, as well as varying expectations for MVP Chairs, with some being expected to go above and beyond their paid role. This is seen as "a barrier to women from some communities or groups getting involved, perpetuating issues with a lack of diversity".
The report calls for "true engagement" with Maternity Voices Partnerships, and says that "local maternity systems need to improve how they engage with, learn from and listen to the needs of women, particularly women from Black and minority ethnic groups". Crucially, "They also need to make sure that targeted engagement work is appropriately resourced".
Tuesday November 16th 2021
The impact of memory making
Children's palliative care deals with life limiting conditions in childhood, defined as "A disease or illness for which there is no reasonable hope of a cure and from which the child will die before the age of eighteen".
This paper states that "The diagnosis of a life limiting or life-threatening condition has a profound and lasting effect on families and poses a huge challenge to lead a normal family life". Importantly, "The loss of the child encompasses an entire journey into a new life, rather than being a single event".
Memory making can help families through this journey by continuing, in a meaningful and comforting way, the bond with the child who has died. The process is described as "the creation of individual pieces of art with families [including] Fingerprint pendant projects, memory boxes or the retention of a lock of hair".
The study asked bereaved parents about their experiences of memory making. Three main themes emerged:
The process of making the memories enabled parents to "make the most of precious time". Some who had not previously considered the concept of memory making "expressed gratitude that the subject was broached, and the opportunity afforded them to create memories and tangible pieces of art".
The impact of memory making was described as "overwhelming" but was also expressed in terms of joy and comfort. One mother described how tangible memories communicate "an invitation to mention her baby son, appreciating that though it is difficult for people it is welcomed".
Memory making also helped with the end of life care journey. It helped parents to deal with "anticipatory grief" and, in the words of one mother, to realise that "her baby's time was drawing close".
The findings, say the authors, "demonstrate the importance and the willingness of parents to have the opportunity to create special and precious mementos with their child when time is short". They recommend these as worthy issues to consider when planning the care of families facing the loss of their child, in order to guide, support and navigate their journey with them.
Tuesday November 9th 2021
Rationality vs complaints
"Mechanisms for raising complaints and concerns often disappoint those who use them, or fail to produce a resolution that meets their expectations".
So say the authors of this report, who immediately point to one cause of difficulty: the fact that complaints come from highly personalised experiences and motivations, but are met by complaints procedures "oriented towards organisational objectives". Another way to describe this is as a difference between "communicative rationality" and "functional rationality".
Communicative rationality is what happens when people engage in deliberation, constructive disagreement, and negotiated consensus.
Functional rationality, however, "belongs in the domain of the System". It enables people to work towards organisational objectives that have already been established, and are not up for negotiation.
In healthcare complaints, functional rationality means that humane and compassionate dialogue can sometimes be displaced by the logic of procedure.
One example is the "often tangled web of pathways for speaking up, reporting issues, raising grievances, commenting on care and complaining...Each pathway had its own procedures, policies and personnel, as well as timelines and terms of reference, all oriented towards its own, functionally rational objective".
Straightforward concerns about uncontroversial matters can be well served by such pathways. But for both patients and staff, many concerns are more complex, relating to "overall experiences of a whole interaction with the healthcare system". In spite of this, they tend to be "allotted to pathways that were not equipped to handle such unwieldy concerns".
When complex concerns are channelled into predetermined pathways, they can become 'stripped of meaning'. The overriding goal is 'packaging them in a form that could be processed". Ultimately, "the collection of patient experience data... can become estranged from understanding patient experience itself, preoccupied instead with processing data for its own sake".
The authors ask what a better way of responding to complaints and concerns might look like. Importantly they do not suggest that existing functionally rational processes should be jettisoned. But they do suggest a greater role for communicative rationality, via processes (independently facilitated if need be) that can allow for a more sense-making response. This, they say, could "ensure that wider considerations were deliberated, rather than being discarded by functionally rational processes that had no means of addressing them".
Tuesday November 2nd 2021
Better care for patients and planet
In an NHS struggling with elective care backlogs, staff shortages and oncoming winter pressures, health professionals could be forgiven for thinking that the CoP 26 climate conference in Glasgow is not particularly relevant. That, however, would be a mistake.
We have previously featured reports that have shown how the climate crisis damages population health - with the poorest and most vulnerable, as always, being the worst affected.
In September, for example, 200 health journals worldwide published the same editorial on health and the climate crisis. It called on health professionals to "join in the work to achieve environmentally sustainable health systems", and made the point that "Better air quality alone would realise health benefits that easily offset the global costs of emissions reductions".
The World Health Organisation's CoP 26 Special Report reinforces the message. It says that health and social justice need to be placed at the centre of climate negotiations, and that the global health community needs to "act with urgency".
To hard-pressed NHS staff, this might seem like just another burden. But some NHS Trusts are already showing that change is both feasible and beneficial.
Have a look at the great video on this page, where a healthcare worker describes her Mary Poppins electric bike that speeds her along on her daily rounds.
This video shows how reduction in single use plastics (disposable gloves) became a big selling point underpinning a hand hygiene campaign. It also saved the Trust a lot of money.
Here we see climate awareness being built into professional training and practice, with benefits for staff, patients and the planet.
The WHO report covers worldwide issues. But it is dedicated to the memory of a little girl from London. Ella Kissi-Debrah died at the age of nine after a series of hospitalisations for severe asthma attacks. The coroner's ruling recorded air pollution as an official cause of death for the first time.
We can do better. And the Trusts featured in the videos above are showing how.
Tuesday October 26th 2021
A make or break for digital health?
The announcement of extra government funding to digitise the NHS must, surely, be welcome. As always, however, it makes sense to dig beneath the headlines.
For patients, adoption of digital healthcare is not just about cash and affordability. All kinds of public attitudes and experiences are in the mix.
This paper sheds light on one in particular: the willingness or otherwise of older people using health-related apps to share their self-collected data.
The first research question addressed the use of mobile devices that enable older adults to track and share their health-related data. It found increasing use of smartphones and tablets by over 65's - showing that many older adults have the tools to use health-related apps. However, use was lower among the over 80's - the age group that would potentially benefit the most from mobile health interventions
The second research question considered levels of interest in health-related apps. This matters because both age and interest in technology are factors in take-up of digital health opportunities. The study found, however, that levels of interest are lower among older people.
A final research question addressed the willingness of older adults to share self-collected health-related data. It found that a considerable number of older adults were willing to share data - but more so with doctors or hospitals than research institutions or health insurance companies.
People who already used health-related apps were more open to sharing their data, as were people with a higher interest in technology, a higher income, and a higher education.
The authors suggest that given the potential for health apps to improve health and behavioural outcomes, there should be efforts to increase health app use among older adults. However, they warn that discussions need to be held around the practicalities of data sharing, as well as around legal, ethical, social, and technical matters. These discussions should include issues such as informed consent, data privacy, data security, and data ownership.
The study finishes by pointing to a need for new models of participant involvement, with the goal of creating a trusted relationship between data providers and institutions working with data.
Tuesday October 19th 2021
Online feedback - Caring for care
This study opens with the statement that "the number of people who go online to... provide feedback about their healthcare experiences has been slowly and steadily growing".
The trend is not always welcome: "A key concern expressed by healthcare professionals, especially doctors, is that online feedback is produced by an unrepresentative minority expressing extreme views".
The authors, however, wanted to know what patients themselves thought. So their study looks at how people who posted online feedback across different platforms in the UK understood the relationship between online feedback and care improvement.
They found that a major motivation for providing feedback was to improve care for other patients and their families. People hoped that their comments would inform healthcare services and result in tangible changes. Feedback of this kind was a form of advice, suggestion or recommendation directed at the service provider.
Alongside this - and regardless of any actual changes made to services - providing online feedback was seen as participation in care itself - for example, by helping other patients and their families prepare, or by making healthcare practitioners feel appreciated.
People's feedback practices were shaped by both their own experiences of care and by a strong moral commitment and sense of responsibility towards other patients and service users, as well as healthcare professionals and the NHS itself.
The authors describe this as "caring for care". The phrase "invokes an understanding of care that is characterised as much by frustration, concern and vulnerability as by love, affection and nurture".
They say that "People providing online feedback in the context of public healthcare services do so both as patients... and as public healthcare citizens". Furthermore, "the amount of practical and emotional labour that goes into people’s online feedback practices... contrasts with an understanding of feedback as done quickly or even flippantly".
Tuesday October 12th 2021
Another bad apple?
Six years ago a baby (called Baby J in this report) died in the care of the NHS in Bristol.
The death of a baby is a terrible thing. But instead of comforting the parents and explaining what went wrong, staff at the hospital made things worse. Here is what the Parliamentary and Health Service Ombudsman has to say:
- "Doctors should have considered a hospital post-mortem, but they did not do this and did not talk to Mr and Mrs N about a post-mortem."
- "The Trust’s staff were not open and honest with Mr and Mrs N about the events surrounding J’s death as they should have been."
- "Immediately after J’s death doctors failed to give Mr and Mrs N important information they needed and wanted to know about J’s illness, and compounded this by failing to send them a copy of J’s discharge summary."
- "Doctors did not tell Mr and Mrs N about J’s pseudomonas infection until a meeting seven weeks after J died, and then told them they had done tests which were negative, when those tests had not been done."
- "The Trust did not properly equip and empower its staff to acknowledge when things had gone wrong and to meet its duty of candour: on the contrary, staff talked about deleting a recording made during one meeting while Mr and Mrs N were out of the room, because it might get the Trust into difficulty."
The Ombudsman finds that "Mr N and his wife suffered serious injustice in... the way the Trust responded to their questions after J died and in its handling of their complaints. The failure to consider and talk to Mr and Mrs N about a post-mortem means they will never have answers to some of their questions about how and why J died".
We must hope that the Trust in question - University Hospitals Bristol and Weston NHS Foundation Trust - is reflecting on its conduct. At the same time, we must be aware that the Trust is not a lone "bad apple". Its behaviour is part of a pattern.
This latest report echoes findings from previous PHSO reports such as Missed Opportunities, Ignoring the Alarms, and The Life and Death of Elizabeth Dixon.
The story mirrors the treatment of patients and bereaved relatives at Mid Staffordshire, Morecambe Bay, Southern Health, Gosport, Cwm Taf, Northern Ireland (Hyponatraemia), Shrewsbury & Telford and East Kent.
Avoidance and denial were also featured in the healthcare system's responses to the criminal activities of breast surgeon Ian Paterson, and the harms to thousands of women from devices including pelvic mesh.
We have an NHS which claims to be person-centred but which - at the system level - struggles to take patient experience seriously and persists in being unable to learn from its mistakes. It could do better:
- Health Education England could support the professional development of patient experience staff, who are almost unique in the NHS workforce in having no professional qualification.
- NHS England could offer more and better analytical tools to help people make sense of patient experience data.
- The National Institute for Health Research could develop a strategic overview of the patient experience evidence base, so as to reduce duplication and target research where it is actually needed.
- NICE could make patient experience evidence a dedicated part of the research databases that make up the National Core Content.
The PHSO says that the Bristol and Weston Trust "did not properly equip and empower its staff to acknowledge when things had gone wrong and to meet its duty of candour". But how can it, when NHS national bodies so conspicuously fail to give Trusts the system level support that they, too, need.
Tuesday October 5th 2021
A tale of two endings
Patient experience is not just a matter of customer satisfaction. Sometimes it is about the ways in which people are treated at the most vulnerable points in their lives. And in those moments, the experience of the patient's relatives can matter just as much.
In the latest edition of our quarterly magazine, we hear from two contributors whose experiences illustrate both ends of the spectrum of care.
Jane was held by a care team through her mother's last hours. The communication, co-ordination and tenderness were so good that Jane is able to remember the whole experience as "a magical time". For her, "It was text book perfect - except you can’t teach what these nurses gave us from a text book".
Kate's experience of her brother's untimely death was, sadly, much worse.
As a mental health patient, "He spent much of his adult life in a revolving door of care that oscillated between insufficient community-based support and enforced inpatient care that was often little more than a modern alternative to Victorian-style warehousing".
Kate's brother was, she says, "far too young to die". Her view is that "when it comes to supporting people severely affected by mental health conditions, we must do much, much better".
Jane and Kate's stories show what some might call "unwarranted variations" in quality of care. But human experience is always at the heart of those variations. And it must always be at the heart of any healthcare system that wants to be person-centred.
You can read Jane and Kate's stories, plus our round-up of the latest and best in patient experience research in the magazine.
Tuesday September 28th 2021
A hidden web of influence
This paper looks at how the pharmaceutical industry - and the organisations it funds - interact with Parliament to form part of a multi-layered web of influence
It concentrates on All Party Parliamentary Groups (APPGs), stating that "These informal cross-party groups revolve around a particular topic and are run by and for Members of the UK’s Houses of Commons and Lords. They facilitate engagement between parliamentarians and external organisations".
According to the authors, "APPGs do not receive any funding from Parliament, but they can choose to accept payments to cover costs of events, secretariats, travel, reports, and other activities". Consequently, "concerns have been raised that some corporate interests exploit the unique opportunities for access offered by APPGs, turning them into a backchannel for lobbying".
The study looked at financial reports between 2012-2018 from 146 health-related APPGs, finding that payments from external donors totalled £7.3 million. Of this, it says, the pharmaceutical industry and industry-funded patient organisations provided a total of £2.2 million. The authors state that their study "shows pharmaceutical industry funding at the upstream stages of the policy process".
To help manage any conflicts of interest, "transparency must be improved at the level of donors (pharmaceutical industry) and recipients (APPGs)". The paper points out that "Troublingly, pharmaceutical companies are not required to disclose these payments at all and are therefore missing from Disclosure UK, a transparency initiative".
In addition, "the payments from patient organisations with conflicts of interest identified in our research suggests that industry might deploy a multi-layered 'web of influence' strategy through partnerships with patient organisations". However, "Regulating these indirect types of conflicts is more complicated than direct conflicts of interest as they are inherently hidden as they do not need to be explicitly reported".
The authors conclude that APPGs "must go further in ensuring that the public to which they are accountable are fully aware of who funds them, why, and the impact". Furthermore, "Making this information easily accessible in one place is crucial given the frequent role of industry funded patient organisations in APPG activities, evidenced by their numerous in-kind payments, and the risk that the patient voice might speak with a ‘pharma accent’ when involved in policy discussions".
Tuesday September 21st 2021
Ten years on from Winterbourne
"Autistic people and people with learning disabilities have the right to live independent, free and fulfilled lives in the community and it is an unacceptable violation of their human rights to deny them the chance to do so." So says this report from the House of Commons Health and Social Care Committee.
However, it also notes that "The poor treatment of autistic people and people with learning disabilities has been a long-standing problem for the NHS and care system".
The report refers to the 2011 Winterbourne View disaster, and says "the fact that these issues have not been resolved even a decade later is a scandal in its own right". Despite efforts to enable autistic people and people with learning disabilities to live independently in the community, "there remain over 2,055 people in secure institutions today where they are unable to live fulfilled lives and are too often subject to treatment that is an affront to a civilised society".
They "can find themselves experiencing intolerable treatment [including] abusive restrictive practices; being detained for long periods of time... and being kept long distances away from their family and friends".
The Committee finds that "autistic people and those with learning disabilities are treated as if their condition is an illness instead of a fundamental part of their identity". Its report goes on to say that "the tragic result of this fatal misunderstanding is that they often do then develop mental or physical illnesses which are used to justify their continued detention".
The report makes a series of recommendations, and notes that "Helen Whately MP (Minister of State for Social Care, Department of Health and Social Care)... considers the issues we are raising to be important and has shared her discontent that there remain significant problems with the treatment of autistic people and people with learning disabilities".
Whately, however, has now moved to the Treasury. It remains to be seen whether Gillian Keegan, her successor, will want to act on the Committee's advice.
Tuesday September 14th 2021
A call to action
Last week saw an astonishing development in the world of medicine, when 200 health journals worldwide published the same editorial on health and the climate crisis.
The message is blunt: "Health is already being harmed by global temperature increases and the destruction of the natural world". And, say the distinguished authors, "The science is unequivocal; a global increase of 1.5 degrees C above the pre-industrial average and the continued loss of biodiversity risk catastrophic harm to health that will be impossible to reverse".
What does this have to do with patient experience? Exactly this: "Harms disproportionately affect the most vulnerable, including children, older populations, ethnic minorities, poorer communities, and those with underlying health problems".
Climate change is not just an environmental problem. It is also a persistent driver of health inequality.
The time for action, say the authors, is now. "Despite the world’s necessary preoccupation with covid-19, we cannot wait for the pandemic to pass to rapidly reduce emissions."
The solution, as with Covid, needs to be driven by governments. "Many governments met the threat of the covid-19 pandemic with unprecedented funding. The environmental crisis demands a similar emergency response." But investment will produce "huge positive health and economic outcomes. These include high quality jobs, reduced air pollution, increased physical activity, and improved housing and diet. Better air quality alone would realise health benefits that easily offset the global costs of emissions reductions".
Health professionals, too, must play their part. The authors state that "As health professionals, we must do all we can to aid the transition to a sustainable, fairer, resilient, and healthier world". And they go on to say that "We must join in the work to achieve environmentally sustainable health systems before 2040, recognising that this will mean changing clinical practice".
The article finishes with this: "Urgent, society-wide changes must be made and will lead to a fairer and healthier world. We, as editors of health journals, call for governments and other leaders to act, marking 2021 as the year that the world finally changes course".
Wednesday September 1st 2021
Changing relationships
The question posed by this study is "how does patient involvement transform professional identity?".
This tends not to be a question that is considered very much - indeed some readers might wonder what it even means. The authors explain that healthcare professionals hold a "strong and deeply entrenched relational ideal: that of the ‘good caregiver’ looking after patients".
A key role for the good caregiver is to "protect the patients’ trust in their professionals". Consequently, professionals can be "afraid to become too familiar or to reveal flaws or imperfection". They want to "maintain a professional ‘healthy distance’".
Patient involvement introduces a new, and different, model for professional identities and relationships. To move from 'good caregivers' to 'good partners', professionals' relationships with patients "should not be hierarchical, but rather built on reciprocity and transparency". This could be demonstrated through "informal terms of address (eg, using first names), sharing of personal stories and demonstrations of camaraderie between patients and professionals".
This process of transforming the ‘caregiver-patient’ relationship into a ‘colleague-colleague’ relationship can generate 'identity upheavals' among professionals". For example, some professionals in this study feared that a patient partner presence in the ‘backstage’ of professional practice could uncover ‘imperfections’ or ‘shortcomings’ that would undermine professionals’ identity story of excellence.
Remuneration for patient partners also crystallised identity questions. Most professionals felt that as they and patient partners shared the same identity within a quality improvement committee, they should all be paid. "However, when questioned on the salary [patient partners] should obtain, professionals showed discomfort".
A further problem for professionals was that if patient partners are seen as full members of the team, that could "distance them from the ‘ordinary’ patient". This issue was "repeatedly expressed by professionals as a concern regarding the insufficient ‘representativeness’" of the patient partner.
The study finds that for professionals, it can be hard to maintain the inner balance between the roles of carer and colleague. "Professionals struggle with this dual identity and transfer this ambiguity to their perception of the patient’s identity as a ‘real patient’ or not".
Tuesday August 24th 2021
Learning from complaints
In our Inadmissible Evidence report, we highlighted a problem with the use of language in healthcare.
When a health professional flags up something that has gone wrong, it is called an incident report. But when a patient does the same, it is called a complaint. The result is that health providers can sometimes find it hard to see complaints as a basis for learning.
This report from the Parliamentary and Health Service Ombudsman (PHSO) shows why complaints matter.
The report focuses on imaging services which, says the PHSO, can mark a crucial point in people's NHS care. "The results of an X-ray, CT or MRI scan can provide reassurance and relief, or the start of essential medical care and treatment". However, "when something goes wrong... it can have life-changing consequences for patients and their families".
By collating and analysing complaints, the PHSO found serious failings in imaging services. In particular:
Half of the cases show that Royal College of Radiologists’ guidelines on reporting clinically significant unexpected findings were not followed.
Half of the cases show that local NHS trust policies were either not followed or were not clear enough to enable adequate follow-up of important unexpected findings.
In nearly a third of the cases, there were delays in reviewing or reporting on an image.
In nearly half of the cases there were missed opportunities to learn from mistakes. In some cases this meant the same mistake happened to the same patient more than once, or there was a missed opportunity to resolve issues earlier for them.
Importantly, the failings came to light because of patient complaints, not because of actions by providers. One Trust "did not take any action to address [their] mistake". Another, after two years of efforts by the complainant "had still not addressed the gap in their duty of candour policy". A third case found "failings in how the complaint was handled", and that "The Trust did not apologise to the family for their loved one’s avoidable death".
As so often in patient experience work, the effects were felt not just by patients but by relatives as well: "Families told us they experienced great distress because the outcome for their loved one could have been different if these failings had not happened".
The report makes a series of recommendations, one of which is about taking complaints more seriously: "Clinical directors and senior managers of NHS-funded radiology services should triangulate the learning from... complaints, claims, serious untoward events, patient safety issues, Freedom to Speak Up Guardian data and candour learning".
Tuesday August 17th 2021
Mental health inequities
"The Covid-19 pandemic has exacerbated the already existing inequity in population mental health in the UK', says this report from the Centre for Mental Health. However, 'longstanding limitations in mental health research mean that we do not have the necessary evidence to inform responses".
The report points to major gaps in mental health research, including that mental health research investment is not prioritised compared to physical health. The funding that is available is skewed towards scientific and clinical research, with less for research on prevention or social interventions.
To understand preventative and social aspects of mental health, it might be necessary to draw on lived experience. Indeed, contributors to the report were clear that ‘peer research’ approaches can lead to deeper and more authentic findings.
However, "While research generally now includes ‘patient and public involvement’ as a necessary element, the extent to which its potential has yet been realised is open to question".
Realising the potential might mean overcoming tokenism in patient involvement in research: 'Those with lived experience often have little opportunity to influence what happens... the nature and impact of their involvement becomes challenging to identify and at times, is lost completely'.
It might also mean looking at the structure of research pathways: 'Some people from service user led organisations found it much harder to gain funding [for research] due to a questioning of the reliability and credibility of their skills'.
A section on "Doing things differently" highlights some approaches that have been used in practice to overcome inequities and structural failings in mental health research. And the authors conclude that "While there may not be one right answer to addressing inequities in mental health research, there may be many better ways of doing research to get there".
Tuesday August 10th 2021
The self advocacy safety net
"It is still the case that, despite major redesign of care delivery, little is known about patient safety incidents occurring in acute medical units" say the authors of this study.
To learn more, they dug into ten years' worth of patient safety incident reports from the National Reporting and Learning System. Their findings included the following:
- Patient trajectory: A common theme with patient trajectory was lack of active decision-making and communication between teams. Errors included poor documentation, patient monitoring errors, and lack of continuity of care.
- Arrival to diagnosis: Common problems here included diagnostic error, often because the system relies on the most junior (and inexperienced) doctors seeing patients first.
- Management of care: Patients were at a higher risk of patient safety incidents when there were multiple handovers between teams, and transfers between wards.
Drawing back from the detail, the researchers looked for "metathemes", a term describing themes that are overarching and cross-cutting.
They found that the strongest metatheme was the system largely depending on patient advocacy. This was "necessary due to a lack of care co-ordination during the patient journey, resulting in patients having to remind staff about investigations or referrals". Worryingly, "patients who were unable to self-advocate were often overlooked due to system pressures".
Further metathemes were "Lack of care co-ordination" and "Decision-making using incomplete information".
This points, say the authors, to "the necessity of self-advocacy from patients as a safety net". They say that "The learning from these reports represents an invaluable opportunity to improve the safety of the acute medical unit for future patients".
Tuesday August 3rd 2021
Tackling digital inclusion
One very noticeable effect of the pandemic has been the huge growth in online activity. Patient experience and engagement work has been no exception - meetings, conferences, focus groups and training sessions are all held online, in ways that might have seemed inconceivable a year or so ago.
That has given rise to concerns about digital exclusion - so it is good to see NHS Providers producing this informative two-sider which offers practical tips on ensuring digital inclusion.
The guide keeps service users front and centre, recommending the involvement of patients and service users (along with staff) from the outset, to identify barriers to access and prevent people slipping through the net.
Public participation gets a mention too, with reference to "volunteer digital ambassadors" who can help to build confidence among patients and service users who are hesitant about using IT.
"Digital poverty" is recognised and addressed: some trusts have provided users with individual devices and supported improvements in local connectivity infrastructure.
The guide also features some handy design principles for digital inclusion, the first of which is "Put people at the heart of everything you do".
Importantly, "digital" is not held up as a panacea. The guide recommends "outcomes first, then digital". It also makes the point that "Digital inclusion isn’t about ‘either or’ - the strategy should be digital for those who can, so you can spend more time with those that can’t".
This is a concise guide - quick and easy to read, but with plenty of links to more information, should you need it. And although aimed at "Board leaders", there is much in here that could equally be used by people working on patient experience and engagement.
Tuesday July 27th 2021
A wait on your mind
It is common knowledge that backlogs in elective care are a major problem for the NHS, with over 5 million people now on waiting lists across England.
Equally well-known is that the experience of waiting for care is, for the most part, bad. Many people on waiting lists are enduring chronic pain, coupled with anxiety - often exacerbated by feeling left in an information vacuum. This is well documented in a recent report from National Voices.
Against this backdrop, a new report from the Policy Exchange sets out a series of analyses, accompanied by recommendations for policy and practice. These cover diagnostics, operational standards, surgical hubs and more. But it is good to see patient experience and engagement emerging as a central theme.
A key aspect is "operational transparency" which, according to the report, must improve. The authors state that "...clinical prioritisation and waiting times are hidden from patients. Few are informed about their likely wait time, and how this compares to their rights as set out in the NHS constitution". They go on to say that "The ‘consumer’ of the service is being left in limbo, with limited support whilst they wait".
We welcome the report's recommendation that "All GPs should be actively encouraged to access tools such as the new Patient Experience Library waiting time tool". We are in touch with the Royal College of GPs, and look forward to working with them to get the word out to general practice. And since our waiting list tracker is free to use, adoption will cost the NHS absolutely nothing.
In the meantime, as the report points out, "The voice of the consumer - the person waiting for treatment - remains underrepresented in the conversation". That cannot be right in an NHS that wants to be person-centred.
The report concludes that "For both the NHS and the Government, the narrative must not be that the backlog was simply addressed, but that opportunities were taken to do things differently, including embracing proven technology-led innovations and addressing health inequalities along the way".
Importantly, it adds that "addressing the backlog from the patient’s perspective could positively transform our existing approach to planned care - which remains largely unchanged in decades".
Tuesday July 20th 2021
Rights-based mental health
"Mental health has received increased attention over the last decade" says this report from the World Health Organisation. However, mental health services often "face substantial resource restrictions, operate within outdated legal and regulatory frameworks and an entrenched overreliance on the biomedical model".
The report highlights the need to promote human rights in mental health care settings. This includes eliminating the use of coercive practices such as forced admission and treatment, as well as restraint and seclusion, and tackling the power imbalances between health staff and service users.
It says that solutions are required not only in low-income countries, but also in middle and high-income countries. (One of those is the UK, where five long years ago, the then Prime Minister Theresa May described mental illness as a "hidden injustice", and called for "parity of esteem" between physical and mental health services.)
Examples of good practice are given from countries including the UK. What is most important, says the report, is that good practice is not just about person-centred and recovery-focused care, but is also about human rights. This means addressing "critical social determinants... such as violence, discrimination, poverty, exclusion, isolation, job insecurity, and lack of access to housing, social safety nets, and health services". These factors are "often overlooked or excluded from mental health discourse and practice".
The report offers guidance and recommendations on mental health policy and strategy, law reform, service delivery, financing, workforce development, psychosocial and psychological interventions, psychotropic drugs, information systems, civil society and community involvement, and research.
Importantly, "development of a human rights agenda and recovery approach cannot be attained without the active participation of individuals with mental health conditions and psychosocial disabilities. People with lived experience are experts and necessary partners to advocate for the respect of their rights, but also for the development of services and opportunities that are most responsive to their actual needs".
Tuesday July 13th 2021
Accountability in maternity care
As we move through 2021, maternity services remain under scrutiny. The forthcoming Ockenden report on Shrewsbury & Telford, and Kirkup report on East Kent will no doubt intensify the pressure on already hard-pressed staff and managers.
But we cannot go on condemning individual Trusts as 'bad apples'. It is too simplistic (and convenient) to label Morecambe Bay, Cwm Taf, Shrewsbury & Telford and East Kent as 'rogue Trusts'. Four in a row over six years looks more like a pattern.
So it is good to see the House of Commons Health and Social Care Committee looking beyond the providers, and asking some searching questions of government.
The Committee’s independent expert panel has looked at government progress against its policy commitments for maternity services in England - specifically maternity safety, continuity of carer, personalised care, and safe staffing.
The panel decided to make use of the Patient Experience Library as a key part of its evidence-gathering. This, crucially, enabled them to unearth important aspects of safety that do not necessarily show up in official statistics.
On the basis of the evidence that we provided, the panel found that:
- Positive impact in maternity safety was not achieved equally across different groups of women, such as women with disabilities or women from minority ethnic or socio-economically deprived backgrounds.
- There is a relationship between charging for NHS maternity care and inequitable outcomes for women from destitute or immigrant backgrounds. It is some of the women that are most in need of maternity care that are charged for it.
- Women with learning disabilities may avoid maternity care due to a of lack of confidence, negative staff attitudes, lack of clear explanations of what is going on, or fear of the involvement of social services.
- Asylum seeking women can be more likely to have to move to different areas multiple times during pregnancy, making receipt of continuity of carer more difficult. Similar issues are faced by women from Travelling communities.
Using a CQC-style rating system, the expert panel found that government progress against its own maternity policy commitments 'Requires Improvement'. On personalised care specifically, it was 'Inadequate'.
So government cannot go on pointing the finger at Trusts for failings in maternity care. It needs to take its own share of accountability, and it needs to put its own house in order. And on the evidence of this report, it has a long way to go.
Tuesday July 6th 2021
Transparency matters
Transparency of data is essential in a publicly-owned NHS. We have played our part during the last quarter, by launching our waiting list tracker to help bring NHS waiting times data into the light.
National headlines showing 5 million people on waiting lists may be of interest to the national media. But most patients want to know the state of the waiting list for the treatments they need at Trusts near them.
The data has always been published, but never in a way that patients (or even most health professionals) can make sense of. Our waiting list tracker opens up the data for all to see.
The question of transparency is also tackled by contributors to the latest edition of our quarterly magazine.
Nicky Lyon and Michelle Hemmington describe the Each Baby Counts initiative which, among other things, broke new ground by publishing data on the number of babies affected by potential brain injury or death in term labour. The data-driven approach has resulted in a significant reduction in overall stillbirth and neonatal death rates.
But data alone is not enough. Eleanor Stanley writes about the importance of personal stories that can "paint pictures that stick in the mind". This is vital to patient and public engagement because today’s sophisticated audiences are no longer touched by polished organisational messages. They want information that is authentic and meaningful.
As always, we have been picking through some of the latest and best patient experience research, and summarising it through the rest of the magazine. And we're always keen to hear from our readers, so if you know of a standout report that we should be featuring, or if you want to submit a comment piece, get in touch!
Tuesday June 29th 2021
Inverse care in practice
With the national GP patient experience survey due out shortly, this report from the Health Foundation is worth a read.
It considers the state of general practice in the context of the government's "levelling up" agenda. The starting point is that general practice is the part of the NHS the public interacts with most, with over 300 million appointments annually. It is also well liked by patients, demonstrating "high public satisfaction ratings when compared with emergency or inpatient hospital services".
There is a problem, however: the funding formula for general practice "does not sufficiently account for workload associated with the additional needs of people living in deprived areas". This has led to a 50-year persistence of the "inverse care law", whereby areas with the greatest health needs have relatively poorer provision.
Practices in deprived areas have, on average, lower Care Quality Commission scores, and lower performance in respect of the Quality Outcomes Framework. Patients have shorter than average GP consultations, despite being likely to have more complex health needs. And although overall patient satisfaction with general practice is high, it is lower in deprived areas.
The report argues that unless policies are specifically targeted at tackling the inverse care law, health inequalities may widen still further. One example is the post-Covid expansion of "digital first" primary care. The risk here is that people in deprived areas are more likely to live with multiple health conditions but are also more likely to be digitally excluded.
A series of "priorities for government" concentrates mainly on funding and workforce. But there is recognition that any such measures need to be set in the context of a wider set of strategies to reduce inequalities. "The inverse care law", says the author, "is not inevitable or irreversible. It is a consequence of the failure of policies to align resource with need".
This is a good overview, and is clearly not a one-off from the Health Foundation. Forthcoming work, we are told, will look in more detail at previous attempts to tackle the inverse care law in general practice in England, analysing what was promised, what was tried, and what has (and has not) worked.
Tuesday June 22nd 2021
Beyond consumerism
Covid 19 has exposed the fact that a consumerist approach to patient experience is, on its own, insufficient. If we only think about patients as "service users" and only ask them about "satisfaction with services", we will miss the bigger picture of patient experience.
Vaccine hesitancy is a case in point. The vaccine programme has been a huge success - but why does hesitancy persist? We are never going to find the answers in the Friends and Family Test, or the national patient surveys. But we might find some in studies like this, from Bradford.
"Misinformation" is, of course, a prime suspect. But it would be a mistake to think that public attitudes are only ever driven by conspiracy theories and fake news. The study finds that confusion and anxiety are also important factors.
Confusion can come from what has been described as an "infodemic" - so much information from so many sources that people are simply overwhelmed. In Bradford, people were getting information from very credible government sources. But those governments included Poland, Slovakia, Pakistan and India - and different responses by different governments affected how people then viewed the UK government approach.
Anxiety was often driven by social media. But although people were aware of the danger of fake news, their anxieties meant that they sometimes shared stories before really thinking about them. As one contributor said "they just forward it straight away and then it just spreads like wildfire".
Much of this plays out in the context of a pre-existing "partial understanding of disease transmission and vaccinations". One widely held view was that "the seasonal flu jab can give a patient the flu". Some people thought that the COVID-19 vaccine would be "stronger" than other vaccines, making it dangerous for recipients.
Importantly, the study found that "misinformation thrives in times of stress and uncertainty, and COVID-19 has provided a perfect breeding ground". Further, "feeling anxious makes people more willing to believe misinformation even if it is inconsistent with their world view". And "This appeared to be particularly heightened within marginalized groups, who had pre-existing reasons for mistrusting institutions".
There are important lessons here - not just for vaccine hesitancy but for other areas of healthcare where patient experience and public attitudes intersect. An obvious example is the General Practice Data for Planning and Research (GPDPR) programme which has been deferred in the face of public concern.
There has been much talk recently of a post-Covid "reset" of the NHS. Patient experience work, however, remains rooted in a consumerist model focussed primarily on "satisfaction with services". This study points to a need to reconsider that focus.
Monday June 14th 2021
One size doesn't fit all
"We need to pay attention to how gender is made in the digital transformation of community care", says this Swedish study.
The phrase "how gender is made" is central. The paper looks at artificial intelligence (AI) systems in community care. For example, an AI-based system that detects the fastest driving routes between care recipients or the likelihood of falls.
Advocates of AI in community care suggest that it can predict and prevent health deterioration, personalise care and increase patient participation. Opponents, however, claim that AI will depersonalise care, as the algorithms regard population averages and not the individual. As such, service users could become objectified through the lens of majority groups and universalism.
This matters, according to the author, because "Community care is not characterised by equality: most care personnel and older care recipients are women". Care work is low-paid and has low status, whereas digital entrepreneurship is associated with masculine values. These power relations "are rarely acknowledged or recognised".
Against this background, care providers "procure digital technologies and platforms in bulk...using the one-size-fits-all approach instead of working with care recipients and care personnel to co-create, design and deploy digital technologies and platforms". From a feminist perspective, the one-size-fits-all model fails to consider the importance of context, pluralism and diversity.
AI-based systems work from huge amounts of data, so the quality of the datasets is crucial. Biased datasets, built from unrepresentative samples, or based on stereotypes and social constructs, can amplify inequalities and perpetuate discrimination. Hence the concern with "how gender is made".
Using feminism as a framework for understanding the digital transformation of community care can, says the paper, help us move away from a one size fits all approach. Gender-transformative change does not happen automatically because gender expectations and power structures are reproduced and maintained if they are not recognised, acknowledged and questioned.
This requires "iterative work, in which assumptions and gender expectations are exposed and the design, implementation and use of technologies in community care are scrutinised, tested, evaluated, revised and tested again".
Monday June 7th 2021
Bringing waiting list data into the light
One of the biggest challenges facing the NHS after the Covid crisis is waiting lists. Half of the general public, according to Ipsos Mori, see "improving waiting times for routine operations" as the top priority in healthcare.
So why is waiting list data so hard to find, and to make sense of?
The data is, of course, published, on the nhs.uk website. But it is buried in vast Excel files, with impenetrable layouts and incomprehensible abbreviations. As so often with NHS reporting, the data itself is good but the presentation leaves considerable room for improvement.
Tired of the monthly struggle to work out what on earth was going on with waiting lists, we decided to do something about it.
Our waiting list tool takes waiting times for treatments in NHS Trusts in England and puts it all in one place. It is a huge breakthrough - bringing the data into the light and enabling anyone, at any time, to see how any part of the NHS is performing.
This matters because the experience of being on a waiting list is fundamental to people's perceptions of the quality of care. Last year, we worked with National Voices and Care Opinion on a report that looked into this. People talked about "fighting the system", and being in "an information vacuum".
The tool should also be useful to GPs - particularly at the point of referral, when patients are understandably keen to get some idea of how long they might have to wait for treatment. GPs can now see the latest figures for waiting times for any treatment at the click of a mouse. They can easily compare waits at different local Trusts. And one more mouse click prints off a simple "headlines" summary that they can give to patients as a handy aide-memoire.
Waiting list data has not been hidden for all these years for any good practical reason. Our waiting list tool shows that it is entirely feasible to present the data in ways that anyone can understand.
Tools like these can be built quickly and affordably. They should be a fundamental part of a person-centred NHS.
You can use the waiting lists tool here.
Tuesday June 1st 2021
Voice in the informal organisation
Various studies have shown that in healthcare, patient experience and staff experience are closely intertwined. Put simply, happy staff means happy patients.
This paper considers the importance of employee voice, which, it says, "is widely recognised as fundamental to patient safety and quality of care". In spite of this, however, "failures of voice continue to occur, often with disastrous consequences".
The authors look at how both the "formal organisation" and the "informal organisation" can help or hinder employee voice.
In the formal organisation, voice is encouraged via values statements, policy commitments to candour, reporting systems, and formal roles such as Freedom to Speak Up Guardians. But these do not always work.
A notable finding of investigations into healthcare failures, according to this study, is a gap between "formally espoused values of openness and listening, and the realities of raising concerns as they are experienced by those at the sharp end". Those realities are often governed by the informal organisation - the unwritten rules that manifest themselves through behavioural norms, social networks, power and politics.
Much in the informal organisation is good. Personal relationships and team spirit can supplement official rules (going the extra mile) and can also compensate for deficiencies, (areas where official rules and systems cannot cover all eventualities).
However, the informal organisation can also have what the authors describe as a "dark side". This can include "malign behaviours", "subgroups and cliques" and "advantage and privilege".
A key finding is that formal rules governing voice were not always well designed, complied with, or consistently interpreted. One example was ambiguity about what counted as a reportable concern requiring an organisational response. Participants reported that using the formally prescribed mechanisms for some types of concern was unlikely to result in action, or sometimes even acknowledgement.
"Etiquette" was another issue. Employees with concerns had to "form a sense of how likely or unlikely the formal organisation was to take them seriously, and to gauge the potential personal risks that might arise from a decision to speak up". Here, the informal organisation "provided clues and cues about what mattered, and the ‘etiquette’ (as opposed to procedures) governing the raising of concerns".
The authors conclude that while the informal organisation can "compensate for gaps, ambiguities and inconsistencies in formal policies and systems", it can also have a dark side, "potentially subduing voice by creating informal hierarchies, prioritising social cohesion, and providing opportunities for retaliation".
Their findings, they say, have implications for efforts to improve voice in healthcare organisations, pointing to the need to address deficits in the formal organisation, and to the potential of building on strengths in the informal organisation that are crucial in supporting voice.
Monday May 24th 2021
Learning from women's experience
Last week, we looked at the government's call for evidence for its proposed women's health strategy.
We made the point that over the last year, a series of large-scale avoidable harm scandals have all, primarily, affected women. These include the Paterson inquiry into unnecessary breast surgery, the opening of the investigation into maternity harms at East Kent, the Cumberlege review of treatments and devices including pelvic mesh, and the Ockenden report on maternity harms at Shrewsbury & Telford.
This week, yet another instance has come back into the headlines - this time involving the use of harmful breast implants.
The pattern is the same as always: women, in good faith, consented to treatment and then suffered harm. They spoke up, and found their concerns dismissed or denied. After an investigation, the truth started to come out.
In this case, the French manufacturer of the implants went into liquidation, and the founder of the company was jailed. But that was not the end of the story for the women affected.
Many were left with chronic pain, and continuing anxiety about possible long-term effects on their health. They wanted financial compensation, and they wanted the German TUV Rheinland company, which issued safety certificates for the implants, to accept its own share of responsibility.
Now, after a nearly ten year legal battle, justice is being served. A French appeal court has upheld the women's compensation claims, and has also upheld a previous finding of negligence against TUV Rheinland.
The BBC has said that the ruling could help up to 20,000 other women, half of whom are British, who are taking similar legal action in France.
As long ago as 2012, the UK government issued a report on the scandal. It said that "We owe it to the thousands of affected women to learn any lessons".
But one lesson is not being learnt. Paterson, East Kent, Cumberlege and Shrewsbury & Telford all show that our healthcare system still has not learned how to take patient experience evidence seriously.
NICE still does not have patient experience evidence as a dedicated part of the National Core Content. Health Education England still sees no need for patient experience staff to have a professional qualification. The National Institute for Health Research still has no strategic overview of the patient experience evidence base. NHS England still offers little in the way of analytical tools to help people make sense of patient experience data.
Baroness Cumberlege has said that patient experience "must no longer be considered anecdotal and weighted least in the hierarchy of evidence-based medicine". That is the lesson that our healthcare system still needs to learn.
Monday May 17th 2021
Women's voices at the centre

It is good to see the government's call for evidence to help develop a women's health strategy. Anyone who doubts the need for this just has to look back over the last year in the life of the NHS.
2020 is thought of as the year of Covid. But it was also a year that saw a succession of large scale avoidable harm scandals - all affecting women.
In February 2020, the Paterson Inquiry reported on the criminal activities of Ian Paterson, who performed unnecessary breast surgery on thousands of women. The same month saw the launch of an independent review into avoidable harm in East Kent Hospitals' maternity services.
In July 2020, the Cumberlege review of medicines and medical devices described the "anguish, suffering and ruined lives" of thousands of women affected by treatments including pelvic mesh. And in December 2020, Donna Ockenden's Emerging Findings report referred to 1,862 contacts from people who believe that they may have suffered avoidable harm in maternity services at Shrewsbury and Telford.
These harms were avoidable because the providers knew about them. Patients and bereaved relatives had been speaking up - sometimes for years. But no one had wanted to hear them.
Men have been affected too, as fathers, birth partners and spouses. But the brunt of the harm has been borne by women.
The call for evidence lists six core themes, the first of which is "Placing women’s voices at the centre of their health and care". But the evidence shows that women are, by and large, perfectly capable of expressing their needs and concerns.
Baroness Cumberlege described the women who contributed to her First Do No Harm report as "...well informed, knowledgeable, and research based. They never failed to ensure we learnt from them and were up to date with emerging developments. They are outstanding communicators and expert in the subject matter."
The problem is not with women's ability to speak. It is with the healthcare system's ability to hear.
Cumberlege went on to consider the tendency of medical professions to dismiss patient feedback as "anecdotal evidence". She said that patient experience "must no longer be considered anecdotal and weighted least in the hierarchy of evidence-based medicine".
We agree, and are working to address fundamental system weaknesses outlined in our Inadmissible Evidence report.
We call on NICE, Health Education England, the National Institute for Health Research and NHS England to join us. They set the tone, they set the culture, and they need to set a lead in placing women’s voices at the centre of their health and care.
A full version of this article is available via BMJ Opinion.
Tuesday May 11th 2021
Person-centred dementia care
"Person-centred care" is a key goal for all NHS services - but it is sometimes easier said than done.
This study looks at the care of people with dementia in acute settings. It says that while many hospitals have committed to the Dementia Friendly Hospital Charter, "the context of acute care still challenges the ability to routinely deliver person-centred care".
Examples of this context include:
- Standardised approaches such as time-based targets or routinised task care, which can disadvantage patients with needs that do not fit the prescribed approach.
- Organisational preoccupations with risk aversion, which can restrict patient choice and person-centredness.
- The tension between the drive to limit the time spent in a hospital against spending time to understand the patient and fitting in around their needs.
The answer, say the authors, is to rethink organisational and ward cultures.
Their first point is that there is no 'one size fits all' model of person-centred care. Indeed, "A generic or formulaic approach to person-centred care might even make matters worse".
Secondly, awareness and skills training for staff is not enough on its own. Crucially, "training of staff had to be combined with a recognition and valuing of the staff role itself". In particular, "Endorsement from senior clinical leaders and management was needed in order that staff felt confident that they had the authority to adapt working practices to meet emerging needs".
A third consideration is a dementia friendly environment on the ward - and within the hospital.
Approaches like these can come together within dementia specialist units. The paper acknowledges that these might not necessarily improve an individual’s health status nor reduce hospital resource use. However, "patient experience and family carer satisfaction can be improved, which for many approaching the end of their lives, might be considered significant outcomes".
The paper finishes with a set of pointers for improving institutional and environmental practices for patients, carers and staff.
Wednesday May 5th 2021
A limpet on a ship
Patient and public involvement (PPI) is now commonplace in research - indeed many research bodies make it a condition of funding.
That in turn, has given rise to a proliferation of "toolkits" explaining how PPI can be done well. But, say the authors of this paper, "little explicit attention has been paid to how the choreography and performance of collaborative research affects how PPI is imagined and practised".
The words "choreography" and "performance" are important. The paper sees the steering committee or advisory group as arguably the most common place for PPI to happen. But formal meetings are not simply places where business is conducted on objective and neutral terms.
They can also be "powerful ritual structures" which work to "reproduce dominant power relations". They can enact group norms through repetitive conventionalised acts whose "tacit rules constrain... what is on/off topic, who speaks and how, what actions should result from the meeting".
The paper's focus is "spatio-temporal dynamics" - in other words where and when PPI happens. It finds that hard to pin down.
In one meeting, a patient representative questioned the value of a prompt sheet for carers. "The chair listened attentively and suggested this might make for an interesting qualitative project - and then moved on to the next agenda item". In another meeting, a patient rep who questioned a definition of "harm" was countered by researchers asserting that their data was reliable and their study design robust. Further challenges from the patient rep were not minuted. At other times, discussion of PPI was met with assertions that it had already taken place, or was planned for a later stage.
The impression, say the authors, was that PPI was "simultaneously everywhere and nowhere". This sense was reinforced by a PowerPoint presentation showing specific workstreams within a research project. A double-headed arrow ran beneath them, separate from the columns and captioned "PPI". The arrow’s purpose was to indicate that PPI was present throughout all studies but it was not clear how. It was "running across the projects but hard to locate and specify, a constitutive part yet spatially and temporally apart from the rest".
The authors describe how frequently the metaphor of the jigsaw puzzle appears in descriptions of research involving PPI. Here, people with lived experience comprise the "missing piece", which promises access to the "whole picture". Health research, they say, "is presented as a collaborative practice in which all kinds of expertise smoothly join together: knowledge from 'lived experience' sits snugly alongside statistical reasoning and clinical trial bureaucracy".
The jigsaw metaphor "conjures a harmonious choreography - one where all actors have a part and move forward together". But the reality may be that PPI - and patient representatives - are more like a limpet on a ship. As one patient rep said, "you are just stuck on the side of something and people are very polite and they ask your opinion but basically they are doing what they want".
Wednesday April 28th 2021
Living and dying well during COVID-19
A few weeks ago, we featured Frustrated, Angry and Unfair - a report which considered the human rights implications of Do Not Attempt Resuscitation (DNAR) decisions.
It is good to see that the Care Quality Commission has also been working on this issue, with its findings now published in a report on living and dying well during COVID-19.
It starts with the observation that "From the beginning of the COVID-19 pandemic, there were concerns that 'do not attempt cardiopulmonary resuscitation' (DNACPR) decisions were being made without involving people". And its position on this is clear: "such actions were unacceptable".
The review (set up at the request of the Secretary of State) heard about the experiences of over 750 people, with findings that give cause for concern. In the foreword, the Chief Inspector says this:
"What we have found through our review is a worrying picture of poor involvement, poor record keeping, and a lack of oversight and scrutiny of the decisions being made. Without these, we cannot be assured that decisions were, and are, being made on an individual basis, and in line with the person’s wishes and human rights."
On the plus side, the report does not simply take a big stick to providers. It offers a series of practical recommendations, taking in information and training; consistent approaches to advance care planning; and improved oversight.
"Patient voice" is central: "providers must ensure that people and/or their representatives are included in compassionate, caring conversations about DNACPR decisions". But staff voice is important too: "providers must ensure that all workers understand how to speak up, feel confident to speak up and are supported and listened to when they speak up".
Last but not least, the CQC is willing to take its own share of responsibility. The final recommendation is that "CQC must continue to seek assurance that people are at the centre of personalised, high-quality and safe experiences of DNACPR decisions, in a way that protects their human rights".
Tuesday April 20th 2021
Learning from loss
The 2021 progress report from the Each Baby Counts programme will be its last. Set up in 2014, it aimed to reduce stillbirths, neonatal deaths and brain injuries incurred during labour. From now on, the work of investigation and reporting will be the responsibility of the Healthcare Safety Investigation Branch in England.
Parental involvement has been central to the ethos of Each Baby Counts. Nicky Lyon and Michelle Hemmington, founders of the Campaign for Safer Births, and bereaved parents themselves, have been involved from the start. Many others have participated over the years.
The good news is that there has been a significant reduction in overall stillbirth and neonatal death rates over the life of the programme. Another important outcome has been the number of parents invited to contribute to local reviews of injury or death.
Baseline data, published in 2017, showed that parents were invited to be involved in only 34% of reviews. The data in this year's report shows that 70% were invited to contribute. Alongside the declining death rate, this is a huge step forward.
Is there more to be done? Of course there is. Edward Morris, President of the Royal College of Obstetricians and Gynaecologists says that while the programme has opened a discussion on a difficult issue, "it is now imperative that the health system shifts its focus from counting to acting".
The publication of the Ockenden report on Shrewsbury and Telford must, he says "be a watershed moment for maternity services. The entire health system must recommit itself to challenging safety issues head on".
For their part, Nicky Lyon and Michelle Hemmington commend the programme for giving voice to harmed families. But, they say, "An area of major concern for us is that, with the end of Each Baby Counts and uncertainty on the future of the HSIB maternity investigation programme, this group of baby deaths and injuries may become invisible again".
Their final words, in this final report, are that "Learning must be turned into local and national action. These babies must not be forgotten again".
Monday April 12th 2021
Doing nothing
"Rehabilitation research has long recognised the importance of sustained activity, including physical mobility, social interaction and cognitive stimulation" says this report. Environments that offer opportunities for activity are therefore considered ideal - however, "The lack of meaningful activity in hospital is recognised as a problem".
The paper concentrates on stroke survivors, and says that studies consistently show that "patients in acute stroke units spend most of their time inactive and alone". But it also says that inactivity is "an experience shared across patients suffering from diverse conditions, from psychiatric disorders, to cancer, brain injuries [and] end of life conditions".
Planned activities, including mealtimes, medical visits and nursing care, were important stimulants, as were visits from family and friends. At weekends, however, there was "a significant downturn in terms of variety and frequency of these planned activities". Patients "often stressed the fact that during weekends 'nothing happened'". Interestingly, "nursing staff also shared this view". A healthcare assistant is quoted as saying "They get their care, obviously, but that’s it. It’s like - what happens now?"
Left to their own devices, patients struggled to find meaningful activities: "...while socialising was regarded as both enjoyable and helpful, patients in four-bedded bays could often be observed staring at the wall while being silent in the presence of each other. Similarly, while patients reportedly appreciated therapists' encouragement to exercise on their own, it was rare to see them doing so".
Some of this was due to the physical environment. The gym, for example, "remained closed when therapists were not on shifts". The corridor was "cluttered with chairs, desks, trolleys, filing cabinets and various pieces of equipment, which made it prohibitively narrow for patients".
De-personalisation was another influence. The bed areas were "typically rather bare", with little in the way of personal belongings or pictures that might have stimulated activity and interaction between patients. The "loss of personal identity... both contributed and reflected the lack of... familiar occupations".
The authors conclude that "patients' own activities were largely subsumed into the daily and weekly organizational arrangements of the unit". From this point of view, they say, institutional efficiency "did not only structure patients' patterns of behaviour, but also shaped what made sense for them to do. This view helps explain the lack of focus which characterised the time outside of planned routines, when meaningful activity unravelled into 'doing nothing' and even patients who appeared fully alert only a few moments earlier could be seen dozing off in their beds".
Wednesday April 7th 2021
Saving lives by listening
Does patient involvement in research really make much of a difference? It's a fair question, given the debates among academics about measuring and demonstrating "impact".
Our latest magazine offers a powerful example of how one patient with myeloma gave researchers a vitally important reality check. While clinicians got excited about possible new drug combinations, the patient - Mike Katz - questioned the use of one particular drug in the first place. His insights from lived experience altered the course of the research, and many lives were saved.
Other contributors, from a Biomedical Research Centre, show how they are moving patient and public involvement in research from a "neglected afterthought" to a process based on shared values and needs. Their aim is to make involvement more meaningful, and get better results - both for the people and for the research.
This matters because a healthcare system that wants to be both person-centred and evidence-based has to have a really good evidence base for patient experience.
We have been concerned for a while about the quality of the NHS evidence base for patient experience. No-one has a strategic overview of the evidence gathering, so there are big areas of duplication, as well as big gaps.
So we are aiming to make an assessment of the patient experience evidence base: identifying areas of saturation, and areas where the evidence is thin. On the back of that, we aim to suggest ways in which the research effort could be better steered, with time and money better used. Look out for more news on this in future editions of our quarterly magazine!
Tuesday March 30th 2021
Human rights under Covid
There are many ways to look at patient experience.
We can take a consumerist view - thinking about patients as users of services, and asking about their satisfaction with services. We can take a person-centred view - thinking about the personal experiences and needs of people living with illness. This week's report takes a right-based approach - thinking about the patient as a citizen with fundamental rights that are protected in law.
The focus is Do Not Attempt Resuscitation (DNAR) decisions, and the context is Covid-19. The starting point is a concern about the numbers of people accessing health, care and support services during 2020 who had experienced a DNAR order being placed on their file without consultation, or while feeling pressured to agree.
The report makes the point that DNAR decisions are not solely a medical matter. All medical decisions within the NHS are subject to the Human Rights Act - and since DNAR decisions are about people’s legally protected human rights, all staff have legal duties to uphold those rights in decision-making.
Importantly, human rights do not extend only to the patient. The Act also protects family life, so consultation with family members can also be an important part of the decision-making process.
Within all of this is the point that human rights should not be restricted in a way that is discriminatory. But the report finds worrying evidence of discrimination - for example, blanket DNARs applied to people with learning disabilities, and frailty scales being used to justify DNAR decisions for people with learning disabilities, but no underlying health issues. It also raises a concern about "assumptions related to capacity", and that people have not been involved in decisions about DNARs because they are assumed (but not necessarily known) to lack mental capacity.
Concerns about DNAR decision-making are not new. The report says that whilst Covid-19 has shone a brighter spotlight on these issues, they are part of a wider pattern of the discrimination experienced by disabled and older people within health and care. It finishes with a series of recommendations focussed on integrating human rights across decision making, policies and processes in healthcare.
Tuesday March 23rd 2021
One woman's experience
Patient advocates and patient experience staff can sometimes find themselves caught up in arguments over what constitutes evidence. Patient feedback is sometimes described as "anecdotal". It can be compared unfavourably, in terms of validity and reliability, with the "hard evidence" of statistics.
But anybody who doubts the value of "patient stories" as a way of understanding patient experience should read this painfully honest account of one woman's experience of incontinence.
This is not about patient experience as "satisfaction with services". It is about living with a long term condition that "seeps into every area of life".
It involves talking with doctors, and feeling stupid. Or worrying about making a fuss, or wasting their time. It is about the embarrassment of intimate examinations - even when carried out by health professionals who have "seen it all before". It is about fear, loneliness, self-reproach and fatigue.
On the plus side are those clinicians who acknowledge that incontinence isn’t very easy to talk about. Who say that they want to help, and that a physical examination will help to move things forward. Sometimes it can even be reassuring to hear professionals admit that they don’t have immediate answers, and that they need to find out more.
The article comes from the BMJ's excellent "What your patient is thinking" series. It offers the kind of insight that is not reliant on control groups, or peer reviews, or formal methodology. It comes from the heart, and from experience. And it rings true.
Personal testimony offers truths that can rarely - if ever - come from formal research or big set-piece surveys. Not that those don't have their uses. Sometimes we need big data and statistical analyses. But sometimes, one patient's experience can speak volumes.
Tuesday March 16th 2021
Out of the cancer maze
"We are at a crossroads for cancer care" says this report. "After a year of devastating disruption to diagnosis and treatment caused by the Covid-19 pandemic, no-one can be under any illusion about the scale of the challenge cancer services face to get back on track."
In the meantime, patients are caught in the maze - uncertain about their care plan, stuck between services, waiting for appointments and scans, or feeling on a "cliff edge" after their treatment ends. As many as 50,000 people may be missing a cancer diagnosis due to disruptions caused by coronavirus, with many people being too scared to seek help for symptoms from their GP.
The report is entitled "Caught in the Maze" but in fact, it suggests some ways through the maze. The starting point is the innovation and collaboration that the response to Covid-19 provoked.
Responding to the crisis has brought organisations together - improving collaboration while reducing bureaucracy and duplication. It has shown how care can be delivered in the community through diagnostic hubs and mobile units. And technology has enabled services to join up in a way that system leaders have long been attempting.
The report sets out a series of recommendations for how these advances can be maintained and built on. Workforce and funding are, of course, part of the picture. But integration of services and personalisation of care are also crucial.
That means plugging gaps in information and support, particularly during transition points between services. It means ensuring that Integrated Care Partnerships align with cancer alliances and providers to create a whole-system approach. Personalised care and support planning should be routinely provided and monitored for impact on people’s experiences and outcomes.
Importantly, modern cancer care for the three million people living with cancer is just as much about services outside the hospital as it is about acute treatment. So there should be greater learning from other long-term conditions, along with the removal of professional silos and expansion of cancer teams to include staff in mental health, end of life and social care.
A final recommendation is that pathways and service redesign should be shaped by the experiences of people living with cancer. "There is", says the report, "growing evidence about people’s experiences of cancer services across the UK... services should learn from people’s experiences and include people with cancer consistently as partners in the delivery of personalised, integrated care".
Tuesday March 9th 2021
Private data, public reporting
While Covid news continues to dominate the headlines, the government is busy preparing its Data Strategy for Health and Social Care. This, it says, "will set the direction for the use of data in a post-pandemic healthcare system".
Understanding Patient Data has done some good work on patient and public views of health data, and this latest analysis - in the context of the forthcoming government strategy - is well timed.
The focus is not so much the data itself, as how it is reported in the media. But that is crucial, since that is where most people get their information on health. In fact, the national media outlet reporting most frequently on health is the Daily Mail.
In the mainstream media, reporting has a tendency to be negative - generally, say the authors, because data becomes more newsworthy when something goes wrong (eg data breaches). There has also been doubt that the government’s approach to data handling would be effective in managing the pandemic, and scepticism that data would be managed ethically and not compromise human rights.
In more specialist science and technology media, reporting on healthcare data tends to be more positive - often driven by proactive company press releases announcing successes in clinical research and drug development.
On social media (Twitter in particular), concern about access to health data drives the majority of conversation, covering access by private companies, data breaches, and a lack of transparency around who data is shared with.
The study finds that the pandemic has made the benefits of health data clear to a wider audience and driven debate on the technicalities of regulation. On the other hand, reporting on the risks associated with the use of health data receives more cut-through with the general public than any other theme.
The authors recognise that health data is highly politicised, often becoming a lens for criticism of broader issues, such as privatisation of the NHS. And there is limited focus on the role an individual can play in managing their own data, potentially reducing opportunities for wider public engagement.
Among the recommendations is a call to "elevate patient voices" by encouraging patient involvement in debates on health data, and by training patient influencers to act as spokespeople on the benefits and risks of health data to patients.
Tuesday March 2nd 2021
Primary inequality
A key starting point for this study is the 2012 Health and Social Care Act, which set out a duty for healthcare commissioners and providers to reduce inequalities in both access to and outcomes of care. A particular focus was inequalities experienced by people living in the most deprived areas.
The authors acknowledge that there are well documented variations in patient experiences of primary care in relation to socio-demographic characteristics. However, they say, "there is limited evidence on longitudinal trends". So they set out to explore whether inequalities in patient experience of primary care had widened, narrowed, or remained the same between 2011 and 2017.
They found few substantial changes for the better. In particular:
- At both practice and national level, variations in patient experience persist, notably in relation to age, deprivation, ethnicity, sexual orientation and geographical region.
- At the national level, inequalities in access to care start to appear from 2015, with access declining fastest amongst practices serving the most deprived areas.
- Reported continuity of care is declining fastest amongst the oldest age groups when compared to other patients registered at the same practice. This matters because poorer continuity of care has been associated with higher rates of both generalised and preventable hospitalisations in older adults and higher rates of mortality.
The authors conclude that "Despite a sustained policy focus on reducing unwarranted variations in care, there have been no substantial improvements in inequalities in primary care patient experience between 2011 and 2017". And "Whilst access is getting worse everywhere, it is declining faster at those practices that serve deprived populations".
The paper warns that "With UK primary care under increasing pressure, widening socio-economic inequalities...are of particular concern". And it suggests that "public reporting alone is not an effective tool to drive reductions in inequalities in the UK".
Tuesday February 23rd 2021
Pestilence and penury
Campaigners and commentators on adult social care must feel stuck in a perpetual Groundhog Day, with government promises of reform followed by indecision and inertia, followed by more promises...
In the meantime, service users and carers carry on with a system which has for years been under acute financial pressure. Now, of course, the penury is compounded by pestilence - the added complications and strain of coping with coronavirus.
Amid that gloomy scenario, this report looked for signs of leadership and progress. And while it found "widespread complaint about a lack of leadership from the Department of Health and Social Care", it did manage to find local instances of initiative, and the will to provide good care.
Some of the most inspirational leadership, say the authors, comes from care staff themselves, and from adults of working age who have been empowered by personal budgets and direct payments.
The report gives examples of innovations and partnerships. Some are simple, practical and cheap. Some actually save time and money. (None of this takes away from the fact that people are improvising within a system that desperately needs more money.) A key message was that "The more local the leadership, the more powerful it could be".
Readers of this newsletter will not be surprised to hear that engagement and listening are crucial. One local authority is praised by a service user who says "We know where we stand. Not just the social services director but the chief executive comes to visit us - comes to our homes". In another area, a provider describes the basis for a good relationship with the county council: "The county consults. It listens. It adapts where it can".
In this respect, the Covid emergency has actually helped, by breaking down barriers. One domiciliary care provider described "peeling back of the layers around decision-making. People needed to just take action - really, really quickly. Just find a solution to the problem. There was that need for speed, and it worked really, really well".
The report carries plenty of good insight - but it is also realistic about the barriers to faster progress and better care. One is a lack of good data. One director of services said, "Certainly compared to the NHS but even compared to the police, we just don’t really know what’s going on". Another pointed to the lack of national leadership, observing that local leadership exists "in the vacuum of a nationally defined vision and plan".
So while the care system struggles on, local dialogue and relationships are vital. As the report says, "Local authority support for user groups, and for local care home associations and their equivalents for domiciliary care, appears to pay dividends. The best local authorities appear to value feedback, the worst hide from it".
Tuesday February 16th 2021
Engaging men earlier
In the world of patient and public involvement, it is well known that "engagement" is not evenly distributed. Terms such as "hard to reach", "seldom heard" and "underserved" are hotly debated - but all indicate a recognition that healthcare is better at hearing from some groups than others.
Men are not generally seen as "underserved". In fact, gender inequalities, gender pay gaps, glass ceilings and so on might suggest quite the opposite. But there are at least some men who, according to this report, are "going through tough times before reaching crisis point".
The report is based on discussions with men who "had not yet reached a mental health or suicidal crisis point, but who had been exposed to risk factors". Evidence indicates that men like these do not receive support early enough. But it also shows that some men do not see wellbeing initiatives as relevant "until they had hit rock bottom and were looking to rebuild their lives".
The study looked at initiatives that might support men’s wellbeing before they reach crisis point. Findings included the following:
- Study participants gravitated towards existing community groups and hobby-based activities rather than formal mental health or crisis services.
- The men were not particularly drawn to activities that were exclusively for men or based around what might be considered stereotypically 'male'.
- Avoiding 'awkwardness' when first joining an initiative was important, and it was felt that a focus on activities could help.
- A playful and fun atmosphere is the best way to foster meaningful relationships among participants. If an activity takes itself too seriously, it risks putting participants off.
There are plenty of other useful tips in the report, as well as examples of projects that embody these kinds of principles and approaches. The authors also consider how to adapt such approaches during lockdowns and physical distancing. It concludes with a "principles checklist" and an "action plan template", both of which could be useful tools for engagement practitioners.
Tuesday February 9th 2021
A vital partnership
"The pandemic has brought new attention to how people live their lives" says this report from the London School of Economics. "Questions are being asked particularly about housing, about inequality, residential care of the elderly, the health and care workforce and, of course, death".
The authors point to an important and authoritative source of guidance on these matters: charities. They recognise that the lockdown had a "dramatic impact" on charities' fundraising activities. In spite of this, they say, many showed great agility in adapting to changing circumstances and needs.
Far from simply plugging gaps in the welfare state, charities have often led the way in "improving standards of care, in professional collaborations, in reaching out into the community, and in making rapid adaptations".
The report considers the contribution of charities under five key headings: Wellbeing, Workforce, Inequality, Ageing, and Dying. It looks at the many ways in which charities have responded to the new challenges thrown up by the pandemic, taking in both policy and practice. Above all, it looks at "human impact" - an issue which is of course central to people's experience of care.
The report makes the important point that charities "not only rearranged their own services in response to the pandemic but often also helped guide NHS services through the coronavirus challenge". Charity staff and volunteers are not necessarily qualified healthcare professionals - but their different skill sets and experience, plus local knowledge and networks, can be a powerful complement to NHS skills and knowledge.
The report states that "The year 2020 simply accelerated the advance of the major challenges that the health and social care system needs to address. In particular it is a 'wake up call' around dying. Death rates seen at the height of the pandemic in spring 2020 will become the norm within the next 20 years".
Faced with growing needs in healthcare, it would, say the authors, "be both disingenuous and dangerous to assume that charities will forever be able to fill gaps in health and social care under 'business as usual'". They call for "a culture that respects charities as important partners in care planning and delivery, and an honest discussion of a shared role in filling the gaps now laid bare".
Tuesday February 2nd 2021
Making integration work
While healthcare systems wrestle with the twin challenges of Covid and delays in elective care, a third challenge is looming: integration.
This week, we look at a report that sets out a vision for "common purpose" in patient and public engagement at the system level. We also flag up (below) some practical tools that could help hard-pressed staff actually convert the vision to reality.
The report, "Building common purpose" starts with an observation about Covid-19. "The pandemic", it says, "created a common purpose that in many areas broke down barriers and enabled services to be transformed".
The authors see this as an important foundation for integration. In just a few months, they say, "every area of the country will be part of an integrated care system, with a ‘system by default’ approach". A "critical enabler" will be effective engagement and communications.
This is good to hear. It is well known that patients and public can find the healthcare system confusing, with its mix of providers, services, commissioning bodies and so on. It should not be assumed that patients and public will, unaided, be able to keep up with the forthcoming changes. Nor should it be assumed that healthcare professionals can successfully integrate services without understanding them from the patient's point of view.
The report recognises these challenges, and there is much in it that is welcome. It talks of embedding a strategic approach to engagement and communications. It mentions continuous relationship building. It recommends shared vision and narrative. And for all of these, it offers real life case studies.
As always, however, the devil is in the detail. The report sets out five success factors for high-performing communication and engagement. It lists ten communication and engagement functions. Those can be applied across three levels within integrated care systems. They can be delivered via four broad operating models. Finally, to summarise the findings, there is a ten part model for shared purpose public engagement and communications. It all gets a bit confusing.
Again, the good news is that the report is frank about the challenges. One example is its acknowledgement that healthcare leaders can often have "broad agreement on the strategic value of engagement and communications". But there is a tendency to act strategically in moments of crisis, then quickly revert to a purely operational approach once the crisis has been resolved
All in all, a good report - but our sense is that hard pressed staff, coping with the mountainous challenges of Covid, delays in elective care and the urgency of integration, will need practical help to get the alignments and synergies that the report recommends. Interested readers can see more on this below.
Practical support for system level engagement
We fully support the "common purpose" vision for integrated care systems, as set out in the report shown above.
Making the approach work will require practical tools. We are working on an online system that would allow anyone, anywhere within an integrated care system (subject to authorisations) to get instant, all-in-one access to:
- Patient experience/engagement documents (strategies, policies, action plans)
- Details on patient reps (who, where, role descriptions, training completed etc)
- Patient experience key datasets (eg survey findings, complaints data etc)
- Patient engagement budget(s) - a vital component, often overlooked.
A joined-up intelligence system is a prerequisite for joined-up engagement at the ICS level. It is essential to keep track of who is doing what - and to stop good intentions running into the sand.
If you would like to know more about the system that we are working on, please get in touch: info@patientlibrary.net
Tuesday January 26th 2021
Under-representing maternity
Patient safety in maternity services is a major concern at the moment, with the first report on Shrewsbury and Telford recently published, and the East Kent investigation ongoing. Both of those follow similar investigations and reports from Morecambe Bay and Cwm Taf.
The common thread throughout has been a failure to take seriously the concerns raised by women, birth partners and bereaved families. The harm persisted because patient experience was ignored.
In this context, it is worrying to hear of a decline in response rates for national maternity surveys. According to our featured report this week, "The response rates to the Infant Feeding Surveys, the CQC Maternity Surveys, and the National Maternity Surveys... have fallen with each successive survey". For the National Maternity Survey for example, the response rate has gone down from 67% in 1995 to 29% in 2018.
It is not just the overall response rate that matters. The paper states that "the extent to which the response is representative of the target population is key, regardless of the rate of response".
When the researchers looked at the characteristics of respondents, they found that "women were more likely to respond to each of the surveys if they were older, married at the time of registering the birth of their baby, born in the UK and living in less deprived areas".
Conversely, "response to the survey by the youngest women, women who registered the birth of the baby in their sole name, and women living in the most deprived areas has become relatively less likely over time". The authors note that "If this trend continues, women in these groups will become even more underrepresented in such studies".
The paper concludes that declining response rates "bring into question the viability of continuing to use the survey method to capture the experiences of postpartum women". It warns, however, that "such data are not routinely available from other sources and currently there is no better alternative method to collect large-scale population-based data".
A final observation is that "it is important to find strategies to halt the decline in survey response rates, particularly amongst underrepresented groups, and to validate the data collected".
Tuesday January 19th 2021
Vaccination - why hesitate?
The arrival and rapid deployment of the Covid vaccines is certainly a good news story. That does not mean, however, that the population as a whole is in favour of vaccination.
A December 2020 study by Oxford University found that 16% of the population are very unsure about receiving a COVID-19 vaccine, and another 12% are likely to delay or avoid getting the vaccine.
So who are the people who might not take up the vaccination offer? We need to understand them and their motivations, and to do so, we may need to avoid simplistic terms such as "anti-vaxxer".
Our featured report this week looks at how individuals’ vaccination beliefs and behaviours are formed - and where the opportunities lie to intervene in the interests of public health.
A good starting point is how people assess risk. With busy lives and limited time to seek out information, we all take mental shortcuts. That can lead to over-confidence about our ability to judge risks, and "omission bias" whereby we prefer not to act even when doing so is beneficial to us. In the context of vaccines, this can mean that people give disproportionate weight to the harms of receiving vaccinations and dismiss the dangers of not receiving them.
Some shortcuts, however, are closely tied to previous experience. Research shows that having been previously vaccinated is strongly linked to subsequent uptake of vaccines. So one tactic could be to turn vaccination into routine behaviour that requires less deliberate planning, while simultaneously lowering perceptions of risk through continued experience of vaccination without adverse effects.
Another issue is that vaccination behaviour is often considered to be a question of individual beliefs and perceptions. But people are social animals, so we need to understand social belief formation, including cultural and political drivers.
Broadcasters and publishers have a role in this. The authors state that "the media often chooses not simply to report expert knowledge of risk but to simplify and sensationalise it by setting up debates about responsibility and blame".
Social media can be seen as a problem in this respect, but it could have a positive influence: "As people like to self-select who they want to spend time with, those who vaccinate might associate more with other vaccinators which can create a clustering of vaccination attitudes where individuals start imitating the behaviour of others".
The paper finds that "discussion to date has been overly focused on the individual, and often underestimates the role of cultural and political situations and other social drivers". It says that "to deal with the issue of vaccine hesitancy we need to develop interventions that take social belief formation and maintenance into account".
Tuesday January 12th 2021
Read, learn and share
2020 might seem like a year we would all rather forget. But for our small team at the Patient Experience Library, it was a good year, with signs of a real shift in how patient experience is perceived.
Quote of the year was from Baroness Julia Cumberlege, in her First Do No Harm report. She said that patient experience 'must no longer be considered anecdotal and weighted least in the hierarchy of evidence-based medicine'. It is a powerful statement, from a highly respected advocate for patients.
We are determined to push patient experience up the evidence hierarchy, and with the help of some equally determined people over the last year, we have made great strides, which you can read about on page 2 of our latest Patient Experience magazine.
We are not the only ones making good progress in this area. On page 3, we hear from Jo Hughes, co-founder of the newly established Harmed Patients Alliance. The loss of her daughter Jasmine ten years ago has left her acutely aware of the need for openness and compassion when things go wrong in healthcare. She reflects on the need to reframe the duty of candour, and calls for a restorative justice approach in the aftermath of medical harm.
Laila Hallam on page 4 considers how clinical perspectives and patient perspectives are two sides of the same coin. The fact that "patient stories" are from only one perspective does not make them less true. They could be contributing to healthcare's body of evidence but, she says, as long as they remain seen as "anecdote", the evidence remains incomplete.
The magazine also includes our usual round up of the latest and best in patient experience research, and we have tempting discounts on some excellent forthcoming training and conference events. Read, learn and share!
Tuesday December 15th 2020
Ockenden's silver lining
The Ockenden report on maternity services at Shrewsbury and Telford could be seen as par for the course in a year that has been full of bad news. The pain of the families can barely be imagined, and we can only hope that there is some relief for them in knowing that the truth is finally starting to come out.
But is there any good news from the Ockenden review? Our answer is a clear "yes".
The review gives us cause for hope because it nails the myth that in our evidence-based healthcare system, only some types of evidence are worth having.
NICE - the National Institute for Healthcare Excellence - offers clinical guidance, drawing on "the highest quality and best available evidence". But none of that was able to prevent a potential 1,862 cases of harm stretching over a period of years.
The Care Quality Commission regulates healthcare providers, based on rigorous, evidence-driven inspection processes. But none of that was able to detect the scale or severity of harm occurring at the Trust.
It was families - with no formal methodology, no analytical rigour, and no peer review - who were able to reveal the truth about the failures in maternity care. In the end, patient feedback - so-called "anecdotal evidence" - proved more reliable than any other form of evidence.
This is the third time this year that patients have shown that their evidence is vital. First it was Paterson. Then it was Cumberlege. And now it is Shrewsbury and Telford. In every single case, it was patient testimony, more than any other source of evidence, which revealed the shortcomings in care.
So we are hopeful that the tide is turning, and that the medical establishment must now start to take note of Baroness Cumberlege's demand that patient experience "must no longer be weighted least in the hierarchy of evidence-based medicine".
We hope that in 2021:
- NICE will make patient experience evidence part of its National Core Content.
- NIHR - the National Institute for Health Research - will help us to make a proper assessment of strengths and weaknesses in the patient experience evidence base.
- Health Education England will support our efforts to develop high quality accredited training for patient experience staff.
- NHS England will work with us on analytical tools that can cut through the morass of patient experience data.
All of this would indicate that NHS leaders were starting to take patient experience seriously - accepting it as a valid form of evidence, and moving it up the evidence hierarchy.
The Ockenden report reveals some terrible truths - but we don't have to despair. If we can use it to get patient experience seen differently, we can ensure that some good comes from the pain.
Tuesday December 8th 2020
Food is medicine
"Food is a form of medicine" says the foreword to this report. It is also an important part of patient experience - as shown by the inclusion of questions about food in various national patient surveys, and in the checklists for PLACE visits (Patient-led assessments of the care environment).
Unfortunately, "There is a poor public perception of hospital food; and frequent critical press coverage". The report states that "There is clearly scope for improvement".
The good news is that there are models of excellence: "hospitals of every type serving fantastic food, and without busting the budget". So how are they doing it?
The report points to four things that successful hospitals have in common:
1 - They adopt a ‘whole-hospital approach’. This means integrating food into the life of the hospital - treating the restaurant as the hub of the hospital, where staff and visitors eat together; the chef and catering team are as important as other staff members; and food is considered as part of a patient’s care and treatment.
2 - They have a chief executive who leads the change and understands the value of food and nutrition.
3 - They concentrate on the things patients and staff care about; good food, attractive environment, and a belief that the hospital they are in serves nutritious food at the best available quality.
4 - They have integrated multi-disciplinary working; bringing together catering, dietetics and nursing to help improve nutritional outcomes for patients, and to ensure that staff well-being is prioritised with nutritious food and drink available on-site at all times.
The report is mostly about patient experience of hospital food. But it makes two interesting comments about staff - one observation and one recommendation.
The observation is that "Staff on night shift are perhaps the most ill-served of all the groups we looked at, often eating from vending machines offering nothing healthy and nothing hot".
The recommendation is that "To ensure quality is driven from the top, it is important that boards and chief executives are regularly eating the same meal as patients. This could include serving patient meals at board meetings. Even better, boards should make unannounced visits to the wards and eat with the patients. This would help the decision-makers better understand the issues faced at ward level".
Monday November 30th 2020
The Life and Death of Elizabeth Dixon
It is hard to know how to respond to Bill Kirkup's report on the Life and Death of Elizabeth Dixon. It is by turns harrowing, desperately sad, and depressingly familiar.
The story, once again, is of a patient (this time, a baby) who died, and of bereaved relatives who had to spend years (this time, twenty years) fighting for the truth about what happened.
The report describes "failures of care by every organisation that looked after her, none of which was admitted at the time, nor properly investigated". That statement has echoes of the Morecambe Bay report, which found "a series of missed opportunities to intervene that involved almost every level of the NHS".
The report reveals "a cover up... propped up by denial and deception, which has proved extremely hard to dislodge over the years". That sounds like Gosport, where "Over the many years during which the families have sought answers to their legitimate questions and concerns, they have been repeatedly frustrated by senior figures".
The report says that "The fabrication became so embedded that it has taken a sustained effort... to demolish it". That mirrors the Northern Ireland Hyponatraemia inquiry, where investigators noted "how difficult it was to persuade some witnesses to be open and frank... concessions and admissions were extracted only with disproportionate time and effort".
A feature of this latest report which has been less evident from other inquiries, is how healthcare organisations were willing to sacrifice front line staff to protect their own reputations. Kirkup notes that "It is fundamentally unjust that the only person held formally responsible has been the most junior involved, who also happened to be both female and of an ethnic minority". This, he says, "is a sad indictment of an investigatory system that can be deflected so easily, and its convenience for others cannot escape notice".
There is a culture in healthcare that has to change - and it is not about individual staff, or individual organisations. It goes to the top.
It is about system leaders like NICE and Health Education England, whose National Core Content of evidence contains no dedicated component for patient experience.
It is about the Department of Health which, down the years, has failed to preserve organisational memory via an archive of patient experience evidence.
It is about NHS England, which knows that NHS staff struggle to make sense of patient experience data, but has not developed good analytical tools.
The failure of system leaders to take patient experience seriously was noted by Baroness Cumberlege in her recent report, First Do No Harm. She said that patient experience "must no longer be considered anecdotal and weighted least in the hierarchy of evidence-based medicine".
Kirkup's latest report says "It is vital that what happened acts as a catalyst for the significant changes that are necessary to ensure that this does not happen again".
Those "significant changes" should not be focussed solely on clinicians, with the usual litany of updating practice protocols and refreshing training. There also needs to be a focus on system leaders - NHS England, NICE, and Health Education England. They set the tone, they set the culture, and they need to set a lead in giving patient experience its rightful place in the evidence hierarchy.
Tuesday November 24th 2020
Strengthening patient experience evidence

"Patient experience must no longer be weighted least in the hierarchy of evidence-based medicine". So said Baroness Cumberlege in First Do No Harm - the recent review of large scale avoidable harm in healthcare.
It is an important and powerful statement - but how do we push patient experience up the evidence hierarchy? Unfortunately, there seems little urgency in government, whose response has been described by Cumberlege as woeful.
Rather than wait for an official response, Care Opinion and the Patient Experience Library have decided to act on their own initiative, and act quickly. We have joined forces to integrate search functionality across both platforms - linking over 60,000 written reports on patient experience with more than 400,000 direct comments from patients.
The rationale is simple: if we want patient experience evidence to be better used, the first thing we have to do is make it easier to find.
There are longstanding barriers to getting access to patient experience evidence. These have been documented in our recent Inadmissible Evidence report. Breaking through those barriers has been a key part of the mission of both Care Opinion and the Patient Experience Library. Both teams have spent years building better, faster and more transparent ways to hear from patients. But until now, both have worked separately.
The join-up, like the rationale, is simple. Enter a search term (eg "XYZ Trust") into Care Opinion and exactly the same term will be automatically entered into the Patient Experience Library. Users can switch between direct comments from patients, and structured reports and surveys relevant to their search term.
It works in reverse as well: a search in the Patient Experience Library brings results from both the literature and from patient comments on Care Opinion. Users can search by provider, by health condition or by service (eg maternity). Both platforms respond simultaneously to whatever search term has been entered, giving a two-way join up of direct comments and written reports.
The initiative brings together two tried and tested systems to create the UK's biggest public evidence base on patient experience.
Baroness Cumberlege has challenged healthcare to take patient experience evidence more seriously. Government seems to be taking its time to respond. But in the meantime, Care Opinion and the Patient Experience Library are providing the basis for a joined up response right across the NHS.
Tuesday November 17th 2020
More than bums on seats
"Public involvement is typically presented as being unquestionably a good thing in relation to healthcare" say the authors of this paper. But why do we want public involvement? What does it actually achieve?
The paper looks at how the "impact" of involvement is measured - particularly in health research. It finds plenty of confusion.
First there is the question of what is being counted. The authors say that measures which are easy to count, such as numbers of people involved, tend to be favoured. However, questions of how "involvement activities change power relations and empower the public, are largely not being captured".
Some of the confusion over measuring impact might come from the fact that "at least 65 frameworks have been developed for assessing the nature and impact of public involvement in health research". And uncertainty over the value of impact measurement might arise from the fact that sometimes, the main purpose is to satisfy funders. This can mean that impacts "get overblown in an attempt to secure further funding - a phenomenon referred to as ‘impact sensationalism’".
Underlying all of this are differences of opinion about what involvement is for. Some see it as "a means to the end of achieving better research". But "An alternative ‘democratic’ or ‘rights-based’ framing of public involvement... sees public involvement not so much as a means to an end (better research) but as an end in itself". As one commentator put it, 'Service users have not fought for a voice at the table merely to help improve the research process, but because they have a right to be there".
The authors carried out a historical analysis of National Institute for Health Research (NIHR) policy. This suggested that policy had moved from being rights-based (‘nothing about us without us’), to "empowering" patients and public to "inform research" in ways that are more amenable to measurement. As a consequence, they say, "questions about how public involvement might enable the sharing of power, who power is being shared with, and in what ways, are easily side-stepped".
The paper concludes that "We still know very little about whether and how public involvement changes power relations between researchers and the public, because this is rarely the focus of impact research". It calls for "public involvement as a social practice of dialogue and learning between researchers and the public: an end in itself, not merely a means to an end (at worst, measured superficially as ‘bums on seats’)".
Tuesday November 10th 2020
Calling the bluff
We'd like to start with a big thank you to everyone who responded so positively to our "Inadmissible Evidence" report last week. There was a huge response on Twitter, and a surge of visits to our website, with over 2,000 downloads of the document within the first 48 hours.
The response vindicates our observation (in the report) that "There are many, many health professionals who understand the value of patient feedback - not just as 'stories' or 'complaints', but as evidence". The same, of course, is true for patients and public.
Interest has extended right across the pond to Canada, where the highly respected Matters of Engagement podcast picked up the report and dug into the question of why patient experience evidence needs to be taken more seriously. Here's what podcast presenter Jennifer Johannesen had to say in her summing-up:
"[The Patient Experience Library are] choosing to be optimistic and keeping their eye on the horizon... they're doing that by showing what's possible.
From the healthcare side, though, I think the lack of inclusion of patient experience evidence didn't happen because of an oversight, or because someone forgot, or because they just didn't know. My main point is that systems that exclude or minimise particular voices aren't broken. They're functioning exactly the way they're designed to. Powerful or dominant systems and institutions work very hard to stay powerful and dominant.
So in this respect, it's not surprising at all that [the Patient Experience Library] have yet to convince the national health authorities to support a project that is seeking to elevate patient experience evidence to sit side-by-side with medical evidence.
In a way the Library is like a fly in the ointment, demonstrating that a few hardworking people on a shoestring budget can put something of value together despite being told repeatedly by various healthcare entities that it would just be too hard and expensive and complicated.
They're not just proving them wrong - they're calling their bluff."
We'll keep going because in the aftermath of Mid Staffs, Morecambe Bay, Southern Health, Gosport, Hyponatraemia, Cwm Taf, Paterson and Cumberlege, it has become painfully apparent that the old ways of looking at evidence are not serving patients well.
As Baroness Cumberlege said recently, "Patient experience must no longer be considered anecdotal and weighted least in the hierarchy of evidence-based medicine".
We appreciate the support we get from readers of this newsletter, and we are inspired by our joint working with groups like National Voices and Care Opinion and the Heads of Patient Experience network. And we are sure that sooner or later, the NHS - at the institutional and system level - will begin to catch up.
You can listen to the podcast here, and download Inadmissible Evidence here.
Tuesday November 3rd 2020
Inadmissible Evidence
2020 is seen as the year of coronavirus. But it has also been a year of large scale avoidable harm in healthcare.
The report on rogue breast surgeon Ian Paterson was released at the start of the year, followed by the Cumberlege review of harms arising from pelvic mesh, sodium valproate and Primodos. In both cases, women's voices were ignored and suppressed over years, even decades.
In the meantime, a huge investigation into maternity deaths at the Shrewsbury and Telford NHS Hospital Trust continues, while a similar investigation has started at the East Kent University NHS Foundation Trust. In these places too, the voices of patients and bereaved relatives appear to have gone unheeded.
Against this background, our latest report asks why healthcare seems unable to accept patient feedback as a valid form of evidence.
NHS strategies emphasise the importance of "person-centred care" - and at a one-to-one level with patients, staff offer deeply personal and compassionate care. But the cases listed above - along with Mid Staffs, Morecambe Bay, Gosport and more, are signs of an institutional culture that finds it hard to hear concerns raised by patients.
The report points to a double standard which takes medical research seriously, while dismissing the experiences of patients as "anecdotal". We call for steps that would strengthen evidence-based practice and ensure that the patient voice is better heard. These include better research prioritisation, improved analytical tools and a professional learning infrastructure for patient experience work.
We continue to do all that we can to help put patient experience work on the same kind of evidence-based footing as clinical work. As we do, we are inspired by these words, from the Cumberlege review:
'Patients often know when something has gone wrong with their treatment. All too often they are the first to know. Their experience must no longer be considered anecdotal and weighted least in the hierarchy of evidence-based medicine.'
Tuesday October 27th 2020
Patients in waiting
Last March, Just as the national lockdown was starting, NHS England asked providers to postpone all routine surgery for at least three months. The decision made sense in a crisis situation, when hospitals were filling up with Covid patients, and the Nightingales were on standby. But what did the decision mean for the huge numbers of people who were waiting for care?
To find out, National Voices - a group of charities advocating for person-centred care, got in touch with us here at the Patient Experience Library. We carried out a literature search, drawing out hundreds of recent reports on people's experiences of being on hospital waiting lists. At the same time, Care Opinion trawled through posts to their website, looking for individual accounts of waiting for care. National Voices then added a third strand - based on deeper conversations with 'patients-in-waiting' via a carefully designed listening exercise.
The research shows that patients' journeys through the system are characterised by waiting/delays before the clock officially starts; stop-starts along the way; cancellations; changing goal posts and reversals, which patients simply did not understand.
For some, this led to speculation about "tactical management" of waiting list/targets at the expense of patient care. For others, a lack of control arising from fear of further deterioration or loss of income/employment severely curtailed their ability to "get on with one's life". Waiting affected family, work, and social lives.
Some people described "fighting" the system, while others talked of "giving up" and "not thinking about the wait" in order to protect themselves and keep their concerns in check. Some said that frequently they didn’t feel mentally or physically strong enough to make enquiries about the status of their wait and this meant remaining in an information vacuum for long periods of time.
The report points to opportunities to improve the experience of waiting. These can include pain relief and psychological support to deal with pain, as well as access to mental health support. Physiotherapy was suggested by some, while others asked for clear pathways to specialist advice if symptoms escalated. Clear communication between primary and secondary care was important, as patients often speak to their GP for support when waiting for specialist care. Alongside all of this was a need for information about employment and benefits.
These forms of support do not necessarily have to come from the NHS. A recurring theme was the importance of the voluntary and community sector, with support including helplines, information, peer mentoring, groups and policy information. People were often keen to get involved in charity work by volunteering and this also helped them to deal with their situation.
This is a comprehensive report, soundly rooted in wide-ranging evidence from credible sources. It has value in its own right, revealing the human experiences behind government statistics on waiting times and targets. But it is also a model for how to gain deep insight into patient experience by drawing on wide-ranging evidence from the literature, from online feedback and from face to face interviews.
Tuesday October 20th 2020
Insights from compliments
Patient feedback takes many forms. At one end of the spectrum are formal complaints which offer exclusively negative feedback. Channels such as the Friends and Family Test and patient surveys generate both negative and positive comments. And at the other end of the spectrum are compliment letters, which are wholly positive.
This paper makes the interesting point that while there are standardised procedures for handling and reporting complaints, and standardised approaches to survey work, there appear to be no common methods for receiving and analysing compliment letters. This, say the authors, is "symptomatic of a tendency in healthcare... to focus on what goes wrong rather than what goes right".
The exclusively positive nature of compliment letters is not their only unique feature. The paper makes the point that "patient and public involvement in healthcare is generally service initiated". Formal feedback channels (eg patient surveys) are based on clear organisational rationales, with written aims and objectives. Compliment letters, on the other hand, are patient initiated. They are written informally and spontaneously by people who have no stated aims and objectives. So what are the writers of these letters trying to achieve?
An obvious answer is that they are wanting to express gratitude. But there may be more to it than that.
By identifying the aspects of care that have gone well, compliment letters could be contributing to safe practice. Traditional "health and safety" follows a "Safety I" model, focused on breaches of procedure, and learning from mistakes. But "Safety II" recognises safe practice as something that emerges from organisational cultures, teamworking and personal relationships. These day-to-day working practices can be overlooked by staff, but patients who recognise and offer feedback on excellence can help "further the goal of understanding high-quality and resilient healthcare".
Secondly, compliment letters can offer insights into patients' own priorities for high-quality healthcare. In effect, patients are encouraging and supporting the healthcare practices they themselves most value.
The authors tested these ideas by analysing compliment letters, looking for instances where patients went beyond simply "acknowledging" excellent care, to "rewarding" or "promoting" examples of excellence. This would indicate compliments whose purpose was not simply gratitude, but an attempt to help improve services.
Part of the method was to identify the person(s) to whom the letters were addressed. Patients wanting to merely "acknowledge" behaviour might write directly to the staff concerned. But patients wanting to "promote" the behaviour might write to managers and chief executives. This could provide evidence that the written compliments were targeted at different audiences to achieve different effects.
The study found that there were indeed differences. Compliments focusing on personal relationships were sent either to the members of staff concerned or their superiors. Compliments focusing on clinical safety were most likely to be sent to senior managers. Letters to senior management also aimed at offering public recognition to front-line staff who had given excellent care.
The authors state that "Patient feedback data, despite vast amounts of data collection, have arguably had little impact on improving services". But, they say, "Compliments are credible, specific and narrative, and positive, which might make them a relatively effective route to improve quality".
Tuesday October 13th 2020
Missing a trick on Covid?
There are many ways to understand the effects of Covid-19 on people's health and wellbeing. We can look at infection rates, and mortality data. We can study outcomes from treatments, and conduct clinical trials for possible vaccines. We can be "led by the science".
All of this matters - but another way to understand how Covid affects people is to ask them. And not just in random ways, but systematically. That's because different people are affected in different ways. Age, ethnicity and pre-existing health conditions are important variables that can determine people's vulnerability to the virus.
The social and economic consequences of lockdown also have variable effects on people's mental health, as well as their susceptibility to loneliness, domestic violence and more.
There is an extensive body of evidence on all of this, and the Patient Experience Library has already amassed over 500 reports on people's experiences of the pandemic. By far the biggest contributor is the Healthwatch network, which has done sterling work under very difficult circumstances to gather wide-ranging evidence at the local level. Their reports shed light on the fine grain of local and even individual experiences, which tables of "science-led" statistics can never reveal.
Other reports come from health charities, polling organisations, think tanks and campaign groups. The work is of good quality and comes from credible sources. Taken together, it offers a body of evidence that could be an invaluable guide to policy and practice.
There is a problem however: a great deal of the literature is invisible to bodies such as the Department of Health and Social Care, and NHS England/Improvement. That is because it emanates from small organisations with small budgets and limited reach. It is published across hundreds of websites. It is what academics refer to as "grey literature" - ephemeral, poorly catalogued and hard to find.
Our rapid review of the evidence summarises the scale and nature of the evidence. It offers examples of reports that show how health inequalities are exacerbated by lockdown restrictions and reduced access to services. And it shows where the evidence base is strong, and where there are gaps that need to be filled.
We see a need for co-ordinated action to steer the evidence-gathering effort, and ensure that findings and recommendations are taken up. Some could be used immediately to fine tune the Covid response. Others could be built into plans for a post-Covid "restart" of health and social care services.
Covid responses that are led by the science are, of course, necessary. But responses that put the human experience alongside the science are likely to be better informed and more effective. Our review offers a starting point for a fully rounded, evidence-based response.
Tuesday October 6th 2020
Emotional journeys
We have all become familiar with the idea that the government's response to Covid-19 will be "led by the science". At the policy level that makes sense. But in all kinds of day-to-day healthcare - and particularly in person-centred care - people's emotions can be just as important as the cold hard facts.
In the autumn edition of our quarterly magazine, our contributors speak from personal experience, and do not shy away from the emotional aspects of healthcare.
Lynn Laidlaw outlines her journey from illness to eventual diagnosis and on into medical research. It is, she says, 'the emotions that stand out'. She wants to think about how we translate both positive and negative emotional experiences into learning to improve all co-production and involvement.
Francine Buchanan describes 'the overwhelming sense of lack of control or dread that I feel when walking into an emergency room'. Part of her response is to take detailed documentation which, she hopes, will give her some credibility when talking with clinicians. She recognises a power imbalance in the professional-patient relationship and suggests that power cannot be afforded to patients until their expertise, born of personal experience, is recognised and understood.
Lesley Goodburn talks about the shock of her husband’s sudden death from pancreatic cancer. The staff she encountered did not seem to see the vulnerable, frightened couple before them and so were unable to relieve their emotional and psychological suffering. So Seth’s legacy uses drama to help health professionals gain insights that they might not pick up from less 'emotional' forms of communication.
As always, we also bring you our top picks of the latest and best in patient experience research, with handy summaries of the key points. And we’re always keen to hear from our readers, so if you know of a standout report that we should be featuring, or if you want to submit a comment piece, get in touch!
Tuesday September 29th 2020
Gratitude in healthcare
Research suggests that there is a connection between staff experience in healthcare, and patient experience. The greater the wellbeing of staff, the more likely it is that patients will receive good care.
Staff wellbeing is not just about terms and conditions of employment. It includes how staff feel valued in their work. Patient feedback can have an effect on that, and expressions of thanks from grateful patients can help to boost staff morale.
This study explores gratitude in healthcare and finds that the expressions and the effects of gratitude are more complex than they might at first appear.
One example is "social capital". The idea is that "gratitude empowers and motivates recipients through strengthening social bonds, encouraging social connectedness, and predicting willingness to reciprocate". This, essentially, is how good staff experience leads to good patient experience and vice-versa. But this does not always work for all patients or service users.
The paper warns of "the problematic nature of gratitude when it exacerbates a lack of autonomy". This can happen for physically disabled people, for some of whom gratitude may be the only currency available: 'For those who are able-bodied, gratitude may well comprise a comfortable and unproblematic response to kindness, but for disabled people it can signify an unbearable state of perpetual obligation'. Interestingly, "people who had access to paid personal assistance tended to feel a greater sense of control, comfort, and autonomy than those constrained by feelings of shame and frustration when having to be persistently grateful for the goodwill of others".
Another example is gift-giving. Hospital staff will be familiar with small tokens of appreciation such as flowers and chocolates. But, says the paper, "gifts become problematic when a gift is given in anticipation of privileged treatment". There is a need for "special caution for gifts that arise 'out of the blue' before the doctor has done anything to 'deserve' them". The authors note that "Hospitals often channel donations from grateful patients and their families into philanthropic programs that seem, at first, to circumvent the compromising effects of individuals accepting gifts". However, "these initiatives (sometimes called 'grateful patient programs' in the United States) are not immune to exploitative tactics that can compromise trust in the doctor-patient relationship".
The paper looks at the wider context for these matters, noting that "civility in workplace culture has a definitive effect on retention, job satisfaction, and patient safety". However, "We found relatively little attention paid to gratitude as a component of civility in care settings...and this could usefully be explored in further research". One opportunity might be the Covid-19 pandemic. The authors observe that "Collective expressions of appreciation for health care workers in many parts of the world have been accompanied by increasingly politicized conversations in the mainstream and social media about what constitutes meaningful gratitude".
The paper concludes by stating that "On the evidence of this review, gratitude should be recognized as integral to the social relations that significantly influence what people think, feel, say, and do in relation to health care".
Tuesday September 22nd 2020
Patient Experience in England
"Listening to patients should not be seen as a chore, or a tick box" says Shaun Lintern in the foreword to this year's Patient Experience in England report.
Lintern has considerable form as a leading reporter for the Health Service Journal and the Independent, and as a persistent advocate for patient safety. So he knows what he is talking about.
His comments come in a year when health news has been dominated by Covid. But as he points out, this has also been a year which saw publication of the report on rogue breast surgeon Ian Paterson, and of the Cumberlege review of harms arising from pelvic mesh, sodium valproate and Primodos. In both cases, women's voices were ignored and suppressed over years, even decades.
Happily, there is also plenty of good news on patient experience coming out of this year's crop of surveys and studies. Patient Experience in England rounds up twelve months of reporting, and summarises key findings. As well as a blow by blow review of the national patient surveys, our thematic overview of recent research draws out cross-cutting learning on matters such as online engagement, patient safety and the evidence-practice gap in patient experience.
The Patient Experience Library is not part of the NHS, and we get no funding for our work. But we are sustained by the enormous goodwill of our many friends and supporters, whose advice, encouragement and moral support give us the stamina to keep going. One of those is Shaun Lintern, to whom we'll give the last word:
"Patients have the lived experience that doctors, nurses, managers and politicians need to hear. Their concerns need to be acted on."
Tuesday September 15th 2020
Is everybody appy?
'The past decade has witnessed an explosion of mental health (MH) smartphone applications (apps)', according to this study from the United Sates. It states that 'More than 10,000 MH apps are available for download, offering features such as symptom and behavior tracking, diagnostic screening, psychoeducation, and relaxation and mindfulness exercises'.
However, analysis of depression app trials has reported a dropout rate of almost 50%, and a median daily engagement rate of 4%. These findings, say the authors, 'highlight a striking mismatch between the degree of enthusiasm, effort, and capital being dedicated to MH app development as compared to the extent of our knowledge regarding apps’ effectiveness and their potential for sustained use'.
The study looked at factors that could affect take-up and use of apps. These included the following:
Relative advantage: Do MH apps demonstrate an advantage over pre-existing modes of care? This matters because 'If patients, providers, or healthcare systems do not see the added value of an app, they will not use it'.
Useability: Here, simplicity is key. In fact, say the authors, 'the first question to ask is whether the complexity of an app is needed at all... many app functions can be achieved through simple text messaging'. In spite of this, 'MH apps often feature dense sections of psychoeducational text, multiple fields requiring users to type in their thoughts or daily activities, and a lack of dynamic features... MH researchers are attempting to squeeze complex behavioral therapies into patients’ pockets without adapting them to an app context, and it is often not working'.
Recipients: The paper states that 'recipients of an innovation are central in determining successful implementation'. This depends partly on values and beliefs: recipients 'may think that apps are impersonal, contain unreliable information, or do not have proper privacy regulations'. But it is also about skills, knowledge and resources: 'MH apps serve no purpose if users do not own a smartphone or do not know how to download or use an app'. And importantly, 'ownership of a smartphone is not a sufficient predictor of successful app use. For those with limited data plans, the decision to download an app may mean sacrificing other functionalities on their phone and can therefore be a considerable barrier to use'.
Context: This is also critical. User ratings influence the order in which apps are presented in online app stores. But '72% of the 29 most popular depression apps contained no information regarding suicide prevention, and some of these apps contained potentially harmful negative content'. The authors remark that 'The current lack of app store regulation is striking'. Within healthcare systems, commitment to sustained MH app use requires investment to train staff and patients, provide technical support, and keep apps updated and/or compatible with electronic healthcare records.
The paper concludes that 'the evidence base is still uncertain regarding the effectiveness and usability of MH apps'. Much, it says, can be learned from the successful apps we use daily; namely, simpler is better - and plans to integrate full behavioural treatments into smartphone form may be misguided. 'As the initial hype surrounding MH apps settles', it says, 'there is an urgent need for reflection and humility regarding the current state of the field in order to develop strategies that are realistic, grounded in evidence, cognizant of context, and more likely to result in successful implementation outcomes'.
Tuesday September 8th 2020
Do pain scales work?
'Managing pain can be extremely challenging' says this paper, because 'it is a private sensory experience'. While things like blood pressure and pulse can be objectively measured, assessments of pain usually depend on self-reporting by patients.
Healthcare providers try to understand pain levels by asking patients to rate their pain via tools such as numerical scales or face scales. Use of these is written into clinical guidelines, implying a belief that they can 'provide a meaningful measure to inform clinical responses'.
However, the study points out that laboratory-based efforts to demonstrate the reliability of pain scales 'neglect social and contextual influences outside the study environments'. For patients, these can include the effects of distress, confusion and anxiety. For health professionals, they can include scepticism, or habituation to seeing people in pain.
The study took the experiences of patients with Sickle Cell Disorder (SCD) as a way of exploring the usefulness of pain scales. SCD is characterised by chronic and acute pain, but patients do not always have visible signs of pain. Their need for opioid-based analgesics can lead to them being seen as 'drug-seekers'. And the fact that SCD is a 'racialised condition' can create problems with understanding and trust.
Patients’ coping strategies can also conflict with observers’ expectations of how people 'should' behave when they are in pain. For people with SCD, coping strategies can include socialising, watching television or listening to music. These patients, say the authors, 'do not adopt a visible sick role'.
One interviewee explained that he had been having painful episodes since he was very young, and so had become good at coping with it. For this reason, he did not ‘look as sick as other people’ when he was in pain, which translated into being discharged too early or not being admitted to hospital at all.
The study concludes that 'While very commonly used, pain scales have numerous drawbacks and are prone to profound social and communicative influences that may not be adequately taken into account'. There is, it says, 'considerable uncertainty inherent in scale use, and considerable scope for future work to explore this uncertainty and improve pain communication'.
Wednesday September 2nd 2020
Tech for health
What do we think of IT in healthcare?
The topic has been debated endlessly over the years, with arguments over matters such as digital inclusion versus exclusion, and the extent of public trust in NHS data security. On top of that are the frustrations of staff faced with clunky software and out of date hardware.
This report from the King's Fund revisits the issues in the light of Covid-19, which has prompted healthcare organisations to move services online "at a dramatic pace".
It is optimistic about the potential of digital technology to support ambitious transformation of care - for example by delivering more responsive care for people with unpredictable, cyclical conditions, or calibrating treatment more precisely for diseases that affect individuals in different ways. Another benefit is "the power of technology to stitch together different health and care services, allowing staff... to deliver joined-up care".
It is important, however, not to get too carried away with grand visions. The report makes the important point that "the success of digital innovation often depends on what might appear to be small details". Examples are the length of time it takes to log on to a system, how hard it is to rectify a small inputting error, or how long it takes to get through to the call centre if you forget your password.
Making digital innovation work means engaging in "iterative cycles of improvement to gain feedback from service users and test improvements". Early collaboration is vital, to enable creative thinking before solutions are pinned down. And when it comes to trust, "the solution lies, in part, in placing patients firmly in control of their own data and how it is used, with simple arrangements for opting in and out of data sharing".
"One overriding message", say the authors, "is that harnessing technology to deliver transformative change in health care is harder than it might initially appear". Their conclusion is that "The types of innovations most likely to spread are often those that fit within existing structures, making small improvements to existing ways of doing things rather than delivering transformative change".
Tuesday August 25th 2020
Making complaints count
"The current complaints system is not meeting the needs of the public." This stark assessment from the Parliamentary and Health Service Ombudsman sets the tone for a report which is unflinching in its critique of how NHS organisations handle concerns raised by patients.
Importantly, the report avoids dumping blame on complaints managers. It recognises that "Some receive commendable help from their organisations to do their job, but many others... receive limited access to training and are asked to address serious and complex issues with little assistance".
The PHSO points to three core system weaknesses:
- There is no single vision for how staff are expected to handle and resolve complaints. Too many organisations provide their own view on ‘good practice’ and staff are left confused as to which one to follow.
- Staff do not get consistent access to complaints handling training to support them in what is a complex role. When staff do get training, the quality and consistency of what is covered is variable.
- Public bodies too often see complaints negatively, not as a learning tool that can be used to improve their service. This often leaves complaints staff feeling that they are not valued or supported by senior leaders in their organisation and lacking the resources to carry out their role effectively.
The report sets out proposals for a more consistent and responsive complaints handling process that works for everyone. However, it warns that "change will not happen unless there is effective and inclusive leadership... to make the cultural transformation needed to recognise complaints as a valuable source of learning".
You can download a copy of the report via the library and you can comment on the new draft Complaints Standards Framework here.
Tuesday August 18th 2020
Stories vs surveys
How are we meant to make sense of patient feedback? There is so much of it, from so many sources, that that the task of extracting meaning can feel overwhelming.
This American study explores the problem, noting the additional difficulty that free text comments from patients might be "garbled, fragmented, or laden with multiple plausible inferences".
Perhaps because of this, some clinicians "remain skeptical about the accuracy of patients’ comments... and are uncertain about the actionability of this feedback for improving quality of care".
The temptation is to respond by channelling patient feedback into formal surveys, where questions are predetermined, and designed to generate quantifiable results. But, say the authors, patients' own stories convey what matters most to them. So "their focus often extends beyond the domains of experience assessed by conventional closed-ended survey questions". How, they ask, can patients’ stories "enhance improvement processes above and beyond what is possible using standardized survey metrics alone?"
The answer is that providers need to "invest in interpretive analysis in order to help clinicians understand, respond appropriately, and ensure maximum benefit".
In particular, they need to focus on the "actionable content" within patient stories - looking for "the who, what, when, and where of the event, as well as how the experience felt to the patient". This is more prevalent than might be imagined: "Overall, 80% of narratives contained actionable content. Fifty-six percent had multiple actionable events, and 17% contained four or more distinct actionable elements".
The study recognises that "coding and labeling of narrative content is labor-intensive if done by human coders". It notes the number of companies competing to sell machine reading and natural language processing programmes to healthcare providers. But it warns that "we know of no analyses... comparing the efficacy of human and machine coding, let alone the capacity of NLP to capture the nuances of actionability introduced in this paper".
There is still a need for "the skill and subtlety people... bring to the task - for example, the capacity to identify emerging patterns, cross-cutting connections, and nuances of language".
The paper concludes that "Patient experience surveys paved the way for patients’ experiences to be routinely measured". However, patients' stories "convey far more nuance, detail, and emotional content than do their survey scores. As a result, their collective narratives may fuel quality innovations that are far more patient-centered than those that rely on quantitative measures alone".
Tuesday August 11th 2020
Involve us now
As the lockdown eases, there may be a sense in some parts of society that life is starting to return to normal. Healthcare providers know differently. The immediate crisis might indeed be over - but its legacy is disrupted services and backlogs in routine care.
Patients, too, continue to be affected. Many are still shielding. Many are waiting for delayed appointments and procedures. Many have experienced a downturn in mental wellbeing through the lockdown.
All of this is playing out in the context of uncertainty about what the future holds - particularly in respect of a possible second wave of infection.
One organisation that is already looking ahead is the Academy of Medical Sciences, which recently published Preparing for a challenging winter 2020/21. The scoping document explores the implications of a possible Covid resurgence combined with the existing backlog of care and the added risk of a flu epidemic.
As might be expected from a medical sciences body, the report is loaded with graphs and tables, and packed with discussion of percentages and ratios. But the very first paragraph says this, "Mitigation strategies should not pose further disadvantage to the most vulnerable in society or the highest risk patients or communities. To maximise their effectiveness (and to ensure they do not exacerbate inequalities), preparations for winter must be informed by engagement with patients, carers, public and healthcare professionals... and, whenever possible, be developed through co-production."
The Academy's deliberations have been informed by a Patient and Carer Reference Group, which provided guidance on priorities and concerns for winter 2020/21. A series of public discussion workshops were also undertaken, and these led to publication of a companion report, giving the "People's Perspective". That report's opening paragraph states "We have rarely experienced more meaningful and genuine involvement than we have with this project".
At just three pages, the People's Perspective is concise and punchy, and very much worth a read. Its key message is "involve us now", and it calls on government to lead by example.
The Academy of Medical Science's report is described as a "rapid review". It is all the more to its credit that it did not exclude public involvement on the grounds that the processes are too slow.
The Academy has shown a government that aims to "follow the science" how an even better approach is to combine the science with knowledge gained from patient and public experience. Following both, together, will always give a better chance of deeper insight.
Tuesday August 4th 2020
Get the whole picture
We all know the importance of data for learning. In healthcare, good data can underpin policy making, clinical practice and the development of new drugs and treatments. So it is good to see government setting up an NHS COVID-19 Data Store to help "national organisations responsible for coordinating the response... to make informed, effective decisions".
The store contains an impressive array of datasets - and we must hope that the data is reliable. After all, a notable feature of the Covid-19 crisis has been the release of questionable statistics.
One way to both check the validity of the numbers, and to dig deeper for greater insight, would be to include qualitative evidence in the Government's data collection, alongside the numerical data.
This matters because it became apparent very early on that Covid-19 affects different people in different ways. Older people seem to be more vulnerable, as do people from Black, Asian and minority ethnic communities, and people with some types of long-term health conditions. Some people have the disease but show no symptoms at all, while others die. Some get ill and recover quickly, while others report a "long Covid" with persistent and recurring symptoms.
There has been plenty of evidence-gathering on peoples' experiences of the pandemic. We now have over 300 reports in the Patient Experience Library, and more come in every week.
The biggest single source (44% of reports) is the local Healthwatch network, which has been doing fantastic work in spite of the difficulties presented by lockdown. Through them we can learn about people's access to healthcare services, and about the effect on domiciliary care. Telehealth is another key theme, as is mental health and wellbeing during lockdown. Some reports cover the experiences of specific groups - examples include Turkish and Kurdish communities, people who are shielding, and residents in a domestic abuse refuge. The Healthwatch output demonstrates the value of a locally rooted patient voice initiative. Local authorities who have been cutting funds to the network should think again.
So why is this kind of evidence absent from the NHS datastore? Yet again, it is hard to resist the conclusion that patient feedback is simply not taken as seriously as other forms of evidence. Indeed, the NHS rapidly abandoned much of its own patient experience work as the lockdown began. According to this article in the BMJ, "This included stopping all work with patient participation groups (PPGs); stopping the collection and reporting of patient experience data; delaying responses to complaints; and stopping any local gatherings of patient groups". The author goes on to make the point that "How quickly and easily this work was stopped raises questions about how it is really valued".
A Government that wants national bodies to make "informed, effective decisions" needs to ensure that its data collection includes the patient voice. We need to understand people's experiences - in all their variety - of living with and through the pandemic. A Covid-19 datastore that fails to include experiential evidence seems worryingly incomplete.
A longer version of this article can be seen on the Understanding Patient Data website.
Tuesday July 28th 2020
Engagement under the radar
A great deal of work goes into the process of patient and public involvement in healthcare. Search the Patient Experience Library for terms like "involvement", "participation" or "co-production" and you will find a plethora of principles, toolkits and evaluations.
But while health professionals wrestle with the challenges of public engagement, some members of the public are getting on with it in their own groups and on their own terms.
Many online peer support groups communicate via platforms such as Facebook and Twitter - and because their engagement is informal, loosely structured, and (sometimes) private it can be hard for outsiders to tap into the knowledge that these groups co-create. They operate, in effect, under the healthcare system's radar.
This study looked at one such group, to see how participants interacted. BRCA is a gene mutation that increases the risk of developing breast, ovarian and other cancers. A BRCA Twitter thread has been running since before 2013, and is seen by the paper's author as a "resilient public" - able to sustain dialogue and mutual support over many years.
A key finding was that the Twitter thread was not simply an outlet for "patient stories". Information sharing was as important as storytelling, drawing from non-profit organisations and generalist news media, as well as traditional scientific sources.
Contributors to the thread adapted their communication styles to the inbuilt features of the platform: emojis allowed a wide range of expression, hashtags were used to enhance outreach, and when referencing sources, URLs replaced formal citations.
The more influential participants did not behave like social media "microcelebrities", reliant on relatable personas. Instead, they built influence by acting as gatekeepers of scientific information - regularly offering selected sources for others to find and read.
The study concludes that within the BRCA Twitter public, the "experiential" and the "expert" intersect. And it finishes with a question: how might professionals see social media as "a potential means to collaborate in both the integration of lay and scientific expertise, and the gatekeeping of quality information".
Tuesday July 21st 2020
Work as experienced
As the Shrewsbury and Telford investigation rumbles on, this report from the Healthcare Safety Investigation Branch (HSIB) sheds useful light on one aspect of safety in maternity care.
HSIB's national learning reports aim to "offer insight and learning about recurrent patient safety risks". This one looks at brain injury, neonatal death and stillbirth associated with group B streptococcus (GBS) infection. GBS is the most common cause of severe infection in babies within the first week of life, with a further 40% of GBS infections developing in babies aged 7 to 90 days.
A key focus for the report is the difference between "work as imagined" (how people think care and treatment is carried out), "work as prescribed", (how guidelines set expectations for care) and "work as done" (how patients are actually treated).
There were various reasons for differences. Sometimes, local practice was not in line with national guidance. Sometimes, "lack of staff availability" meant that antibiotic prophylaxis (critical for the baby's safety) was delayed or "missing". Sometimes "workload within the maternity unit" influenced decision making.
These are important factors in safety culture and practice, and it is good to see them highlighted in a national learning report. But the report appears to miss a further area that is vital for safety in maternity care.
The "work as imagined - work as prescribed - work as done" model seems to assume that "work as done" is the end of the line. Of course in healthcare, it is not.
Beyond "work as done" is "work as experienced" - by patients and, in this case, birth partners. Here and there through the report, it is possible to pick out references to patient experience. For example:
- "...mothers are not always provided with all the information recommended by the RCOG in relation to GBS... in some cases this limited their ability to make decisions relating to the use of antibiotics during labour and their timely attendance to the hospital."
- "The mother and father... felt that their concerns about getting into hospital in time were not heard."
- "When mothers make more than one telephone call for advice, they may not speak to the same clinician each time... for one mother the record made during the first telephone call was not referred to during her second telephone call."
Joining up comments like these, we can get the sense that the "work as experienced" by mothers might include inadequate information, a sense that anxieties are not being addressed, and difficulty communicating with clinicians at crucial moments.
But why do we have to do this joining-up ourselves? Why would a national learning report not be more explicit about the need to consider - and learn from - "work as experienced"?
We know that "patient voice" is critical to safety in maternity care. At Morecambe Bay, parents felt ill-informed, unheard and pushed from pillar to post. It was the same at Cwm Taf, and similar issues will almost certainly arise from the Shrewsbury and Telford investigation.
The HSIB report is useful and we must hope that its learning points are taken up. We must also hope that future HSIB reports can acknowledge that "work as done" is not where healthcare stops. "Work as experienced" is the ultimate end, and needs to feature much more prominently in safety culture.
Tuesday July 14th 2020
Do no harm
Two years ago, almost to the day, the report of the Gosport inquiry was published. We posted it on our website as a Featured Report, with the headline, "An end to anecdote". We felt that it was time to move on from a longstanding culture of dismissing patient feedback as "anecdotal evidence".
We have continued to argue the case via the BMJ, pointing to the use of language, to a double standard in evidence-based practice, and to issues with organisational culture.
Yet more evidence of the need for change has now emerged via the Cumberlege Review. Here is what Baroness Cumberlege has to say about "patient stories":
"The patient groups, some of whom have campaigned for decades, have been invaluable to us; well informed, knowledgeable, and research based. They never failed to ensure we learnt from them and were up to date with emerging developments. They are outstanding communicators and expert in the subject matter."
This is not mere politeness. Cumberlege is experienced and forthright, and she means what she says. And she also means it when she goes on to say that "The healthcare system... does not adequately recognise that patients are its raison d'etre. It has failed to listen to their concerns... and has too often moved glacially".
The words "healthcare system" are important. The NHS is full of dedicated staff who, at a one-to-one level with patients, offer deeply personal and compassionate care. But too often the system as a whole seems institutionally deaf to the patient voice. Evidence of this has been plentiful in recent years, in inquiry reports from Mid Staffs, Morecambe Bay, Southern Health, Gosport, the Hyponatraemia inquiry, and Cwm Taf. Shrewsbury and Telford will be next.
We are determined to be part of the solution.
We believe that patient feedback must be embedded into evidence-based practice. That is why we have built the Patient Experience Library as the national evidence base for patient experience and engagement. It is why we have given every NHS Trust in England a one-click access point for their patient experience evidence. It is why we have catalogued over 11,000 reports from the Healthwatch network, and it is why we continue to put out regular research summaries and updates.
We will carry on with the task of unearthing patient experience evidence and making it widely available. And we will continue to work with forward-thinking health professionals to get it better understood and used.
Monday July 6th 2020
Data plus stories
Our big breakthrough recently has been our one-click surveys and feedback tool - giving every NHS Trust in England instant access to key patient experience data, all on one page.
But understanding patient experience isn't just about data. It's also about the issues and insights that come from lived experience, and which can't always be picked up via questionnaires.
We have some great examples in the latest edition of our quarterly magazine, starting with Angela Cornwall, who explains why we need special arrangements for appointments for patients with autism and learning disabilities. This is not a plea for preferential treatment. It's about levelling patients like hers up - not levelling the rest of us down.
Liza Morton talks about routine hospital practices that can seem normal to staff, while feeling dehumanising for patients. Why do some services make patients wear gowns, when there is no medical need? If it's supposed to be for easier access for medical examinations, why are some patients "double gowned"?
Andrea Downing looks at the vulnerability experienced by groups of patients who gather online for peer support. In medicine, confidentiality is sacrosanct. But it seems that some online platforms have no moral qualms about taking patients' data - with or without their knowledge - and selling it on.
We're on a mission to make patient experience an integral part of evidence-based practice. So we continue to seek out and catalogue hundreds of documents every month - and our magazine brings you our top picks of the latest and best, with handy summaries of the key points.
Monday June 29th 2020
Tackling health misinformation
"Over half of the disease burden in England is deemed preventable", says this report, "with one in five deaths attributed to causes that could have been avoided". It notes however, that progress has stalled on reducing the number of people with preventable illness, and that compared to other high-income countries, we are underperforming.
The authors call for a paradigm shift in prevention policy - from interventions that "blame and punish" to those that "empathise and assist". Regressive taxes and bans have not, they say, delivered the transformation required.
Key to any new prevention strategy is the online information environment. Over 60% of British adults use the internet to check symptoms or self-diagnose, with the NHS website considered to be the most trustworthy. There is also, however, a "pernicious prevalence of false information". Polling shows that less than half of the population believe obesity is linked to cancer (misinformation), while over a third either agree that vaccinations can cause autism, or say they don’t know (disinformation).
The report states that the Covid-19 crisis shows how rapidly disinformation spreads. A poll revealed that nearly half (48%) of all British people had either seen or been sent "fake news" about Covid-19, online since the outbreak began. In addition, almost two in five (17%) said they did not know whether they had come across fake news, suggesting that the ability to identify and report the spread of misinformation is less than perfect.
In this context, health education, on its own, is insufficient. We need to build health literacy (people's ability to understand health information), and work towards the goal of patient activation (enabling people to exert control over the determinants of health).
The report makes a series of recommendations, including the introduction of a permanent "disinformation unit" to correct false information and help shape public health narratives.
The authors conclude that "New technologies have created opportunities to reach wider audiences, but ... It is also clear that the NHS and health sector more broadly need to take a more proactive approach. As an extremely trusted source of health information, it is imperative the NHS stays ahead of the curve".
Monday June 22nd 2020
One-click data access

Last year, a report from the Health Foundation looked at quality measurement - including patient experience - across a range of healthcare services. It described a "measurement maze", with numerous national bodies presiding over data collection. The data was "hard to locate online, with multiple spreadsheets to choose from and large Excel workbooks to download and navigate".
We thought that sounded all too familiar. The patient experience corner of the measurement maze is a tangle of datasets emerging from the Friends and Family Test, CQC patient surveys, NHS England patient surveys, complaints data, and more. One recent study identified no fewer than 37 different types of patient feedback on offer to staff within UK hospitals.
As we thought about the measurement maze in patient experience, we started to wonder about clearing a path through it.
We set ourselves a challenge: what if a Chief Executive of a Trust said, "I want all the patient experience data for this Trust and I want it now". We wondered whether it would be possible to respond to a request like that with just one mouse click.
Developing the solution took months. We had to trawl endless CQC and NHS England web pages, working through out of date pages, broken links, and poor navigation. Then we had to download vast spreadsheets and plough through complicated layouts. Finally we had to find a way to organise all the data such that every Trust could get all its data with a single click.
We have now achieved exactly that - but we want to go further. Because this is not just about speed and convenience of access. It is also about insight - so we have also developed one-click cross-referencing, to pull out common themes across the survey data.
We think there is more to do. We are keen to hear what you think of our surveys and feedback tool, and whether it could do more. Please feel free to try the tool (open access) and let us know what you think, via info@patientlibrary.net .
A full version of this account ("Hacking through the Measurement Maze") is available via BMJ Opinion
Tuesday June 16th 2020
Covid worse for women
Medical evidence seems to indicate that men are at higher risk from Covid-19 in terms of serious illness and death. So we might imagine that they would be more concerned than women about the virus, and its effects on society and the economy. But not according to this study.
The survey explored how the public experience of coronavirus varies between men and women. Interestingly, it found that although men are more likely to contract Covid-19, they are less concerned about the disease as a whole than women.
Women are more likely to think the effects of the virus will be greater across various areas including the economy, public services and our system of government. This could be because in some very direct ways, women are more seriously affected than men. For example, one third of women responding to the survey said that their workplace had closed, against one quarter of men. And respondents in general thought that working from home would be more likely to damage a woman's career than a man's.
Women have also been busier than men during the lockdown - partly by engaging in more spare time activities, but also with looking after friends, family and neighbours.
When it comes to mental health, women are finding it harder than men to stay positive - both on a day-to-day basis, and when thinking about the future. They may be less trusting of the government's handling of the crisis, and more likely to be anxious and sleeping less well.
The authors are careful not to speculate on the possible implications of all this, stating that "What this means for the future is uncertain". But they do note that nearly seven in ten women think the government acted too late, and that women are more uncomfortable about some aspects of returning to normal.
Tuesday June 9th 2020
Language vs experience
When patients give feedback to healthcare providers, the topic of "communication" often features prominently. That is because when people are feeling vulnerable, the way they are spoken to, and the words that are used, matter a great deal.
There can be few experiences that are more distressing than the death of a baby. So we need to think very carefully about how bereaved parents are spoken to. This paper looks at clinical terms such as "miscarriage", "stillbirth" and "neo-natal death" and finds that "These categorisations based on gestational age and signs of life may not align with the realities of parental experience".
The study explored the healthcare experiences of parents whose babies had died just before 24 weeks of gestation. Those interviewed "felt strongly that describing their loss as a "miscarriage" was inappropriate and did not adequately describe their lived experience".
Many "hadn’t realised properly that I’d have to actually give birth". One mother said "so in my head I was like... it’s going to be... just blood or whatever. But you know, I had to full on give birth". Another was reassured when her midwife compared her experience as similar to birth later in pregnancy as "that’s the majority of the hard work, it’s just the same, and you did really well".
Parents who were treated as if they were having a baby were more prepared for how their baby might look and found it easier to make decisions about seeing and holding their baby. In contrast, the use of the word "miscarriage" created different expectations: "My husband was actually really surprised when they put her in my arms, and he said, 'She’s a real baby. She’s even got hair'".
Memory-making was often extremely important to parents. Official certificates were a potent part of this memory-making process, but parents whose baby was born showing no signs of life before 24 weeks of gestation did not receive an official birth or death certificate. Parents were sometimes offered informal birth and death certificates. However for some they were a stark reminder that there was no legal documentation of their baby’s life. One said, "It’s just like insult to injury... it’s just a printed out bit of paper that the hospital gives you...".
The study refers to the National Bereavement Care Pathway's core bereavement care principles which highlight that "some parents may see late miscarriage and premature labour as being very similar even if some staff may view these as very different situations". And it includes additional recommendations for staff caring for parents experiencing loss between 20 and 24 weeks of pregnancy.
It concludes by emphasising that language in healthcare should "validate the loss of a baby, acknowledge the hopes and dreams associated with that loss, and prepare parents for the experience of labour and birth".
Tuesday June 2nd 2020
Experts of experience
Many readers will be familiar with the term "experts by experience". This is the idea that in a science-driven healthcare culture, we need to make room for the kind of expertise that comes from living with illness, alongside the expertise that comes from studying or treating it.
Equally familiar is the idea that experience of illness is personal. Two people might have the same long term health condition, but their lifestyle and treatment choices might be very different, and so might their ability to get the services they need. It is these personal differences, often affected by class, gender, ethnicity and so on, that can lead to questions of how "representative" experts by experience can be.
This wide-ranging paper considers whose lived experience is represented in healthcare, as well as how and by whom. It recognises that simply sharing an experience does not mean it will be considered evidence, or that the person sharing it will be deemed an expert. It goes on to ask how "experience" is converted into credible "evidence", and how specific pieces of evidence can then become an accepted part of a healthcare system's body of knowledge.
The paper identifies three factors that shape the likelihood of an experience being used to generate evidence and create knowledge. Firstly, whether the experience has been sanctioned by being shared through an official feedback channel. Secondly, whether the experience has been solicited by a healthcare professional. Thirdly, whether the experience has been sought with the specific intention of being used for a particular purpose. These, it says, serve as preconditions for an experiential account to be used as evidence in the NHS feedback landscape.
The process of converting experience into evidence and then into knowledge is, to a large extent, steered by NHS staff who gather patient feedback. They have the power to "shape what and whose experiences are incorporated, used and responded to and in what ways... Their work involves filtering, aggregating, collating and isolating patient experience as it comes in through the various sources".
These staff "develop expertise in... extracting and sharing... experiences within the specific institutional contexts of the NHS and the demands for evidence-based policy and practice". They are not so much experts by experience, as experts of experience.
The paper concludes that incorporating people’s experience into healthcare remains challenging. "Patient stories" can be powerful because of their subjective and emotive nature. But that also makes it hard for them to be accepted as reliable evidence, and patients often lack the resources needed to produce the kind of evidence deemed necessary by decision makers. The answer could be to recognise that as well as experts-by-experience, we need experts-of-experience.
Wednesday May 27th 2020
Beyond lived experience
Patient and public involvement (PPI) in healthcare is a well-established principle. In spite of that, practice remains variable. There are arguments over definitions, tensions over power dynamics, and questions of equality and inclusion.
One of the challenges, according to this paper, is "legitimacy". For example, "Some professionals do not believe in the value of experiential knowledge, or consider it legitimate only when public contributors are... connected to their particular patient group". This, say the authors, places public contributors in a "legitimacy double bind". Contributors who are supposed to speak for a group can be denigrated as "unrepresentative", while the evidence of those who tell only their own stories can be dismissed as "anecdotal".
The problem can be exacerbated when PPI is equated solely with lived experience. That is because "To be involved at the higher levels public contributors need to take on more strategic roles in determining healthcare agendas and directions". However, "In strategic roles, direct lived experience inevitably becomes less and less relevant to the work at hand".
In this context, the study sought to uncover how public contributors themselves define their legitimacy. It reports that "The most striking results related to the number of valuable roles the public contributors established for themselves, and the way these provided the internal legitimacy left lacking by government and funder mandates".
The paper describes nine distinct roles: lived experience, occupational knowledge, occupational skills, patient advocate, keeper of the public purse, intuitive public, fresh-eyed reviewer, critical friend and boundary spanner. Importantly, "All the public contributors played more than one role".
The legitimacy of these roles is based in a number of factors, of which "lived experience" is just one. Others were "knowledge and skills", "citizenship" (particularly in service of a greater public good) and the "outsider" status of public contributors.
The paper concludes that "The conflation of PPI with lived experience [presents] a challenge for public contributors and involving organisations alike". Instead, a broader view of legitimacy could "demonstrate the potential value of public involvement in settings where lived experience appears to lack relevance". The authors suggest that "all involving organisations could benefit from encouraging public contributors to undertake a wide range of roles".
Tuesday May 19th 2020
Taking kindness seriously
For Mental Health Awareness Week (18th-24th May) we thought it would be worth taking a look at this study of patient experience in inpatient mental health care.
It describes itself as "the first study of patient experience in acute adult mental health settings" and as such, it sets a very high bar for potential followers. At 111 pages, it is not a short read - and with its appendices, it weighs in at an intimidating 337 pages. But there is little in here that could be described as waffle, and a great deal that offers valuable insight.
It outlines the importance of visible changes in response to feedback: "When change was not observed, it disincentivised patients and carers from giving feedback and staff from collecting it, as they felt that there was nothing they could do about actioning it".
It explores links between staff experience and patient experience: "When staff were over stretched, demoralised... and frustrated at the lack of change that resulted from patient experience feedback, they stopped attempting to collect the feedback".
It looks at intrinsic versus extrinsic motivations for staff to engage with patient experience work, stating that if quality improvement is "driven by external drivers, such as the CQC, complaints and serious incidents, staff disengage from collecting feedback and develop a siege mentality motivated by fear".
The often confusing context for patient experience work is also considered: "NHS trusts are required to collect experience data from patients. Currently, there is little understanding of what data are most important, what processes are in place to collect them and whether such data make any difference to the quality of patient experience".
In fact the report covers so much ground that it is impossible, in this short summary, to do it justice. If you are short of time, it is worth at the very least looking at the discussion, integrated findings and conclusions in Chapter 9. And pages 85 - 88 offer a set of "rules" on how to collect, analyse and use patient experience data to improve the quality of care. (It actually says "...to improve the quality of care in adult inpatient mental health settings", but many of the rules could apply to almost any healthcare setting.)
The theme of this year's Mental Health Awareness Week is "kindness". One way to show kindness towards people suffering with their mental health is to take their lived experience seriously. This important study points to ways to do that.
Tuesday May 12th 2020
Patient data sharing - who wins?
The launch of the coronavirus contact tracing app on the Isle of Wight has - once again - ignited debate over the pro's and cons of sharing personal health data. While advocates of track and trace say that digital solutions are essential, privacy and human rights advocates are not so sure.
Liberty has proposed five key questions that we should be asking about government use of personal data linked to coronavirus. A Conservative MP has warned of the risk that "health trumps privacy". And the Financial Times reports that the creators of the app at NHSX "admit they are in uncharted territory".
Against this background, a briefing paper from the House of Commons Library makes for useful reading. It offers a comprehensive but concise summary of all the main points of the data-sharing debate, including legalities, practicalities and ethics.
It includes some lessons from (recent) history - not all of which inspire confidence in the state's ability to safeguard personal health data. These include the following:
- The suspension of the national Care.data programme, due to concerns over the opt-out system in place and over patient confidentiality. Following the review, the then Life Sciences Minister confirmed that Care.data was to be closed.
- A finding by the Information Commissioner that the Royal Free Trust failed to comply with the Data Protection Act when it provided patient data to Google DeepMind.
- An NHS investigation which found that none of the 80 NHS Trusts affected by the 2017 WannaCry ransomware attack had applied an advised Microsoft patch update.
The report looks forward as well as back - examining cross-border data sharing after Brexit. We learn that in any US-UK trade talks, one negotiating objective of the United States would be to "Establish state-of-the-art rules to ensure that the UK does not impose measures that restrict cross-border data flows".
In response, the UK Minister for Trade has said that "We would seek to review any rules in place to safeguard data... and ensure that they are not overly protectionist. We set up the pipework, but whether or not the taps are turned on is a matter for the regulators". Patients may or may not be reassured by this.
As always, we need to remember that personal data is the personal property of patients. It is shared with clinicians on the long-standing principle of confidentiality. Any wider sharing - with government departments, with foreign governments or with private enterprise - must be on the basis of democratic debate and informed consent. In the rush to react to coronavirus, the patient and public voice must not be steamrollered.
Tuesday May 5th 2020
Lived experience under lockdown
"Aside from the tragic loss of life", says this report, "we know that coronavirus, and measures to reduce its spread, is impacting on the health and wellbeing of millions of people in the UK, and changing the way they access care and support".
It seems that some people are nervous about accessing healthcare settings where the risk of infection with coronavirus is higher. Others feel that their problems are not important enough to merit treatment when there are other, more urgent, priorities for the NHS.
The study aimed to explore the knock-on effects of coronavirus for health and wellbeing in the UK by understanding the experiences of people whose care has been disrupted. It is based on interviews with 12 people in the week beginning 20th April, just after the second 3-week lockdown period was announced in the UK.
It found that in choosing not to seek care, responsibility often trumps fear: "...the primary reason for delaying care was to avoid adding to the burden on the NHS". But the sense of responsibility was accompanied by anxiety. "Some participants were afraid that by following guidance to self-isolate and avoid risk, they would be discharged from services, or ‘sent to the back of the queue’."
Fear did also play a part. "One pregnant participant told us that part of her concern about asking for medical help was fear for her baby." Others "reported that they knew someone who had contracted the virus while in hospital for another condition, a powerful anecdote".
People whose care was cancelled or postponed could be left feeling in limbo: "the feeling of having built up to a potential resolution and having it snatched away was a source of disappointment, and where no timetable was available for it to be rescheduled, hopelessness".
An important learning point for health professionals is that in helping people deal with uncertainty, clear personal communication is crucial. "People appreciated being informed at each step of the process, having the time to ask questions and where staff acknowledged the unique situation we are all in."
The report also considers the practicalities of things like hospital visits, telecare, and the use of apps. For the latter, "telephone calls were strongly preferred, because they allow for questions, which is both practically and emotionally valued".
The report, which finishes with a series of recommendations, is a useful addition to the literature on patient experience - and one that might remain relevant for some while yet.
Tuesday April 28th 2020
Engagement under Covid
Every year, NHS England runs Experience of Care week to highlight the importance of patient experience, and to give people the opportunity to share ideas, case studies and best practice tips.
This year is no exception, and right now (28th April - 2nd May) is the opportunity to join in. But does it make sense to run Experience of Care week when the coronavirus has put a stop to almost all forms of "business as usual"? The answer, we think, is "yes".
It would be too easy, at a time of national emergency, to assume that patient experience doesn't matter - that we are all too busy with more important things, and that saving lives is the priority. But the emergency brings new challenges to all aspects of care, and for some of them, public engagement is an essential part of working out how to respond. For example:
- We need to find new ways to connect people with relatives in hospital, and to help bereaved families cope with the deaths of people they weren't able to be with.
- We need to work out how to enable visiting in care homes - and look for new ways to bring residents and relatives together.
- We need to understand how people with long term conditions are dealing with "self-management", at a time when appointments and medicines might be harder to come by, and anxiety and loneliness more pronounced.
Our featured report this week (from Australia) explains why public engagement in a time of crisis still matters. It offers handy tips on how to find "consumers" quickly, and tackles some of the practicalities of engaging with people while minimising face-to-face contact. A section at the end explodes some myths - for example, the idea that public engagement is too time-consuming and difficult at present.
The report does not ignore the challenges. However, it finishes with the observation that "Your consumer partnerships do not need to be perfect; the most important thing is that you try."
Tuesday April 21st 2020
Moving engagement online
With the lockdown set to continue for a while yet, videoconferencing is starting to become part of the new normal. So can patient engagement work - via committees, focus groups and so on, simply move into cyberspace and carry on? The answer, according to this report, is "yes but..."
"Yes" because the technology these days is sufficiently mature, and many people nowadays are familiar with the basics of social media and with platforms like Skype and FaceTime.
The "but", however, arises from the fact that hosting a business meeting online is somewhat different from chatting with friends or family after work.
A key difference is that business use can make far better use of the wide range of features that videoconference platforms offer. "Don’t assume that online meetings are the ‘poor relation’ of face-to-face meetings" says the guidance. "Online platforms allow for lots of different kinds of interaction, including the chance to use break out rooms, run polls, allow people to share their screens with each other, and to use ‘chat’ to comment and share responses." Hosts who are familiar with these tools have a much better chance of offering enjoyable and effective online engagement.
Planning and preparation are important too. The guide suggests opening meetings well in advance of the official start time to allow time for people to log in, and then sort out any problems they may be having with sound and vision.
If you want to share your screen, show powerpoint slides, move people to break out rooms, etc, it might be worth having someone to help. "Trying to facilitate, present and manage the technicalities is really hard - so splitting the roles - with a ‘presenter / facilitator’ and ‘technical support / producer’ working hand in hand really helps."
The guide offers further tips - for example playing music as people wait for the meeting to get underway, not stressing too much about bad hair days, and having a back-up plan for that crucial moment when the screen freezes or the video clip fails to load.
All in all, a handy guide for changing times and new ways of working.
Tuesday April 14th 2020
Patients at the heart of healthcare
Amid rising death rates and the opening of the Nightingale hospitals, it has been wonderful to see people finding new ways to offer person-centred care. Staff in full protective equipment have been sticking photos of themselves to their gowns, so that patients can see the person behind the mask. Other staff are using knitted hearts to connect bereaved relatives with patients who have died alone.
In the meantime, the day to day work of the NHS goes on, and in all sorts of settings, person-centred care matters as much as ever.
In the latest edition of our quarterly magazine, we hear from Michelle Sokol, who makes the important point that 'care' does not only happen in clinical settings. She looks at how regulators can also take a person-centred approach. 'Fitness to practise' involves judgements about whether clinicians are meeting the required professional standards. But, says, Michelle, those judgements must take into account the views of patients, relatives and carers.
Brooke Batchelor draws on her experience as a paediatric nurse to think about how we look after children. Sometimes clinicians and parents - with the best intentions - hurry or even force children through procedures that are distressing for them. Brooke suggests other, less traumatic ways to gain the child’s co-operation and stop them from spiralling into a fight or flight response.
Karl Roberts challenges another assumption - that care is a one-way process - provided by health services for patients. In his article, he looks at peer support, and how patients’ own knowledge and skills can be a source of all-round learning on how to develop person-centred care.
Regular readers will know that for us, the best learning comes from matching personal insight and experience with rigorous research. So this edition also includes a round-up of the latest studies on patient experience and involvement - many of which offer good news in these difficult times.
Monday April 6th 2020
Growing public satisfaction
Asking about public satisfaction with the NHS may seem unnecessary at a time when people routinely emerge from their homes to applaud the efforts of healthcare staff. But this survey, carried out before we had even heard of coronavirus, asks questions that are important for society and healthcare in the long term.
As an annual "gold standard" research exercise, the survey provides a rich time trend, adding a depth and context to the findings that, say the authors, no other measure of NHS satisfaction provides.
An encouraging headline is that after falling for the last two years, public satisfaction with the NHS rose significantly in 2019. Overall satisfaction was 60% - a 7 percentage point increase from the previous year. And while 42% of respondents thought that the general standard of care would get worse over the next five years, that was actually an improvement on the 51% who, in the 2018 survey, expected care to get worse.
The top reasons for satisfaction with the NHS were quality of care, followed by the fact that the NHS is free at the point of use, and that it has a good range of services. The main reasons for dissatisfaction were staff shortages, waiting times for GP and hospital appointments, and a view that the government doesn’t spend enough money on the NHS.
On the question of funding, recent government announcements of a new, and more generous five year cash settlement for the NHS could be key in explaining the upturn in satisfaction. It is possible, say the authors, that the public have understood (and believed) that NHS funding is increasing and that this in turn has fed through to an increased optimism about the future of the service.
It is important to note that the survey is about social care as well as the NHS. The satisfaction rating for social care remains "stubbornly low", at 29% - some way below any of the NHS services. Moreover, users of social care were more dissatisfied than users of any other service, with almost one in two (47%) saying they were dissatisfied. The report states that "governments have promised to ‘fix’ social care, but so far these have remained only promises, and there has been no actual reform of an increasingly challenged sector".
Monday March 30th 2020
Time for telehealth?

Covid-19 presents us with the need to look after very large numbers of ill people, most of whom must avoid face to face contact with health professionals.
While the lockdown continues, equally large numbers continue to need appointments for minor ailments and long term conditions. They, too, should follow NHS advice: "If you need medical help for any reason, do not go to places like a GP surgery, pharmacy or hospital".
So is it time for a large scale switch to telehealth?
The potential of telehealth has been discussed for a very long time: well over a decade ago, the King's Fund was asking people to think about it. More recently, the Now Healthcare Group has looked at how telehealth "can have a significant positive impact on GP pressure, medicine adherence and medicine wastage". According to them:
- Use of telehealth consultations obviated the need for an NHS GP appointment in 56% of cases
- Pre-triage through app technology could redirect up to 73% of patients to non-GP consultations (i.e. nurse or pharmacist), reducing pressure on primary care doctors.
- When patients were given direct control over repeat prescription ordering they only ordered 31% of total possible items, demonstrating the scope for the technology to reduce over-ordering waste.
Some objections to telehealth have been based on the idea that some of the people most in need of healthcare do not have access to IT or do not know how to use it. But consider this recent research by the Office for National Statistics:
- Virtually all adults aged 16 to 44 years in the UK were recent internet users (99%) in 2019.
- 95% of adults aged 16 to 74 years in the UK in 2018 were recent internet users, the third-highest in the EU.
- In 2019, the number of disabled adults who were recent internet users reached over 10 million for the first time, 78% of disabled adults.
That still leaves some for whom telehealth won't work. But for many - providers as well as patients - the barriers might not be as big as they have seemed. We'll leave the final word to a patient who, just this week, posted this comment on Care Opinion:
"Just had a video consultation on my iPhone with my own doctor and all I can say is that it was excellent. He sent me the link, which I downloaded, followed the instructions which were easy and success! The doctor was there!"
Monday March 23rd 2020
What now for patient experience?
The coronavirus pandemic has, according to some observers, led to a corresponding "infodemic" - a tsunami of facts, figures and advice, not all of which are consistent. We are not going to add to that.
Instead, we want to look beyond coronavirus, and to explore what it might mean for the future of patient experience work.
One thing is sure: in the current emergency, questions about "satisfaction with services" are likely to be seen as an unnecessary luxury. When the wards are full and people are dying, nobody is going to care whether you would recommend the service to friends and family. So the idea that "patient experience" equates to "customer satisfaction" may be about to hit a brick wall.
There is, however, another side to patient experience.
Looking beyond coronavirus, the chances are that we will continue to live in an ageing society, with continuing growth in long term health conditions. So we need to improve our understanding of what it is like to live with illness. Clinicians can't help us with that - only patients and carers can.
Returning to the short-term: part of our learning about the pandemic must be learning about the experience of self isolation and self medication. As hospitals develop treatments, and researchers race to find a vaccine, what are the rest of us learning about coping in our homes and communities?
We need to understand this because people's reactions to, and behaviour during, this crisis will affect disease progression far more than policy statements or clinical guidelines.
Perhaps, in a few months' time, the crisis will blow over and we can all go back to business as usual. Alternatively, we could take this moment to rethink what patient experience work is really about.
Is it time to ditch the "customer satisfaction" model? Time to give up on the Friends and Family Test? To move on from the large scale patient surveys whose results appear many months after the questionnaires have been completed?
Should we instead shift the focus to learning about people's ability to understand illness, manage self-medication, and cope with the social determinants that can make or break quality of life and even survival?
These are big questions and right now - at the start of the crisis - the answers may not be clear. But given that crisis is always a time of opportunity, it might be worth starting now to ask some big questions about the future of patient experience work.
Tuesday March 17th 2020
Hearing Survivors of Surgical Mesh
This report from New Zealand opens with the observation that "The use of surgical mesh, especially in urology, gynaecology and obstetrics surgical procedures has been a matter of local and international concern for some years".
Much of the concern was raised by women who had suffered harm from mesh products. But they were up against a healthcare industry whose "evidence was mired in a multimillion pound deal, industry funded research, and undisclosed conflicts of interest".
Part of the response in New Zealand was to establish a restorative justice approach to address the needs of those affected by mesh harm. The approach would enable storytelling, provide validation and help to rebuild trust.
Restorative justice is described as a process in which "those with a personal stake in a harmful episode come together... to speak truthfully about what happened and its impact on their lives... and to resolve together how best to promote repair and bring about positive changes for all involved".
Patient stories were gathered via Listening Circles, individual meetings and an online story database. From this, says the report, "a complex and nuanced picture of the harms and needs created by surgical mesh has emerged". Participants described
life-changing physical and psychosocial harms, including:
- Loss of trust in healthcare providers
- Injuries and needs rarely being acknowledged or validated, leaving some feeling desperate or contemplating suicide
- Erosion of dignity and grief over losses to physical wellbeing, relationships, identity, employment and financial status.
Mesh injury has also "rippled out through the lives of... families and loved ones. It has deeply affected the emotional wellbeing of partners, children, relatives and communities".
The report makes it clear that the listening process is not an end in itself. A section on "proposed actions" sets out a series of important next steps. Central to that is including "the mesh community and clinicians in transparent and inclusive dialogue in order to rebuild trust and secure lasting change".
As UK health services revisit their own approaches to patient safety and "just culture" it may be worth reflecting on how safety investigations are conducted. For the survivors and bereaved relatives from Morecambe Bay, Gosport, Shrewsbury & Telford and elsewhere, there may be healing to be found in the kinds of restorative justice approaches described in this report.
Tuesday March 10th 2020
Anonymity and power
This paper says that online feedback is "an equalising mechanism, enabling people to give feedback at a time of their own choosing, in their own words, often unmoderated and often anonymous".
But is anonymous feedback a good thing? Patients may want it because they "fear that being identifiable may compromise the care they receive if they make critical remarks". Healthcare professionals, on the other hand can "see patient anonymity as... a risk to the reputation of individual practitioners or organisations, given that anyone can say anything, no matter how unfair or damaging".
This, say the authors, "constitutes an ‘anonymity paradox’, whereby patients see anonymity as a prerequisite but professionals see it as a barrier".
This study explored anonymous online feedback via a series of interviews with NHS staff registered as "responders" for comments received via the Care Opinion platform.
It found that in general, staff understood why anonymity might be important for patients. At the same time, "anonymous feedback creates an unfamiliar and uncomfortable situation. [Staff] are encouraged to name themselves and engage in tailored, personalised conversation, but with a faceless, nameless other". It found that "In spite of themselves, [staff] may try to work out who someone is".
Sometimes, "the perceived unequal relationship and feeling of vulnerability can spark more problematic responses and feelings". The study reports that "Staff may...feel helpless, frustrated, unfairly attacked, and that their professionalism has been impugned with ‘no redress’".
Importantly, "Feedback on Care Opinion needs to be seen within the wider landscape of staff response to feedback of any kind, whether anonymous or not". The paper refers to other research showing that medical staff are "strongly supportive in principle of incorporating patient feedback into quality improvement work. Yet they also expressed a simultaneous view questioning the credibility of survey findings and patients’ motivations and competence in providing feedback".
Other research, on complaints (from known individuals) reveals similar defensiveness: "staff often characterised complainants as ‘inexpert, distressed or advantage-seeking’, described their motives for complaining ‘in ways that marginalised the content of their concerns’, and rarely used complaints for improving care".
The paper concludes that the ‘anonymity paradox’ "is at its heart a question of unequal power, risk and vulnerability" It suggests that "Staff used to engaging directly with patients and families... need support in dealing with anonymous feedback, and the uncomfortable situation of unequal power it may create".
Tuesday March 3rd 2020
Safety in mental health services
"Mental health services... often need to improve the safety of care", says this recent study.
It reports that "In the UK in 2017, the CQC considered over a third of mental health services deficient in terms of safety. Of particular concern were sexual safety and the use of restrictive practices such as restraint and seclusion". In spite of this, "Service user and carer perceptions of the safety of mental health services have not been widely reported".
The study, based on interviews with mental health service users and carers, found differences in the ways that safety was perceived. Carers were primarily concerned with physical safety, to prevent self-harm and suicide. Service users recognised physical safety issues, but also talked about psychological safety, and experiences within services that had led to fear and distress.
One such example is physical restraint, which might prevent self-harm but can also cause further psychological harm. "The trauma of experiencing restrictive practices was graphically described by participants."
In such circumstances, it can be hard for patients to raise concerns or complaints. One interviewee remarked that "If you are ill enough to be detained, you do not have the mental energy to start formulating complaints and pursuing a complaints procedure".
Communications in general were problematic, with carers expressing "frustration at not being listened to, especially about potential early warning signs that were likely to be antecedents to incidents".
Psychological harm can also come from a sense of being locked out of services. "Accessing help in a crisis had been universally inadequate, distressing and occasionally life-threatening for all participants."
Inadequate access can relate to practical difficulties: "one example... is crisis services with limited opening hours". But there may also be a kind of double standard operating: "Evidence suggests more assertive patients gain access to services in primary care, but in mental health services, assertiveness can hinder access to services with participants being seen as difficult".
All of this has particular relevance for an NHS whose Long Term Plan is steering it in the direction of personalised care. Choice is fundamental to personalisation, and "In other care settings, patients have the right to choose between care providers and can avoid certain individuals or services. For mental health service users however, this autonomy often cannot be exercised due to lack of treatment providers and threat of compulsory treatment". This, say the authors of this paper, makes it "even more important that if autonomy is overridden, safety should be assured".
Monday February 24th 2020
What matters in A&E
"Good patient experience is an essential indicator of high-quality health care and should be central to national performance measures." So says Healthwatch England in its opener to this report on patient experience in A&E.
However, "while the current four-hour A&E target does help illustrate performance across the NHS... the lack of detail means it tells us far less about the quality of care people receive and their overall experiences".
The report comes in the context of the Clinical Review of Standards (CRS) which is looking at updating and supplementing NHS performance targets. Part of the aim is to ensure that NHS standards "drive improvement in patient experience".
But Healthwatch England makes the point that "time alone does not dictate how people feel about their experience of A&E". Other factors that shape patient experience are:
- Quality of clinical care
- Quality and frequency of communication
- Staff attitude
- Whether the A&E is working well with others services such as NHS 111 and GPs
- The quality of the A&E facilities themselves
"This doesn't mean that waiting times are unimportant", says the report. It acknowledges that "national performance against the current target is a serious concern" that has "left the public lacking confidence in the NHS".
However, the challenge is to "do things differently, not just count things differently". And "if the CRS realigns targets around patient priorities [it] has a real opportunity to improve experiences for people in A&E".
Tuesday February 18th 2020
Racism in medicine
Our featured report each week is usually just that: one report, journal article or academic paper tackling one aspect of patient experience. But this week we have chosen to highlight a whole series of articles in a special edition of the BMJ.
The "Racism in Medicine" issue looks at the experiences of NHS staff, exploring inequalities in training and professional development, recruitment, and so on. But, commendably, the issue also covers aspects of patient experience and looks at how some health inequalities are embedded in institutional culture and practice.
One article discusses "Bibi-itis" - defined as "the belief that older Asian women express psychological distress through physical symptoms". This, says the author, is a form of "casual clinical stereotyping that can cause unrecognised bias leading to missed diagnoses, delayed treatment, and preventable unwanted outcomes".
Another, on ethnic disparities in maternal care refers to research showing that between 2014 and 2016 the rate of maternal death in pregnancy was 8 in 100,000 white women, compared with 15 in 100,000 Asian women and 40 in 100,000 black women. It quotes Christine Ekechi, a consultant obstetrician and gynaecologist, who says "People think of racism in an overt, aggressive way. But that’s not always what it is. It’s about biased assumptions - and we doctors have the same biases as anyone else.'
Neglect of older ethnic minority people in UK research and policy is the subject of a third article. This explains how ethnic health inequalities are undermonitored and poorly understood because of a lack of data and research. It says that "Policy efforts to reduce inequalities, improve population health, and plan for the provision of health and social care are therefore not adequately informed by evidence".
There are other articles, too, that are worth a read - and in an NHS whose Long Term Plan talks of wanting to "to develop and embed cultures of compassion", they should be read. As Zosia Kmietowicz, the BMJ's news editor puts it, "we can all play a part in reducing the disparities and inequalities faced by patients and doctors".
You can view the full BMJ Racism in Medicine edition here.
Tuesday February 11th 2020
Carrots, sticks and sermons
There has been a sudden acceleration of avoidable harms inquiries, with East Kent and the Paterson Inquiry coming hard on the heels of reports from the ever-widening investigation at Shrewsbury and Telford.
As always, a persistent theme is active obstruction of patients and relatives who tried to raise concerns.
The report of the Paterson Inquiry says that patients were "let down when they complained to regulators and believed themselves frequently treated with disdain". It describes a "capacity for wilful blindness" among "managers and those charged with governance", and says that the inquiry's findings are "primarily about poor behaviour and a culture of avoidance and denial".
Equally persistent are the calls for "lessons to be learned". Jeremy Hunt, for example, in his new role as Chair of the Health Select Committee, has called for an inquiry into the safety of maternity services, asking "Why do these mistakes appear to be repeating themselves?"
The answer to that question probably lies in the active obstruction of patients and relatives who try to raise concerns. But it could also come from the ways in which inquiries themselves frame their findings and recommendations.
This week's featured report looks at the ‘implementability’ of recommendations from the three inquiries of Ely, Bristol and Mid Staffordshire. Its premise is that "If one of the key reasons for an inquiry is to learn lessons and prevent similar events from reoccurring, recommendations must be implementable".
In order to avoid the Groundhog Day of repeated inquires and repeated failure to learn, every recommendation must comply with two basic requirements. First, it must be clear who the recommendations are aimed at, "for example ‘the Care Quality Commission (CQC) should...’ rather than... ‘consideration should be given to...’".
Secondly, actions must be described by reference to a clearly identified policy tool or operational mechanism. Typically, these would be "incentives, authority and persuasion; the economic, legal and communications families".
This may seem obvious. But analysis of inquiry reports shows that "The vaguest recommendations involve either a lack of clarity regarding who they are aimed at, or are seemingly aimed at everyone. For example, Francis’ first two recommendations that ‘require every single person serving patients to contribute to a safer, committed and compassionate and caring service’ may be seen as ‘everybody’s concern but no one’s responsibility’".
Vague recommendations such as these can be described as "sermons" - moral arguments that are not linked to "carrot and stick" policy tools and are not ascribed to anyone in particular. Worryingly, the analysis shows that "sermons are the main policy tool, accounting for some 89 per cent of Ely recommendations, compared to 66 per cent at Bristol and 63 per cent at Mid Staffordshire".
The paper concludes that "Given the large number of potentially responsible agencies, [inquiry] recommendations should be ‘active’ with a clearly identified agent and a clear policy tool or mechanism should be identified rather than a vague tendency to sermonise".
Monday February 3rd 2020
Person centred care needs person centred feedback
One year ago, the NHS Long Term Plan was published. It is wide ranging, but a theme that runs all the way through is 'personalisation.'
It says that one of the 'five major, practical, changes to the NHS service model' is that 'People will get more control over their own health, and more personalised care when they need it.'
That is a worthy ambition, but how will we know if personalised care actually works? The obvious answer is, 'ask the patients.'
Patient feedback is collected to drive quality improvement, manage risk, and gather insights that clinicians and healthcare managers might miss. Could it also be used to test whether efforts to personalise care are working?
This new report from the National Institute for Health Research (NIHR) does not address this question directly - but it does hint at some challenges.
The first of these, ironically, is that conventional feedback mechanisms are not personalised. The report describes 'procedure-driven, standardised approaches such as surveys and checklists [that] are too narrow'. In an echo of the Long Term Plan’s call for personalisation, it says that 'patient experience feedback is about being heard as a unique individual and not just as part of a group. This requires their experience to be considered as a whole, rather than reduced to a series of categories'.
Underpinning personalisation is the concept of 'choice.' But a second challenge is that patients cannot always choose how and when to offer feedback. 'In general, only sanctioned channels get monitored and responded to with feedback from other channels ignored.'
Personalisation also depends on dialogue. So a third challenge is a failure to close feedback loops, which leaves some patients feeling treated impersonally: 'The lack of organisational response to their survey feedback meant they perceived it as a ‘tick box exercise’ and they thought that their comments would not be used.'
So how could patient feedback mechanisms move closer to the Long Term Plan’s goal of personalisation? The answer could lie in a recent blog which calls for greater use of 'thick data' to support 'human-centred policy'.
Thick data is the kind that provides insights at an individual or group level, as opposed to 'big data' which offers cumulative evidence at a macro, often systemic level. The blog argues for the blending of big data and thick data - and perhaps this should be the direction of travel for patient feedback.
Conventional surveys and 'sanctioned channels' have their uses. But an NHS aiming for personalised care has to understand personal patient experience. And that might mean rethinking how it goes about getting feedback.
Monday January 27th 2020
Credit where it's due

Last October, we featured a report from the Lancet which analysed the health impacts of climate change.
It said that "The nature and scale of the response to climate change will be the determining factor in shaping the health of nations for centuries to come". However, "A lack of progress... threatens both human lives and the viability of the national health systems they depend on, with the potential to disrupt core public health infrastructure and overwhelm health services".
The report went on to say that "Ensuring a widespread understanding of climate change as a central public health issue will be crucial".
We took that as a cue to see what public engagement was going on around health services in respect of climate change. Our findings were disappointing: we reviewed four major national strategies on healthcare and found that none contained any serious reference to climate change, much less to engaging NHS staff, along with patients and public, in debate and action.
Just three months later, something has changed. It is encouraging - and impressive - to see the launch of a Greener NHS campaign to tackle the climate ‘health emergency’. An expert panel is being set up, but the campaign is calling on individuals and organisations to start work immediately on actions to cut carbon emissions and other environmental harms.
A Healthy Returns infographic offers handy ideas ideas for where positive changes can be made. And a Powerful Points library is being set up to enable people to submit their own facts and figures about sustainable development in health and care.
There is recognition that this will require leadership from the top: a linked website says that "Engagement and sustainability both need to be owned by boards and staff. Engagement and sustainable development programmes must also draw in service users, communities and the wider public, local councils, third sector and Health and Wellbeing Boards".
We will offer credit where it is due. Last October we were disappointed that health strategies appeared lacking on the crucial issues of climate, health, and public engagement. Now, right at the start of 2020, we take fresh heart from what looks like a surge of energy from NHS England. We'll be supporting this initiative - will you be joining in too?
Tuesday January 21st 2020
Fresh eyes on end of life care
"Caring for people who are dying is an everyday occurrence in acute hospitals" says this report from Hospice UK. "With around 46% of all deaths in England occurring in hospital, it is important that hospitals provide good quality, compassionate care."
The report describes a way of exploring the patient, family and carers’ experiences by walking through a potential journey - from the hospital car park, through the Emergency Department (ED), an acute assessment ward, a general ward, mortuary and bereavement services.
The Fresh Eyes team members consider their first impressions of the ward or service from the perspective of a service user, recording how it appears, looks, sounds and smells. They talk and listen to staff - trying to understand usual practice (for example how a deceased person travels from the ward to the mortuary). They also wander through public areas such as restaurant facilities, chapels, faith and spiritual spaces using available signage to self-navigate.
The method includes both objective and subjective perspectives, with feedback indicating where there were differences in views. Differences of opinion can be helpful in indicating areas which may need further attention.
Photographs are taken to help reveal unloved, often simple to fix areas - for example, dirty windows, clutter, out of date/unconsidered notice boards and poor signage. Generally, staff knew the issues, and the visit helped to raise the profile for necessary change. Many hospital trusts said it was relatively easy to fund improvements to mortuary visiting areas and bereavement suites through charitable sources.
This is an excellent report - clearly written and with plentiful photos to illustrate the kinds of "unloved" areas that busy staff perhaps stop noticing, but which might add to the distress of people at a sensitive and vulnerable time. A concluding "key actions" section offers helpful tips for improvement.
Tuesday January 14th 2020
Hearing is the start of healing
The winter edition of our quarterly magazine looks at patient stories, which are in big demand these days.
Board meetings of healthcare organisations often feature a patient - filmed, or in real life - recounting their experience of care. Annual reports carry mini case studies from (mostly grateful) patients. Proposals for service change are illuminated by testimony from patients who look forward to forthcoming improvements.
Of course, negative stories are also heard. They are channelled into complaints procedures or, better still, dealt with swiftly and compassionately by staff who know that a quick response is better for both patient and provider.
But what happens to the stories that don't fit the neat binary of satisfaction/complaint? How do we talk about the messy realities of living through illness, or travelling across "care pathways", or entering the strange world of "patient engagement"?
In this edition, we hear three such stories. Sue Robins wanted to write her way through her experience of cancer. But she discovered that her account did not fit the healthcare system's preferred narrative of illness, cure, and gratitude to healers. For her, uncomfortable stories need to be heard - without interruption, correction, or looking on the bright side. Hearing is the start of healing.
Tony Roberts looks at the story of "DNAs" - the shorthand for patients who "did not attend" their appointments. Healthcare professionals can see a DNA as a failure of motivation on the part of the patient. It can be frustrating and dispiriting. Patients, on the other hand, can see DNAs as a failure of motivation on the part of healthcare providers - to schedule appointments more sensitively, to consider transport needs, to understand the struggle to adhere to institutional routines. They too experience frustration and disappointment.
Finally, Douglas Findlay tells his story of patient leadership. His experience has been interesting, stimulating and challenging. But he wonders whether it really counts as leadership. He sets out some thoughts on how healthcare organisations could rethink their approach.
The magazine also contains our top picks from recent literature on patient experience and involvement.
Tuesday December 17th 2019
Status Quo Bingo
As 2019 draws to a close, and all you patient experience mavens head off for your Christmas parties, we thought we'd offer up a bit of festive fun from the Canadian comrades.
This comes from Christine Maika (@maikachristine) who had the great idea of asking the Twitterverse to come up with the kinds of reasons people give for not involving patients and public in discussions about healthcare. She compiled the best responses in a bingo card full of the cliches and timeworn excuses that will be familiar to involvement advocates everywhere.
You can play the "status quo bingo" by just drawing on your own memories of the things you might have heard people say. Or print the card out, and carry it with you to meetings and conferences in 2020. You'll have hours of merriment and laughter!
As Christine says, "Working in different ways means challenging the status quo. Calling BINGO on reasons not to engage people with lived experience will raise important questions, assumptions and might just lead you down a road to transformative change".
Thank you for reading this newsletter through 2019, and accompanying us on our mission to embed patient feedback in evidence-based practice. We'll be back with more news, views and top picks from the literature in 2020. Until then, Happy Christmas!
Tuesday December 10th 2019
Emotional labour in patient experience
"Connecting with patient experience is a crucial aspect of... quality improvement interventions", according to this newly published study. "However", it says, "there may be unintended consequences for health care service staff, particularly in sensitive areas of service delivery such as end of life care".
The study looked at the technique of "patient shadowing", intended to help practitioners see healthcare services from the perspective of patients and their families. The process enables them not only to see the problems with their service, but also to empathise from the perspective of the patient. Shadowing has been described as creating "a sense of empathy and urgency among caregivers by highlighting and clarifying the patient and family experience in a way that cannot be understood unless one 'walks in their footsteps'".
The researchers evaluated an improvement programme that included elements of patient shadowing and found that "the emotional power of shadowing was cited by staff... as initiating many transformative effects". However, they also found other consequences.
One of these was anxiety - particularly in respect of "putting colleagues under scrutiny". This was compounded if staff were being asked to do shadowing by more senior members of a team. Another was "resistance". For example, some staff expressed concern that patients may not feel comfortable with being observed, even though the assumption was largely unfounded.
The researchers observe that "Shadowing cannot be considered as a tool that is socially, politically or culturally neutral". Indeed, "Many varied social, cultural and political attitudes to shadowing were found among services: some staff felt surveyed or scrutinised by being shadowed by colleagues, whilst others reacted to shadowing as if it were thrust upon them".
The paper concludes that "Even though it is an intended consequence of shadowing to instil an emotional response... there was also potential for [shadowing] activities to intensify the strain upon staff, particularly those at lower levels of care service hierarchies". "This", say the authors, "emphasises the importance of organisational support for staff wellbeing when carrying out service improvements in this way".
Monday December 2nd 2019
What do patient surveys mean?
Shrewsbury and Telford, Morecambe Bay and Cwm Taf offer ample evidence of the need to pay attention to patient experience in maternity care. In every case, women and birth partners raised concerns, only to be met with institutional defensiveness and denial. The result was serious harm and avoidable death.
Efforts to understand experience of maternity care can help to underpin evidence-based practice. This can improve risk management and contribute to quality improvement. But what do we actually mean by "women's experiences of maternity care"? This paper says that the concept is ambiguous and ill-defined.
Many healthcare systems use large-scale surveys to explore patient experience - but there is no universally accepted definition of what is meant by "women's experiences of maternity care". So what is actually being explored via patient surveys?
Sometimes the basic concept is interpreted as meaning "women’s satisfaction with their maternity care". But, say the authors, measurement of "satisfaction" has limited usefulness for understanding and improving the quality of care. That is because surveys tend to extract high reported levels of contentment. This may be in part because of an "acquiescence bias" that may mask critical issues.
As satisfaction with care has generally been reported as high (regardless of the actual quality of care that was being provided), focus has shifted from the measurement of "women’s satisfaction with their maternity care" to "women’s experiences of their maternity care". However, the study finds that clear conceptual boundaries between these concepts do not exist. Consequently, it concludes, the concept of "women’s experiences of their maternity care" is philosophically immature.
The study raises important and intellectually challenging questions for patient experience staff. If we have no clear definition of "women's experiences of maternity care", what are patient surveys actually studying, and why? And once they are complete, what do the survey results actually tell us?
Monday November 25th 2019
Shrewsbury and Telford is not an outlier
Last week saw the leaking of a report into the deaths of mothers and babies at the Shrewsbury and Telford Hospital NHS Trust. The media response picked out revelations of a "toxic culture" that appears to have been at the heart of the disaster.
The culture included dismissive attitudes towards patients and bereaved relatives who raised concerns. There was, apparently, "A long-term lack of transparency, honesty and communication with families".
But denial and defensiveness in the face of patient concerns is not unique to Shrewsbury and Telford.
The Kirkup review of maternity deaths at Morecambe Bay said, "The treatment of complainants [included] defensive ‘closed’ responses, delayed replies, and provision of information that complainants did not find to be accurate".
Another review, into maternity care at Cwm Taf, found that "Women repeatedly stated they were not listened to and their concerns were not taken seriously or valued".
Similar observations run through inquiry reports about other health services, beyond maternity. These include the Francis report on the Mid Staffordshire disaster, and avoidable deaths reports from Southern Health, Gosport, and the Northern Ireland Hyponatraemia inquiry. They crop up again in Ombudsman reports such as Learning from Mistakes and Ignoring the Alarms.
And even in Trusts where there have not been official inquiries, there are cultural barriers to hearing the patient voice.
Commenting on the slow uptake of Learning from Deaths guidance, the CQC's Chief Inspector of Hospitals said recently, "we are still seeing the same issues persist in some NHS trusts... Issues such as fear of engaging with bereaved families, lack of staff training, and concerns about repercussions on professional careers, suggest that problems with the culture of organisations may be holding people back from making the progress needed".
Evidence repeatedly shows that a poor culture of responsiveness to patients who have been harmed is not unique to one or two "bad apples". It is widespread.
We need to recognise that the culture of any one healthcare provider does not arise in isolation. It is part of, and to some extent derives from, an overarching NHS culture. And the national culture also has a tendency to be dismissive of patient feedback. Evidence of this includes the following:
- We tolerate the use of dismissive language. Patient feedback is routinely referred to as "anecdotal evidence".
- We are comfortable with a double standard in use of evidence. Medical evidence is cherished, preserved and used. Patient experience evidence is treated as disposable.
- We are content to weaken the independent patient voice. Healthwatch, set up as a strengthened successor to the Local Involvement Networks, has seen its funding reduced by over a third.
We can tackle all of this. The term "anecdotal evidence" must be challenged wherever it is used. Directors of Nursing could lead on this. Patient experience evidence should be embedded in professional training, clinical guidelines and practice protocols - just as medical evidence is. NHS England has the Patient Experience Library at its disposal - it just needs to start using it. Healthwatch funding should be restored to its original 2013 level. That is a job for the Secretary of State.
None of this would be hard to do. But it all needs explicit commitment from people in leadership positions
A fuller version of this article, published by the BMJ, is available via the BMJ website
Tuesday November 19th 2019
The measurement maze
Measuring patient experience is never easy. Perhaps that is why there are so many approaches - including the Friends and Family Test, CQC and NHS England patient surveys, complaints processes, local Healthwatch reports, and more. But does the plethora of measurement systems create more confusion than clarity?
This report from the Health Foundation looks at quality measurement - including patient experience - across breast cancer care, children and young people's mental health (CYPMH) care and renal care. Its findings will resonate strongly with anyone who has to deal with the morass of patient experience data.
Interestingly, its findings on the often contentious Friends and Family Test are broadly positive. "While many interviewees acknowledged that it is a fairly limited tool, it was still seen as a valuable resource, without which there would be a considerable gap in measuring patient experience. Positive patient feedback, from the Friends and Family Test and other patient experience indicators, was thought to have significant value in terms of improving staff morale."
Other comments, however, reflect concerns about the value of data collection and use. A key question is what is being collected and why: "All the [data] we collect feels like a huge task and nothing happens to it... we’re told we have to collect it, but [we’re] not aware that it goes anywhere else."
Getting the data back in useable form is also problematic. The authors observe that where interviewees had experience of data feedback, many felt it was not quick enough: "it is painfully slow, which makes it irrelevant".
Even where the indicator data are released in a timely and comparable form, the interviews suggested that the potential usefulness for trusts, wards or teams was limited by the data being hard to locate online, with multiple spreadsheets to choose from and large Excel workbooks to download and navigate.
So how can we find a clearer path through the measurement maze? One suggestion is about analytical tools. "Any approach to enabling greater use of data for local improvement will need to consider the lack of analytical capacity within NHS organisations. [There are] gaps in training and development within analytical teams and in the infrastructure... to use and disseminate the results of analysis."
Another suggestion is more radical, involving a national overhaul of measurement systems. "Given the high volume of national indicators across multiple sources, and multiple national bodies sponsoring and using the data, there is a case for... streamlining and simplifying. It is currently not clear whether [anyone] maintains an overview of all the indicators in use across the system."
Encouragingly, interviewees across all five case study sites expressed a desire for more emphasis on, and greater measurement of, patients’ experience of health care services. For some, this would mean questioning whether what is measured also reflects what is important to patients.
Tuesday November 12th 2019
How helpful are involvement strategies?
Why do organisations publish patient and public involvement (PPI) strategies?
Presumably it is to help readers understand how and why the organisation carries out its involvement work. But, say the authors of this paper, PPI strategies can also have symbolic importance.
For example, "The presence of a PPI strategic document on a website or the production of this evidence on request is interpreted as a signal that efforts are being made". On the other hand, "The absence of documentation can be negatively interpreted... as a lack of intent".
So are PPI strategies just for show, or do they have practical value?
The authors used the National Involvement Standards (4Pi) framework to assess the extent to which various PPI strategies demonstrated principles, purpose, presence, process and impact. They found that not one met the full range of standards.
Further findings were that:
- Readers were required to work hard to disentangle the ‘why’ (strategic aim) and ‘how’ (plan of action) of involvement. There were limited, absent, and confusing aims that were rarely, if ever, logically linked to the proposed process of involvement.
- Documents differed in accessibility of language and content. Some were closer to Plain English and clearly explained NHS or organisational structures, but managerial and technical language with jargon and acronyms dominated the sample.
- Very few documents stated any meaningful detail about who was to be involved, for example by offering data about the local community or demographic information about the patient population across services. This, according to the authors, is especially concerning when considering issues of inclusivity, equity and equality.
The paper aims to "open the debate about the limitations of PPI strategic documents". It suggests an alternative approach - based on continually testing and learning from practice. Through small tests of change or Plan-Do-Study-Act (PDSA) cycles, professionals, patients and public can learn together about what works, how and why. The authors state that this "has the potential to release practitioners from the tokenistic cycle of monitoring and reporting... replacing it with a richer understanding".
Tuesday November 5th 2019
When PPI goes wrong
Patient and public involvement in healthcare is generally seen as A Good Thing. But what happens when PPI takes off in directions that neither health professionals nor some patient advocates might have expected?
This paper looks at the use of social media by groups seeking to promote an anti-vaccination message. Their tactics, according to the authors, include misinformation and anti-science sentiment. And these can be hard to counter because vaccination narratives can be complex, and the science may not be 100% clear cut.
Calm and rational dialogue is further compromised by notions of a "war" between people labelled on one hand as "anti-vaxxers" and on the other as uncaring professionals who are "in it for the money". Study participants described being "bombarded" on social media, and treading through a "minefield". They recounted crude language, vitriol and personal attacks.
So how do organisations promoting vaccine use deal with this particular type of patient and public involvement?
Using facts and evidence was important - even in the context of "anti-science sentiment". However, complex evidence needed to be explained in straightforward language.
Emotions matter too - so facts needed to be humanised with stories about the actual effects of preventable disease on real people.
It was important to create safe online spaces for information and debate - for example by quickly removing aggressive comments, and reporting offensive posts.
Responses had to be concise and respectful - and selective too, to avoid amplifying misinformation, or giving false legitimacy to some anti-vaccine views.
Alongside all of this, say the authors, is a need to publicly strengthen the pro-vaccination voice. Partnerships with other organisations played an important role in sharing and amplifying the collective voice. But the belief that vaccine-promoting organisations as a group were failing to adequately engage in the social media landscape was a source of frustration for some participants.
This is an insightful paper - focussed on the anti-vaccine issue, but potentially useful to guide online responses to other contested areas in healthcare.
Tuesday October 29th 2019
Over the rainbow
Take up of the Rainbow Badge across the NHS demonstrates the scale of health service support for LGBT patients and staff.
An important principle underpinning the Rainbow Badge initiative is that wearing the badge is not, on its own, enough. Participating providers are expected to develop practical measures for a better and more inclusive experience for their LGBT employees and patients.
We recently pointed to evidence of the need for this, and now a House of Commons committee has weighed in with further evidence.
The report on Health and Social Care and LGBT Communities says that "Good quality medical care is the foundation of our health and social care service", and that "Treatment that is respectful and inclusive is a cornerstone of these services".
However, LGBT people are often less healthy than the wider population, and tend to receive lower levels of care than non-LGBT people. Worryingly, the committee found that "Too often medical professionals focus on sexual health rather than broader health needs and differences when supporting LGBT people".
The report states that "too few health and social care providers are actively thinking about LGBT people when they plan their services". Furthermore, "senior leaders are not doing enough to ensure that LGBT-inclusion is hardwired into commissioning strategies. This problem filters all the way down to training, where medics of the future are not taught how to provide LGBT-inclusive treatment".
The committee concludes that "training currently sends the message that sexual orientation and gender identity are not relevant to providing 'person-centred care''.
Encouragingly, the committee heard many examples of good practice - and while these are not as widespread as they should be, they are seen by the committee as "a clarion call to the health and social care sectors to take up the work that some very dedicated and inventive individuals have already begun".
Tuesday October 22nd 2019
Cost effective feedback
Why do healthcare providers collect feedback from patients?
At a time when budgets are tight, and the NHS workforce is stretched, it is worth asking why time and money are spent on patient surveys, Friends and Family Test and all the rest.
Some providers might cite quality improvement as a motive. Others might talk about person-centred care. Still others might refer to patient safety. All of these would be good reasons for trying to understand patient experience. Especially so in mental health services, since Care Quality Commission patient surveys repeatedly show that people with mental health conditions generally have poorer patient experience.
Our featured report this week looks at how patient feedback is gathered and used in NHS mental health services. Worryingly, in the context of pressures on finances and staffing, it found that half of Trusts collecting patient experience data were not actually using it. A quarter of Trusts struggled to collect it at all, and only one quarter used patient feedback to support change.
There is of course an ethical dimension to this: why ask patients for feedback if it is not going to be used? But the study also raises questions of cost-effectiveness. The authors make the point that "For patient experience processes to be cost-effective for NHS providers, they need to find ways of collecting and analysing patient experience feedback and then using it to drive change".
Increased patient experience activity in mental health services can, they say, lead to reduced rates of violent incidents, faster discharge and improved staff morale. All of these could be seen in terms of cost-effectiveness. But to achieve outcomes like these, "it is necessary to act on feedback in ways that facilitate meaningful change".
The authors of the study are now looking to work with NHS providers to implement recommendations from their report and evaluate the organisational and clinical cost-effectiveness of collecting, analysing and using patient experience feedback to improve service quality.
Monday October 14th 2019
Burnout and bias
"Despite efforts on multiple fronts, substantial morbidity and mortality differences persist between white and black patients, regardless of their socioeconomic status and level of education."
This opener to our Featured Report for this week touches on the important topic of health inequality. The NHS Long Term Plan is peppered with references to health inequality, many of which focus on public health issues such as smoking, obesity and air pollution.
This American study, however, tackles a different aspect of health inequality, by looking at black patients' experience of racial bias in healthcare. Specifically, the paper asks whether resident physicians showing signs of burnout are more likely to display racial bias in their encounters with patients.
Burnout is described as "emotional exhaustion, depersonalization, and a decreased sense of efficacy". It is, according to the authors, common among resident physicians, and largely driven by work-related factors. These include work intensity, suboptimal supervisor behaviour, lack of flexibility and control, educational debt, and work-home conflict.
The study found that staff with symptoms of burnout did indeed display higher levels of racial bias towards patients. To understand the effect of this, it refers to previous studies, which have shown that "physicians with higher implicit bias toward black people demonstrate fewer patient-centered behaviors during clinical interactions with black patients; in turn, their black patients have greater distrust, have lower level of adherence to treatment recommendations, and are less likely to follow up".
In the NHS, it is well known that staff experience is closely linked with patient experience. So with an NHS workforce under pressure, the implications of this study are serious. Not just for the care and safety of individual patients, but also for more strategic efforts to reduce health inequalities.
As the report says, "given the high prevalence of burnout and the negative implications of bias for medical care, symptoms of burnout may be factors in racial disparities in health care".
Monday October 7th 2019
A climate for change
What is the biggest challenge facing UK health and social care? Ageing population? Funding? Workforce?
According to the Lancet there is a much bigger challenge: climate change.
It says that "The nature and scale of the response to climate change will be the determining factor in shaping the health of nations for centuries to come". However, "A lack of progress... threatens both human lives and the viability of the national health systems they depend on, with the potential to disrupt core public health infrastructure and overwhelm health services".
It goes on to say that, "Ensuring a widespread understanding of climate change as a central public health issue will be crucial".
We took this as a cue to see what public engagement is going on around health services in respect of climate change. Here's what we found:
- The newly published Public Health England Strategy 2020-25 contains just one reference to climate change in its 39 pages.
- The PHE Infectious Diseases Strategy has four mentions of climate change, but they all say much the same thing, and there is no reference to public engagement.
- The HM Government green paper, Advancing our health: prevention in the 2020s, has nothing whatsoever to say about climate change.
- To find climate change in the NHS Long Term Plan, you have to go all the way through to page 120, where it finally gets one mention in the Appendix.
This is surprising, because we know that some providers are working hard on environmental responsibility. There is a good summary here on how hospitals can cut greenhouse gas emissions, and an argument here for how the NHS can behave as an environmental anchor.
So - in a week that sees the start of the international climate rebellion, should healthcare services start thinking more about how they engage with the general public on these matters? The Lancet (as per the quote above) seems to think so. And so do we. And given that "the response to climate change will be the determining factor in shaping the health of nations for centuries to come", we hope to see NHS England and Public Health England encouraging much greater efforts to engage with patients and public on the climate emergency.
Tuesday October 1st 2019
Human experience matters most
'You can argue with figures and statistics, but you can’t argue with personal experience'.
These are wise words from a person who knows that in an NHS driven by targets and performance measures, it is still the human experience that matters most.
They come from Stephen Elsmere, who has used the NHS both as a mental health patient and as a general patient. He is also a carer. And on top of all that, he is an Experience of Care Partner with the NHS Leadership Academy. This is someone who knows what he’s talking about.
Stephen is one of a number of patients who are helping the NHS Leadership Academy to think about 'patient leadership'. You can read their stories in the latest edition of Patient Experience magazine, and can click through to a series of short videos where they outline their experiences and motivations.
We also hear from Jennifer Johannesen, who was the main carer for her son Owen throughout his childhood, up to his early death. Her book No Ordinary Boy is a record of her 'encounters with healthcare', and how those are uniquely experienced by a family like hers. Her account also shows that although measures matter, the true nature of 'patient experience' can only really be found through personal testimony.
Our third contributor is Liz Pryor, whose mother Anne Robson died in distressing circumstances in hospital. Liz converted her grief to action, setting up the Butterfly Volunteers, who offer companionship to hospital patients in the last days and hours of their life, particularly for patients who have no other visitors. It is an astonishing story of the power of personal experience to effect change.
All this, plus our usual round-up of the latest and best in patient experience evidence can be found in the autumn edition of our magazine. Enjoy!
Tuesday September 24th 2019
From setbacks to success
For some time now, health and social care services have been looking for "New Care Models" - propelled by the Five Year Forward View, Long Term Plan, Sustainability and Transformation Partnerships and the rest.
Patient and public involvement has played a big part, with views being sought through the usual mechanisms of public engagement and formal consultation. Often the discussions focus on what works best for patients, and how services can be made better for more people.
This American study works from the other end. The authors realised that a focus on success can sometimes mean missing an important part of the story: what innovators learn when things don't work out as planned. As they see it, healthcare leaders need to understand that setbacks and failures are inherent to innovation. Rather than being feared by people designing new care models, they should be seen as an opportunity to learn.
Fundamental to understanding setbacks is understanding patient experience. As the paper puts it, "When refining a new care model, examine which patients don’t benefit".
One example was a programme to reduce avoidable hospitalisations among older adults. This sent advanced practice nurses into hospitals and patients’ homes during transitions - such as after a major illness or surgery - to help coordinate care and offer services. But the model only worked for some patients, not all.
Discussions with patients and families found that having the same nurse practitioner visit patients in the hospital and their homes was pivotal because it engendered trust and led to clearer communication about their goals. What had appeared to be a design flaw in the care model was actually an issue about personal relationships.
The paper gives other examples, but makes the point that learning from failure is not always easy. According to one contributor, "One of the challenges of deliberately looking for blind spots is that many health care organizations haven’t developed the discipline for doing so". Crucially, "You need to have a culture where people aren’t going to be slammed for failing".
People are key - as shown by the comment that "The models are one-third of the story. The people who operate within the models are two-thirds". This can require fresh thinking because some healthcare providers tended to focus narrowly on medical risk when introducing new care models. But once they began to consider social as well as medical risk, they began to gain greater traction. For example, one organisation partnered with a food bank to prepare nutritious meals for heart failure patients who lacked social support.
Ultimately, developing new care models means that "You have to experiment with innovative approaches and recognize instances when what you’re doing now just won’t get you where you will need to be in the future". And judging what works is not just a matter for clinicians. "We also need to consider what’s important to patients - how do they define success and failure?'
Tuesday September 17th 2019
Why patients miss appointments
Non-attendance for appointments increases the cost of delivering care, reduces available appointments and increases waiting times for other patients.
It also has consequences for the person who has missed their appointment. According to the authors of this paper on non-attendance by diabetes patients, "People with diabetes who do not attend clinic appointments tend to have poorer glycaemic control, more complications, more frequent hospital admissions and increased all-cause mortality".
So why do patients miss appointments?
The study involved people with diabetes who had previously failed to attend clinic appointments. It found three main causes of missed appointments:
Practical barriers. These can include work and family commitments, and difficulties in travelling to appointments, particularly via public transport. Participants suggested that a wider range of appointment times and having fewer, longer appointments that addressed various aspects of their care would make it easier for them to attend.
Value of appointments. Participants mentioned aspects of appointments that put them off attending. Some were fearful of hearing bad news. Others felt reprimanded if they had not maintained "self-management" regimes. Others felt that they were not listened to.
Perceived impact of diabetes. The majority of participants felt that their diabetes had very little effect on their day to day lives. Some showed very little understanding of their condition, and one could not say which type of diabetes she had.
The authors suggest that their findings highlight the importance of psychological variables in predicting non-attendance at diabetes appointments. They state that "whilst interventions to improve attendance should address practical barriers...there may also be a need to take account of the underlying perceptions about diabetes, the emotional impact and perceived lack of value in attending appointments".
At a time when NHS strategies are focused more and more on "self-management" of long term conditions, these findings could have implications across a range of conditions and services.
Tuesday September 10th 2019
Patient Experience in England
Thousands of reports are published every year on patient experience in the NHS, by government bodies, patient voice organisations, health charities and academic institutions.
Our annual Patient Experience in England report cuts through the bewildering mountain of evidence, summarising a year's worth of patient experience surveys, and drawing out key themes from wider research.
The "state of patient experience" overview this year shows that:
- Some patients are more equal than others. The NHS offers universal health coverage but some groups do not get the access they need.
- Online patient feedback can build community - if healthcare professionals respond appropriately.
- Patient and public involvement in research is good in parts. There is not yet a consensus about the need for, and benefits of, involvement.
- Public funding for patient voice is declining, and drug companies are moving in to fill the gap.
The report also looks at "learning from deaths", and finds that culture is impeding progress. And it covers the deepening crisis in social care.
"Improving patient experience is a key aim for the NHS" says Professor Debra Jackson in her foreword to the report. "In my nursing career, I have seen how the unique patient perspective can reveal things that we can miss in the rush and busyness of providing care. The Patient Experience Library represents a realistic strategy to help health service staff gain insights into patient experiences and concerns."
Tuesday September 3rd 2019
Emergency admissions from care homes
It is well-known that one of the pressures on hospitals is delayed discharge - often linked to lack of capacity in care services. However, the care system can also cause pressure at the front end, by referring people into hospital unnecessarily. And A&E departments can take the brunt of this.
This Health Foundation briefing starts by observing that emergency admissions from care homes can expose residents to stress, loss of independence and risk of infection. It says that care home residents often prefer to be treated in the care home - so reducing emergency admissions could be good for residents, as well as help reduce pressure on the NHS.
The numbers are large - in 2016/17, over a quarter of a million care home residents in England attended A&E. But 41% of emergency admissions from care homes were for conditions that were potentially manageable outside a hospital setting, or that could have been caused by poor care or neglect.
The authors were surprised to find that emergency admissions were particularly high from residential care homes as against nursing care homes. Given that residential care homes provide 24- hour personal care, they say, one might expect residential care home residents to be less seriously ill than nursing home residents.
The study looked at four initiatives to improve health and care in care homes that were associated with the NHS’s New Care Models programme. It found reductions in at least some measures of emergency hospital use for residents who received enhanced support. This, it says, shows that there is potential to reduce demand for emergency care from care homes, but it also points to implementation challenges.
Co-production between health care professionals and care homes is key to tackling these challenges - but so is access to linked administrative datasets that can provide evidence to support policy making. It is important, say the authors, that these sorts of data are routinely and consistently collected and are easily accessible if we are to understand residents’ health care needs and improve care for this vulnerable group.
Wednesday August 28th 2019
Patient centred safety
The newly published NHS Patient Safety Strategy has been described by the NHS Confederation as a "paradigm shift" in the way the NHS treats patient safety. A key feature is a move away from a culture of blame to one of learning.
This paper from Ninewells hospital in Dundee shows what a safety learning culture looks like in practice. Better still, it explores - and resolves - a safety issue by using patient experience as a key learning tool.
The hospital's Radiology Department, in common with units across the UK, uses Magnetic Resonance Imaging (MRI) for diagnostic tests. MRI scanners are generally safe - but they generate magnetic forces that can be up to 30,000 times the strength of the Earth's magnetic field. These forces can cause overheating and malfunction in implants such as pacemakers and artificial valves.
Safety is addressed via a system which requires referrers (GPs, hospital doctors and others such as physiotherapists) to ask patients to list any implants or foreign bodies they have. A secondary check by radiography staff immediately prior to the scan provides a safety back-up. But, say the authors, "Despite constant efforts, there have been recurrent incidences of safety breaches with patients attending MRI department with implants, including pacemakers, when none have been declared".
Rather than ask referrers what was going wrong, the radiographers went to the patients. A questionnaire survey asked patients what safety checks they had undergone at the time of referral. It found that almost regardless of the type of referrer (GP etc) only 50-55% had been asked about pacemakers, and fewer than 50% had been asked about valves, clips and other metal objects in the body.
In case patients had misunderstood or forgotten their conversations with referrers, a second survey was carried out, using face to face interviews to check and clarify patients' responses. It found similar results.
Rather than blame the referrers for compromising patient safety, the radiographers developed a "strategy for change", with risk alerts, and reworking of questions on the referral form. In the twelve months following, there was no incident of any undeclared implant. This, say the authors, "was in sharp contrast to the continuous stream of significant events earlier that had prompted our intervention in the first instance".
The safety exercise was carried out at a Scottish hospital. But "pathways for MR referral and acceptance are broadly similar throughout the UK [therefore] this survey could be usefully applied to provide further insight to other NHS centres on MRI safety issues".
Tuesday August 20th 2019
Do what you say and say what you do
"Many people talk about the importance of public trust" says this report. But, it goes on, "Trust can only be earned, and that starts with understanding what people think, want and expect".
The report looks at trust and transparency in the politically fraught area of personal health and care data. It reveals a "healthy degree of scepticism among publics about whether the proclaimed benefits of better data use are actually realised in practice".
It also acknowledges "significant gaps in our understanding of people’s views, most notably around the perspectives of minority and marginalised groups". It notes that "Some groups may have good reason to feel distrustful of the health and social care system and be inherently concerned that data about them could be used to target or discriminate against them".
The report's focus is development of a Local Health and Care Record system in London. The aim is to make health and care information more consistent, more joined-up and more available to the clinicians, patients and families who need it. This might be complex to implement in practice, but "there should be no barrier to providing straightforward and comprehensive answers about why, by whom and how patient data is collected, managed, protected and used". And this should be informed by meaningful engagement with patients and public - "those with rights and interests over the data".
So how can transparency be achieved in the area of personal data, where there are legitimate concerns over matters such as anonymisation and information governance? The answer, it seems is that transparency can mean different things to different people but boils down to 'do what you say and say what you do'.
Debates over use of data are rarely easy. But "It is incumbent upon those managing and using data to describe a clear trajectory from the collection of data to delivery of benefits. Without this, the public will have every reason to question whether the case for using data beyond individual care really stacks up".
Tuesday August 13th 2019
Refusal and resistance
Dementia care is often thought of as taking place in the community, or in specialist settings and long-term care. However, as many as one in four acute hospital beds are occupied by a person with dementia, with some hospitals reporting that up to 50% of acute admissions may also have a diagnosis of dementia.
People with dementia are highly vulnerable within hospital settings, where functional abilities can deteriorate quickly. They are more likely to experience a delayed discharge, more likely to be readmitted and are at much higher risk of dying.
This study examined a common but poorly understood phenomenon within the acute setting: refusal and resistance to care. This can include getting out of bed, trying to leave the ward or hospital, shouting, and refusing food or medicine.
Reaction such as these were typically rational to the patient's perceptions. But ward staff typically interpreted resistance as a feature of a dementia diagnosis, which overshadowed the person. Chronic and disruptive resistance was viewed as a feature of the patient's identity, which could become their principal identity in the context of the ward.
The study found that refusals were "viewed by staff as problematic, difficult, signifying a lack of capacity, and, because they do not ‘fit’ the organisation and timetabled routines of the ward, as something that must be overcome or managed".
Staff responded with highly repetitive language, instructions to be obeyed, and containment of the person at the bedside. Raising the side rails of the bed or tucking bed sheets in tightly around the patient were common means of containing a patient within the bed. For patients sitting at the bedside, the close placement of the mobile tray table or unreachable walking frames and technologies such as chair alarms were used to contain people and keep them sitting in their bedside chair.
These approaches "created damaging cycles of stress for patients, families and ward staff". Furthermore, "approaches to... patient containment at the bedside were a response to resistance but also frequently the trigger for resistance or patient anxiety".
The study concludes that there are "powerful cultures of containment and restraint, with... work in the ward driven by the organisational demands of delivering care within fixed routines and timetables that do not meet the needs of people living with dementia". In response, the authors are developing "simple, no-cost innovations at the interactional and organisational level within wards that can be introduced and used by nurses and HCAs". The feasibility of these is currently being tested within one acute ‘laboratory’ ward.
Tuesday August 6th 2019
Navigating the feedback maze
It is no secret that NHS staff can feel swamped by the volume of patient feedback coming from Friends and Family Test, national surveys, local surveys, complaints, social media and more.
There is broad consensus on the value of seeking patients' views. But there is less agreement about how to learn from, and act on, the mass of data gained from widespread evidence-gathering.
According to this paper, "quantitative surveys [are] the most frequently collected type of patient experience data (often mandated) but the least acceptable to healthcare teams with respect to use within quality improvement". On the other hand, there is "an apparent sense of nervousness amongst hospital teams surrounding the use of qualitative data as it is regarded as time-consuming to collect and difficult to interpret without bias".
To try to make sense of all this, the researchers looked for a way to define types of patient feedback, and to develop categories that could help clarify potential uses for the different types.
A scoping review returned no fewer than 37 feedback types. These were sorted into 12 characteristics and then into 4 categories, as follows:
- Hospital-initiated quantitative surveys: eg the NHS Adult Inpatient Survey
- Patient-initiated qualitative feedback: eg complaints or twitter comments
- Hospital-initiated qualitative feedback: eg Experience Based Co-Design
- Other: eg Friends & Family Test.
These categories might help us to make sense of the wide range of patient feedback types in use across the NHS. But do they help us to make sense of the feedback itself? Unfortunately, the paper finds that few of the routinely collected feedback types elicit 'ready-to-use' data. And where useable data is easy to extract, it is "most suitable for measuring accountability, not for informing ward-based improvement".
The authors conclude that "If feedback is to be used more frequently within quality improvement, more attention must be paid to obtaining and making available the most appropriate types".
Wednesday July 31st 2019
Involving patients and public in research
Patients and the public get involved in research because they want to help others, and contribute to a better healthcare system. They may also have an interest in a research topic because of relevant personal experience.
These are good reasons to involve patients and public in research and according to this report, researchers often recognise and build on these motivations. However, that is not always the case. Sometimes, for example, patients and public are included in research simply because that is a condition of the research funding.
The report aims to build a better understanding of patient and public involvement (PPI) in research, to help ensure meaningful involvement. But that in itself is a major challenge, as "there is limited agreement about how, when, and why [PPI] should best be done".
Definitions are often blurred, and PPI "lacks standard terminology". Furthermore, "Few studies evaluated the fidelity of their PPI approaches, making it difficult to know whether the approaches discussed were implemented as intended". Under these circumstances, "PPI can sometimes become a tick-box exercise".
The report looks at the research tasks and activities that patients and public can undertake, and considers enablers and challenges to involvement. It also explores questions of impact and evaluation.
The authors point out that "Some have assumed the more PPI, the better, suggesting that co-production - the most involved of PPI approaches - is the 'gold standard'. Others reject the idea of 'the more, the better', raising concerns that it may lead to tokenistic practice or work against meaningful involvement".
They conclude that "with careful consideration of when to do PPI... all sides can benefit from bringing real-world understandings into research about healthcare".
Tuesday July 23rd 2019
Putting out fires
Patient experience staff may be familiar with the idea that some types of patient complaint are perennial, pervasive and well-known.
One example is "communication" or "attitude" - a sense from patients that even if their clinical care was good, the way they were spoken to could have been better. Another is waiting times, along with difficulty getting appointments, or scheduled appointments being rearranged at short notice.
According to one nursing unit manager interviewed for this Canadian study on patient complaints, "nothing is new, but we don’t have a solution".
So why is it that some types of patient complaint persist for years, without appearing to lead to institutional or system-wide improvements? The authors identify three challenges:
Firstly, the nature of the issues are well known, but difficult to address. Some clinicians, for example, simply apologise when a complaint arises about their attitude, rather than working on improving their communication style. And although training courses on communication may be well received by staff, they do not necessarily stop communication coming up as an issue in complaints year after year.
A second challenge is the use of weak change strategies. Again, there may be an over-reliance on one-off education sessions. Or improvements may be restricted to specific units, rather than rolled out across whole institutions or systems.
The third challenge is resolution of complaints outside the formal complaints structure. The study found that unit managers preferred handling patient complaints directly, as formal complaints might suggest failures in their management. Moreover, they considered the additional bureaucracy of a formal complaint burdensome, and many complaints lodged through the formal system would eventually come back to unit managers for resolution anyway. But when complaints are resolved directly, the learning - about both the problem and the solution - may be invisible to the institution as a whole.
Faced with these challenges in embedding organisational learning and improvement, patient experience staff focus instead on "complaint resolution", typically defined as addressing patient complaints in as timely a fashion as possible. Many referred to this part of the job as "putting out fires".
The authors found that "in an effort to do something rather than nothing, [patient experience staff] reach for simple and inexpensive responses". But "the daily work of 'putting out fires' and ... simply placating patients and resolving complaints as quickly as possible... may in effect suppress the patient voice".
The authors conclude that "the major categories of complaints remained unchanged year after year [which] in itself attests to difficulties in developing effective improvements from past complaints".
Tuesday July 16th 2019
Neuro patience
We are all used to the big national patient experience surveys carried out by the Care Quality Commission and NHS England. These cover patient experience of maternity services, community mental health services, GPs and so on. Results are published by provider and the surveys are, essentially, a test of people's access to, and satisfaction with, services.
But there is another dimension to patient experience which is less well explored. That is people's experience of living with long term health conditions. And this really matters, given the increasing emphasis on "self-management" within NHS strategies.
So it is encouraging to see the Neurological Alliance continuing to show a lead in how patients can help to build an evidence base, and a case for change. Their latest patient experience survey highlights key areas for improvement, based on the following:
- Long delays, and a lack of access to specialists. Around a third of survey respondents waited more than 12 months to see a neurologist.
- A lack of personalised care. Only 42% of neurology patients had written information at the time of diagnosis, against 83% of people with cancer. Just 10% had been offered a care plan.
- Poor experience of social care, with many people dependent on unpaid carers.
- Disability discrimination in the workplace, and problems accessing welfare benefits.
This year for the first time the results are broken down to regional level, based on the Sustainability and Transformation Partnership (STP) footprints. The findings reveal wide geographic variation, representing a postcode lottery in access to care. And it may come as no surprise to learn that people in the most deprived areas report the poorest experiences of care.
National patient surveys run by the CQC and NHS England are valuable - helping patients and providers alike to get a sense of people's experiences within individual services. But in an NHS that is building integrated care systems, we need to understand how people experience care across services, and through pathways, and how they cope with extensive periods of self-management of their conditions.
The Neurological Alliance is uncovering evidence that can provide an important counterpoint to the mainstream national surveys. Their work deserves to be taken seriously.
Tuesday July 9th 2019
Large scale change
With the advent of Sustainability and Transformation Partnerships, Integrated Care Systems and the NHS Long Term Plan, we are getting used to the idea of large scale change in healthcare. However as this paper points out, large scale change tends to be associated by the public with making cuts and downgrading services, and can be met by strong opposition.
The response is public involvement - to increase the legitimacy of decision-making, tailor publicly-funded services to local needs and resolve tensions. But what actually is public involvement?
A plethora of terms are used to refer to who should be involved: patients, service users, citizens, public, lay people, communities or consumers. And the term involvement is often used interchangeably with participation, consultation or engagement. Little is known about how involvement is understood, or operationalised in practice. It remains unclear which methods are most appropriate under different circumstances, and evidence about the impact of involvement is sparse.
This study found that in large scale change, public involvement often takes the form of a consultation model in which information flows one-way. Any public opposition is attributed to a lack of understanding of the technical arguments, implying a need to improve communication rather than offer more deliberative methods of involvement.
But sometimes the public both understand and question the technical arguments, seeking alternative routes to voice their views. As a result, two models of involvement co-exist: invited and uninvited participation.
Uninvited (oppositional) participation is often framed as an obstacle to implementation of large scale change. But, say the authors of this paper, "Political conflict is an inherent, and potentially beneficial, part of healthcare planning. Thought should be given to reframing the conflict in large scale change as positive, and how it can be incorporated into meaningful methods of public involvement".
Tuesday July 2nd 2019
Lost in the system
'As a former cancer patient I fear getting sick again, but it’s not the disease I fear, it’s being lost in the system that scares me.'
These words are from Rachael Bull, a contributor to the latest edition of Patient Experience magazine. We think they should be heard by healthcare providers everywhere. Imagine being more afraid of the healthcare system than you are of cancer.
Patient experience is often thought of in terms of things like compassion and 'patient-centred' care. These things matter, but both patients - and the staff looking after them - are let down when appointments are cancelled, records go astray and 'pathways' that look good on paper turn out to be impossible to navigate in practice.
Another contributor - Cancer Mum - has a similar story. As a long term carer for her disabled son, she had to fight for access to his records. But she then found herself with a record containing hundreds of document and consultation entries that had not been indexed and so were useless.
These are powerful illustrations of why we need to see things from the patient’s point of view. For healthcare professionals, an overly complex system can be exasperating. For patients, it can be life-threatening.
So it is good to see the NHS Leadership Academy taking matters such as these seriously. Our third contributor, Karl Roberts, talks about the importance of developing patient leaders with the skills and confidence to take their experiences into senior levels of healthcare organisations.
Healthcare systems need to hear from people like Rachael and Cancer Mum. But they also need to embed individual stories in a solid base of evidence. So the magazine includes our usual round-up of the latest research on patient experience and involvement, with summaries to help you get quickly to the information you need.
Tuesday June 25th 2019
Inpatients speak out
The Care Quality Commission's Adult Inpatient Survey has now been running for 15 years, but as the CQC says, "every year brings a new perspective". So what do this year's results show?
As always, there is good news. Trust in doctors and nurses remains relatively high, most patients (over 90%) report that they had enough privacy, and communication between patients and staff remains a positive experience for most. Patient satisfaction with hospital food has improved over the years, with the proportion of those saying that it was 'very good' increasing from 19% in 2009 to 23% in 2018.
Alongside this, however, are areas that consistently show poor patient experience, including waiting times, the quality of information and involvement around hospital discharge, and experience of integrated care.
Patients' reports of problems with waiting times have been corroborated by the House of Commons Public Accounts Committee, which has deemed it "unacceptable that less than half of NHS trusts meet the waiting times standard for elective treatment, and only 38% meet the standard for cancer patients". The committee is concerned that national bodies "appear to lack curiosity regarding the impact of longer waiting times on patient outcomes and on patient harm".
Hospital discharge is a longstanding source of dissatisfaction for patients, with Healthwatch reporting back in 2015 (and many times since) on the problems.
The survey also finds that "people’s experience of the integration of their care has got worse". 18% of respondents said they did not know what would happen next with their care when they left the hospital, and nearly a quarter of patients (24%) said they did not get enough support from health or social care professionals to manage their conditions after leaving hospital
The CQC concludes that "While last year we reported on a system still delivering improvements in patients’ experiences despite growing pressure, this year, the improvement is not sustained. In 2018, there is a lot of evidence to suggest that pressure on the system is having a real impact on patients’ experiences of care".
Tuesday June 18th 2019
Care deserts
This report, commissioned by Age UK, looks at the geographical lottery for residential and domiciliary care. It argues that some parts of the country are turning into ‘care deserts’ - areas where even if you have money to spend on care, you will be unable to get it.
The report makes the point that "With still no sign of the Government’s green paper, the social care system has been left waiting for over two years for the Government to set out its vision for the long-term sustainability of the system". It observes that "There have been four independent reviews, five consultations and seven government policy papers focused on social care in the last 20 years without a meaningful change to the system".
The result, it says, is a social care workforce crisis, and a reduction in the number of both care home and nursing home beds, at a time of rising need. It describes a dysfunctional market for social care, and states that "The needs of some older people must be going unmet, or they face travelling a long way to get into a care home, or their families and friends have to care for them instead. In [some] areas the care market has ceased to function and there is no care to be had".
The report refers to the Care Quality Commission's 2015/16 State of Care report which raised concerns that social care was reaching a ‘tipping point’. It goes on to state that "in some places that tipping point has now been passed".
The report pulls no punches about the lack of an effective political response. It states that "while ‘Brexit sucks all the political oxygen out of the air’... social care is gradually rotting away".
Tuesday June 11th 2019
Body image matters
This report opens with the observation that "for too many of us, our bodies are sources of shame and distress".
It backs this up with statistics: for example that during the last year, one in five adults felt shame, just over one third felt down or low, and 19% felt disgusted because of their body image.
This matters because higher body dissatisfaction is associated with a poorer quality of life, psychological distress and the risk of unhealthy eating behaviours and eating disorders.
Body image concerns have been found to be more prevalent among people who are overweight or obese. But there are further issues relevant to body image and mental health that are specific to certain factors and experiences. These include pregnancy, the effects of long term health conditions, menopause, and ageing. Cultural differences around body ideals, and gender and sexuality also play a part.
The report is clear that developing healthy attitudes towards body image is not simply a matter for each of us individually. It considers how attitudes are shaped by advertising and social media, and how better industry regulation, combined with stronger public health initiatives, can make life better for everyone.
Tuesday June 4th 2019
Raising the equality flag
This study takes as its starting point the fact that most LGBT people aged over 50 were born when being gay was effectively illegal in the UK. Some may have hidden their LGBT identity - and from a health perspective, this could have led them to hide aspects of their own health for fear of 'outing' themselves. For others, it could have fostered a reluctance to engage with health services for fear of discriminatory attitudes by health care providers.
The study looked at the health and care needs of older LGBT people across four categories: physical health and access to health care; access to social care and end-of-life care; experiences around loneliness, social isolation, and mental health; and experiences of violence.
It found that LGBT men and women aged 50+ have poorer self-rated health and are more likely to have other conditions that impact their health and wellbeing. This matters because poor self-rated health is a strong predictor of future mortality and is also used to determine healthy life expectancy and disability-free life expectancy.
There are implications for policy and practice: bodies like Public Health England are required to work toward reducing health inequalities, while local authorities have a duty to advance equality established in the Equality Act 2010. In spite of this, responses are patchy. For example, an information standard for monitoring sexual orientation is now available to all NHS organisations but use of the standard is not compulsory.
The report makes the point that specialist or targeted services rarely exist outside certain cities in which there are higher concentrations of LGBT people. But it goes on to say that while there is value in targeted/specialist services in certain areas of the country, greater effort must be made to improve the inclusivity of mainstream service provision.
Wednesday May 29th 2019
Screening patients out?
Health screening hit the headlines a year ago, when Secretary of State Jeremy Hunt announced that there had been a serious failure in the English breast screening programme.
Subsequent investigation found that the error was more administrative than clinical. A new service specification did not align with the IT system then in use, and was not consistently implemented by breast screening units. No-one in the Department of Health and Social Care, Public Health England or NHS England had realised.
One year on, the House of Commons Public Accounts Committee has taken another look at health screening.
Its report says that screening is an important way of identifying potentially life-threatening illnesses at an early stage. Yet the Department of Health & Social Care, NHS England and Public Health England are not doing enough to make sure that everyone who is eligible to take part in screening is doing so, and do not know if everyone who should be invited for screening has been.
The committee took evidence on the management of four health screening programmes operating in England: bowel, breast and cervical cancers and abdominal aortic aneurism. None met their targets for ensuring the eligible population was screened in 2017-18.
Performance varies drastically across the country and yet the national health bodies still do not know which specific barriers prevent certain groups from attending meaning they cannot effectively target these groups to encourage them to attend.
National health bodies therefore run a constant risk of not knowing if all the people who should have been identified for screening have been. At the centre of this, the national oversight of screening programmes has failed patients, resulting in thousands of women not being invited for breast and cervical screenings or waiting too long for their cervical screening results.
The committee concludes that national health bodies have been too slow to recognise and respond to the problems caused, including sufficiently holding local screening providers to account for long-term failure.
Tuesday May 21st 2019
Cwm Taf women's voices
The official review of maternity services run by the Cwm Taf Health Board has now been published. It was triggered by the identification of 43 potential Serious Untoward Incidents that included stillbirths, neonatal deaths and complications of pregnancy or delivery.
Our featured report this week is a record of the public engagement exercise that ran alongside the official review. The aim was to assess whether services were woman-centred, open and transparent.
The authors found that "overwhelmingly, the women and families who came forward... spoke about distressing experiences and poor care". The result was "both physical and psychological impacts on them and their families"..
In a dismaying echo of the Morecambe Bay investigation, "Women repeatedly stated they were not listened to and their concerns were not taken seriously or valued". In the worst cases, "they were ignored or patronised, and no action was taken, with tragic outcomes including stillbirth and neonatal death of their babies".
Women's sense of not being heard was compounded by other factors including:
- Lack of access to all appropriate information, including notes
- Lack of comprehensive investigation resulting in incomplete responses to concerns
- Focus on providing responses that were formulaic and seemed to be more interested in defending the reputation of individuals and the Health Board
- Failure to apologise, causing distress
We have heard all this before - not just at Morecambe Bay, but at Mid Staffs, Southern Health, Gosport and in the Northern Ireland Hyponatraemia inquiry.
The report states that "Already, work is being undertaken to use the lessons from the poor experience of those families... to change culture and behaviour". That news is welcome - but it is not enough. Bill Kirkup, author of the Morecambe Bay report said, "It is vital that the lessons, now plain to see, are learnt and acted upon, not least by other Trusts, which must not believe that ‘it could not happen here’." So we hope that all providers of maternity services - even those that think they are doing a good job - will take the Cwm Taf review as a signal to revisit their own practice in hearing and acting on feedback from patients.
Tuesday May 14th 2019
Staff vs culture
Just over a year ago, we carried "Ignoring the Alarms" as the featured report in our weekly newsletter.
The report, from the Parliamentary and Health Service Ombudsman, told of "multiple serious departures from the standards of care expected" which had led to the avoidable death of Averil Hart, a young woman who had anorexia nervosa.
Today, a House of Commons inquiry looks further into those failings, taking in not just the clinical care of the patient, but also the treatment of bereaved relatives who subsequently tried to find out what had gone wrong.
We have submitted evidence to that inquiry, setting the PHSO's findings alongside similar findings from academic research, regulatory bodies, and other official inquiries. Our submission might make for uncomfortable reading.
We all know that there are staff right across the NHS who want the best for patients, and understand that "patient experience", in its broadest sense, is every bit as important as clinical care. But they are being let down - by Boards who won't take patient experience seriously enough, by clinicians who cannot see patient complaints as grounds for quality improvement, and by organisational cultures which inhibit change.
The Chief Inspector of Hospitals has recently commented on progress in learning from deaths. He said that "...the same issues persist... issues such as fear of engaging with bereaved families". And he warned that "the current pace of change is not fast enough".
With the publication of the Cwm Taf report, and with the Shrewsbury and Telford review coming soon, we need absolute honesty about shortcomings in the way that patients and relatives are treated when things go wrong. Otherwise, as Bill Kirkup said in the investigation into the Morecambe Bay scandal, "we are destined sooner or later to add again to the roll of names".
Wednesday May 8th 2019
Questionnaires versus online feedback
Patient feedback is integral to safety and quality of care. And an NHS that aims to be person-centred needs to understand patient experience really well.
Attempts to understand patient experience often involve structured questionnaires. But in a digital age, more and more people are bypassing formal surveys, and giving feedback online.
This study looks at the requirement to include patient views in regulatory processes such as medical revalidation. It asks whether questionnaires are tackling the right questions in the right way, and whether they align with the kinds of issues that patients address in online feedback. The study focused specifically on patient experience of psychiatric care.
A key finding is that patients describe some different measures of psychiatric care quality online and use different terminology to those used in questionnaires. This may reflect the acknowledged exclusion of patients and the public in the design, administration and evaluation of patient feedback questionnaires, accentuating the importance of coproduction.
Another finding is that when psychiatric patients discuss their care online, they rarely focus on the care provided by a single psychiatrist alone. Other healthcare individuals, services, systems or processes are also described. The authors suggest that the current GMC revalidation requirement for patients to disaggregate the care provided by an individual practitioner from the wider healthcare team, service or environment is therefore unhelpful.
Timeliness matters too. Working online, patients can offer feedback as and when they need to. But, say the authors, "The current requirement to collect patient feedback so infrequently (once every five years) sends the message, whether intentional or not, that patient feedback is unimportant".
The study concludes that "The sharing of healthcare experiences online could help create desirable and dynamic transparency to the benefit of both current and future patients".
Tuesday April 30th 2019
A hostile environment for care
"There is now clear evidence that The National Health Service (Charges to Overseas Visitors) (Amendment) Regulations 2017 are deterring vulnerable groups from accessing NHS treatment, threatening public health, and taking vital clinical time away from patient care."
This opener to a new report from the BMA sets the scene for a strong challenge to government on its rules for charging 'overseas visitors' for accessing NHS services in England.
The rules, introduced in 2015, are seen as part of the government's "hostile environment" for immigration. They were updated in 2017, to expand charging to community services, introduce upfront charging for non-urgent care, and require NHS services to record patients' eligibility for free treatment.
The Department for Health and Social Care (DHSC) announced a review in December 2017, less than two months after the updated rules came into force, and before some providers had had time to fully implement them, let alone assess their impact. DHSC says that the review found no evidence of the regulations deterring patients from accessing care - but it has said that the findings of the review will not be published.
The BMA's report is based on a survey of its members, and refers to patient experience as outlined in reports such as Maternity Action's What Price Safe Motherhood. It finds that patients are, in fact, deterred from seeking care, "including for treatments that are not chargeable". It states that "vulnerable groups are being, and will continue to be, negatively affected by the regulations".
The BMA is calling for publication of the findings of the DHSC review, and for "the introduction of safeguards to ensure that vulnerable populations are not deterred from seeking care, are able to access the care they are entitled to and that necessary treatment is not denied due to difficulty or delay in proving eligibility".
Wednesday April 24th 2019
Pulling in different directions
For some years now, there has been talk of "parity of esteem" between physical and mental health. This has been defined as "valuing mental health equally with physical health" and has been seen as a way to raise standards of care for people with mental health conditions.
But how do we assess "value" in mental health services and treatments? What outcomes should we be looking for, and how would we measure them? This paper from the King's Fund makes the point that "Even the briefest discussion with service users shatters the illusion that agreeing these outcomes will be an innocuous administrative exercise".
It goes on to say that, "While there are many strong partnerships between service users and NHS services, there was also evidence of profound differences in perspective on what is important and even, at times, outright hostility and distrust between the two sides".
Some service users are suspicious of "narrow clinical" responses to illness, and "oppressive interventions" such as restraint and seclusion. NHS staff, for their part can feel "accumulated demoralisation when they see the same patients in their clinics, caught up in the same cycles, struggling to make progress".
This leads to a risk that "people with mental health problems are among the 'problem patients' of modern health care - those that seem to rub the system up the wrong way and wear professionals down with their stubborn refusal to be cured".
In this context, the task of defining "value" in mental health services, along with desired outcomes, is very difficult. "The outcomes prioritised, and those discounted, inevitably reveal the degree of influence of different voices in the discussion - those around the table and those outside the room."
The report reflects on the advantages and disadvantages of current approaches, and makes some suggestions for the future. It concludes that "we cannot usefully direct mental health services to the dogged pursuit of particular outcomes until there is a broader consensus on which outcomes really matter".
And with "service users, professionals and different professions... pulling in different directions... it is also clear that some sort of reconciliation is urgently needed".
Tuesday April 16th 2019
Must we bust the trust?
"Although patients desire safe care, they are reluctant to perform safety-related behaviors when they worry it could harm the relationships they have with clinicians."
The opening statement from this week's paper lays bare the reality of safe practice in healthcare settings. Safety is not simply a matter of well-trained staff following the right procedures. It is also culturally influenced, depending on the quality of relationships between clinicians and patients.
This American study finds that interventions tend to focus on giving patients access to information about their own care, but generally do not attempt to influence the clinician-patient relationship. Yet, the clinician-patient relationship influences patients' willingness to engage with their safety.
In particular, patients are reluctant to engage in safety behaviour that requires them to digress from the traditional patient role by questioning or challenging clinicians' judgments. Perceptions of staff time pressure, fear of negative reactions from clinicians, and the fear of being seen as a "difficult" patient have been found to inhibit patient engagement in safety.
Sometimes, in an apparent reversal of the doctor-patient relationship, it is patients' concerns for the wellbeing of clinicians that drives behaviour. Some patients "exhibited a desire to protect their clinician' emotional or professional needs that at times interfered with their desire to engage with their own safety". Others "were reluctant to report undesirable events because of their concern over repercussions to hospital staff".
The authors suggest reframing safety behaviour as a co-operative act. One example is to provide a shared safety checklist with tasks assigned to both clinicians and patients. Transparently assigning tasks to both parties could help cultivate a sense of teamwork between patients and clinicians, especially if patient participation is framed as helping clinicians and contributing to the team, rather than simply ensuring personal safety.
The paper finishes with a warning about the development of new technology. Because the importance of the clinician-patient relationship to safety, technologies should be used to supplement face-to-face communication, rather than completely replacing that communication.
Tuesday April 9th 2019
Stop measuring, start learning
Why is there a seemingly endless debate about the "impact" of patient and public involvement (PPI)? It's as though we can't accept that dialogue between patients and professionals is intrinsically a good thing. We have to justify it through complicated and time-consuming "impact measurement".
The authors of this paper argue that PPI professionals are unduly influenced by clinical practice, which uses interventions to treat medical conditions in ways that can be objectively evaluated. But is it sensible to conceptualise involvement as a "measurable intervention"?
The paper suggests an alternative approach that sees involvement as "conversations that support two-way learning". Instead of a "correct method" for involvement, it advocates varying approaches, tailored to the context and the needs of the individuals involved. Crucially, the quality of the interaction between professionals and public becomes more important than the process.
Still - the question remains: how do we know whether involvement actually makes a difference? According to the authors, obtaining "robust evidence" of the outcomes of involvement may not be possible or appropriate. For them, researchers' subjective accounts of what they learnt through involvement represent an equally valid way of knowing whether involvement has made a difference.
The paper argues for different approaches to evaluating and reporting involvement. These could share researchers' personal accounts to describe what was said and learnt by whom (short term outcomes), what changes were made as a result (medium term outcomes), and the long-term, wider impacts on the research culture and agenda.
Tuesday April 2nd 2019
The power of two truths
What happens when two or more versions of truth, otherwise in conflict, come together to create a new version of the truth?
That is the question posed by Jessie Cunnett in the latest edition of Patient Experience Quarterly. She makes the point that when it comes to issues of patient safety or fitness to practise, different stakeholders have different ways of understanding what matters. Clinicians start from a medical perspective. Lawyers want to determine right and wrong. Patients and their relatives work from subjective experience.
As Cunnett sees it, professional regulation in its current legalistic form is not keen on subjective accounts. It wants to identify statements of fact so that all doubt is removed. But for her, the facts must be judged in context. And the patient experience is an essential part of understanding evidence roundly and in a meaningful way.
Our other contributors pick up the idea of differing - sometimes conflicting - truths. Mark Hudson nearly died - and that changed his life for the better. He has dyslexia - and gets his ideas across through his writing. His dream of being a doctor was shattered - but he is able to help people recovering from the experience of intensive care.
Liza Morton nearly died as a baby, and then became, in her own words, a "medical curiosity". She owes her life to science, but wonders whether there is more room for recognising the emotional toll of treatment - for both patients and clinicians.
Mark's and Liza's stories show that in healthcare, objective science and subjective experience are closely intertwined.
There are yet more truths to be found in our round-up of the latest studies and surveys on patient experience. Our mission (in a "post-truth" world) is to put patient experience work on the same evidence-based footing as clinical work. So it is heartening to see excellent evidence being produced by academics, charities and government bodies. We continue to collate, catalogue and preserve as much of it as we can.
Tuesday March 26th 2019
Changing the culture of care
Several of our previous newsletters have touched on the subject of learning from deaths. That's because there can be no worse experience in healthcare than the avoidable death of a loved one. The experience is even worse when bereaved relatives feel locked out of investigations, and have to fight - sometimes for years - to get the truth.
The current investigation at the Shrewsbury and Telford Hospital NHS Trust is just the latest in a series of such cases, taking in Mid Staffs, Morecambe Bay, Southern Health, Gosport and the Northern Ireland Hyponatraemia inquiry.
Against this background, the National Quality Board has issued guidance on learning from deaths. This report from the Care Quality Commission looks at how - and whether - NHS Trusts have been implementing the guidance.
It paints a mixed picture. Right at the start of the report, the Chief Inspector of Hospitals says, "... we are concerned that we are still seeing the same issues persist in some NHS trusts more than two years on. Issues such as fear of engaging with bereaved families, lack of staff training, and concerns about repercussions on professional careers, suggest that problems with the culture of organisations may be holding people back from making the progress needed".
Happily, some Trusts have been more active in adopting the guidance, and the report gives examples, along with detailed case studies illustrating both challenges and practical solutions. These make it clear that "there is no one factor that guarantees good practice, with enablers and barriers to implementing the guidance being interrelated. However... the existing culture of an organisation can be a key factor in trusts'implementation of guidance".
That question of organisational culture is important, as it clearly influenced developments at Mid Staffs and elsewhere. And on this point, the Chief Inspector sounds a warning note: "Cultural change is not easy and will take time. However, the current pace of change is not fast enough".
Tuesday March 12th 2019
Public satisfaction on the slide
"In 2018, the outpouring of affection that accompanied the NHS's 70th birthday did not stem falling levels of public satisfaction with the service."
So say the King's Fund and Nuffield Trust in their annual overview of public satisfaction with the NHS and social care.
The report highlights various points of detail - for example that older people were more satisfied than younger people, and that supporters of the Conservative party were more satisfied than supporters of the Labour party. And within the overall picture, there is good news - for example, that satisfaction with inpatient services is at its highest level since 1993, and satisfaction with outpatient services is at its highest level since the survey began.
However, the authors point out that the data gives its richest insights when viewed over decades rather than years. So the 2000s were characterised by increasing satisfaction, while the 2010s are characterised by decreasing satisfaction. And although levels have fluctuated, the broad trend shows a falling level of satisfaction, which in 2018 was 16 percentage points lower than in 2010.
The four main reasons for satisfaction were the quality of care; treatment free at the point of use; the range of services available; and the attitudes and behaviour of NHS staff. Conversely, dissatisfaction arose from long waiting times; staff shortages; a lack of funding; and money being wasted.
The report concludes that with less firm commitments to reducing waiting times than in the past, and the government's strategy for dealing with critical workforce issues still outstanding, we must wait to see when the decade-long slide in public satisfaction with the NHS will come to an end.
Tuesday March 5th 2019
Patient involvement in animal research
This report opens by stating that "Patient and Public Involvement and Engagement (PPIE) is increasingly embedded within healthcare research".
It notes that "lay people" can become involved at various points within research processes. And increasing openness within the research community means that patient and public involvement is ever more extensive. So perhaps we need to start raising questions about PPIE and animal research.
The study found that patients and public can see value in opening up conversations about animal research. It can help to alleviate anxieties by providing opportunities to learn more about how animals are used. But for some people, being involved in research that uses animals is an ethical and emotional challenge.
Funders often believe patients and public should be involved with all types of research, including animal research. However, there is also apprehension about how to organise PPIE around animal research, how to manage potential concerns, and whether it can make a meaningful difference to research.
For researchers using animals, PPIE can be an opportunity to engage people's lived experience and help ensure research will be meaningful and beneficial. However, these conversations can be uncomfortable and there are challenges around how best to communicate and listen.
The authors see public involvement with animal research as an emerging area, informed by changing research cultures of communication and openness. And as PPIE practices are increasingly embedded in research funding and strategy, public involvement with animal research is likely to become more common.
This may not be easy - many people could find it challenging having conversations about animal research. But, say the authors, there are also potential problems from not having these conversations for research transparency, authentic engagement, and research translation.
Tuesday February 26th 2019
Reducing readmissions
Towards the end of 2017, Healthwatch England published a briefing on emergency readmissions to hospital. It noted that numbers had been rising for some years, and said that in 2016/17, over half a million emergency readmissions had been reported across 84 hospital Trusts.
Worryingly, only four of the 125 Trusts contacted were able to provide information outlining the reasons for emergency readmission. Many Trusts explained that the information was not kept electronically, or was stored on paper records, making it too difficult to analyse.
Our featured report this week sheds some light on the matter - and interestingly, its starting point is not medical records kept by healthcare providers, but the perceptions of patients who have experienced hospital readmission. Furthermore, it did not concern itself with in-hospital discharge procedures, but looked instead at the challenges patients face after leaving hospital, including social determinants of health (SDoH) such as safe housing, food access and economic stability.
The study found that high proportions of patients cited non-medical factors as reasons for readmission. There was an increased risk of preventable readmissions associated with a history of homelessness, substance use disorder, or at least two unmet SDoH health related needs. Indeed, patients with at least two unmet SDoH needs were almost three times more likely to have a preventable readmission rather than a non-preventable readmission.
The authors state that their data underline important vulnerabilities and reflect the growing complexity and evolving scope of current medical practice.
The study was conducted in America so may not, on the face of it, be directly applicable to the UK. However, the NHS Long Term Plan sets a clear steer towards personalised care and integrated services. That means understanding people's personal circumstances, and co-ordinating a range of services around the individual. In this context, closer joint working between health services, social services and voluntary organisations could be a way to ensure successful hospital discharge and fewer readmissions.
Tuesday February 19th 2019
Sweet dreams are made of this
"Disruption to sleep is known to interrupt recovery and increase the chances of poor health and wellbeing." So says the Care Quality Commission in its most recent Adult Inpatient Survey. In spite of this, the survey findings show that 1 in 5 patients were bothered by noise at night from hospital staff.
Our featured report this week is an American study which starts from a similar premise: "Although sleep is critical to patient recovery in the hospital, hospitalization is not restful, and inpatient sleep deprivation has been linked to poor health outcomes".
The study tested the effectiveness of the SIESTA intervention - based on patient and staff feedback, from which "overnight vitals, medications, and phlebotomy were identified as major barriers to patient sleep".
One important finding was that some sleep disruption was due to basic system errors as opposed to uncaring staff. For example, the electronic health record contained various default settings, but physicians did not know how to change the default vital signs order 'every 4 hours'. They were also unaware of how to batch-order morning phlebotomy at a time other than 4:00 am.
The SIESTA system was introduced to two general medicine units, but in one it was enhanced with nursing education and empowerment. This included giving nurses pocket cards describing the mnemonic SIESTA (Screen patients for sleep disorders, Instruct patients on sleep hygiene, Eliminate disruptions, Shut doors, Treat pain, and Alarm and noise control). Nurses were also coached to collaborate with physicians to implement sleep-friendly orders.
In both units, the intervention was associated with a significant reduction in orders for overnight vital signs and medication administration. However, addition of nursing education and empowerment in the SIESTA-enhanced unit was associated with fewer nocturnal room entries and improvements in patient-reported outcomes compared with those in the standard unit.
The authors conclude that "even when sleep-friendly orders are present, creating a sleep-friendly environment likely depends on the unit-based nurses championing the cause".
Tuesday February 12th 2019
The community value of community hospitals
In some parts of England, Sustainability and Transformation Plans have led to battles over the future of community hospitals. To health service managers, the institutions can sometimes appear outdated, poorly located and possibly no longer fit for purpose. To local communities, they can represent cherished assets, where generations have been cared for, and for which "Friends of" groups have tirelessly fundraised.
For this study, the starting point was that there is no agreed definition of what a community hospital is. Furthermore, little is known about patients' experiences of them or how they are supported and valued by local people.
The study found that patients and carers experience community hospitals as qualitatively different from other settings. Key to patients' and carers' experiences of community hospitals was their closeness to "home" through their physical location, environment and atmosphere. Relationships also counted - particularly community hospitals' provision of personalised, holistic care; and their role in supporting patients through difficult psychological transitions.
A further finding was that community hospitals are highly valued by their local communities. People support their hospitals through giving time, raising money, providing services and giving voice. This can contribute to hospital utilisation and sustainability, patient experience, staff morale and volunteer well-being.
The study concludes that community hospitals enable the provision of local intermediate care services, delivered through an embedded, relational model of care, and generating deep feelings of reassurance. However, it says that current developments (including the withdrawal of GPs, shifts towards step-down care for non-local patients and changing configurations of services, providers and ownership) have the potential to undermine these positive experiences and values.
Tuesday February 5th 2019
The language and culture of complaints
It has been good to see NHS Improvement inviting comments on proposals for a patient safety strategy. Importantly, the proposals make repeated reference to a "just safety culture". This matters, because a key learning point from Mid Staffs, Morecambe Bay, Gosport and elsewhere is that regulation and procedure alone cannot protect patients from unsafe cultures.
So where do unsafe cultures come from? Sometimes they can arise from the visible effects of poor leadership, bullying of staff, or workforce pressures.
But some influences on culture are less visible. When culture is just "the way we do things around here", staff can become oblivious to the ways in which their behaviour and attitudes can affect patient safety.
One example is the language that is commonly used to describe patient feedback. We can start with the language of "complaints".
When a health professional flags up something that has gone wrong, it is called an incident report. But when a patient does the same, it is called a complaint. The word "complaint" is synonymous with words like "objection", "grievance" and "criticism". Culturally, it creates a tone of negativity.
So it is perhaps unsurprising - as we have already reported - that some health professionals see complaints as "a breach in fundamental relationships involving patients' trust or patients' recognition of their work efforts". Within a culture like this, it can be "rare for [professionals] to describe complaints raised by patients as grounds for improving the quality of care".
A similar language problem affects wider patient feedback (patient surveys, focus groups, social media posts) - frequently described as "anecdotal evidence". The term indicates a cultural tendency to see patient feedback as subjective, irrational, and potentially unreliable.
A "just safety culture", as called for in the draft patient safety strategy, would make it clear to patients that their feedback was valued and would be acted on. It would treat patient stories as valid evidence, having equal weight with clinicians' stories, set down in their written notes.
Healthcare providers could start down this path by changing their language. They could start describing patient complaints as a form of incident reporting, complementary to that practised by staff. And they could recognise that reference to patient feedback as "anecdotal evidence" is indicative of a dismissive and disrespectful safety culture, and should not be tolerated.
You can read our BMJ opinion piece on this topic here.
Tuesday January 29th 2019
Rare disease and mental health
We recently touched on the experiences of parents who have children with rare diseases. The study, from Canada, described a complicated experience, with numerous doctors' appointments, and the need for persistence in pursuit of a definitive diagnosis. It found contentious relationships with healthcare providers, and a lack of formal care co-ordination and communication between services.
This UK study touches on similar issues, and explores the effect on the mental health of adult patients living with rare disease, and their carers.
The report is based on a survey which found over 90% of respondents feeling low, stressed or worried about their condition. 88% have felt emotionally exhausted, and 70% have felt at breaking point.
Over 80% of respondents put feelings of this kind down to health professionals having a poor awareness of their condition, along with a sense of not being believed. Mislabelling and misdiagnosis can delay the start of appropriate management and treatment, and can also prevent people from seeking help.
In spite of this, around half of patients and carers affected by rare disease are never asked about their mental health.
Healthcare professionals might be tempted to think that rare disease is a niche topic. And it is true that a single rare disease may affect a relatively small number of people. But there are over 6,000 known rare diseases, so a much larger number are affected overall.
The report is clear that awareness among healthcare professionals needs to improve. Understanding the patient and carer experience might be a good place to start.
Tuesday January 22nd 2019
Patient powered resilience
We all know that our healthcare system struggles at times. Newsfeeds routinely contain stories of workforce pressures, finance pressures, and - at this time of year - winter pressures.
The answer, according to some, is "resilience". But what does that actually mean?
For the authors of this paper, resilience "is an attribute of a system that allows it to flex and adapt to unpredictable circumstances". They explain that "flexibility may be what is needed to allow care delivery to meet the needs of varying conditions, to produce positive outcomes, and importantly, to support more patient-centred care".
That might sound like a cue for hollow laughter from staff trapped in highly inflexible IT systems, reporting requirements, management procedures and so on. But help might be available from an unexpected direction - the patients.
The paper observes that patients, families and carers sit within and outside and across organisational boundaries. "Their movement across... boundaries means that they are uniquely positioned to understand how different system components work, often in ways that elude the understanding of professionals".
From this perspective, they may be able to act as knowledge brokers, filling structural holes and helping to "manage the inconsistencies and unwanted variability in the care system".
Examples include "undertaking their own reconciliation of their medications following discharge from hospital, or proactively contacting their GP or community pharmacy where medications have been changed".
Patient and public involvement is often thought of in terms of how to "reach out" to service users, and encourage them to contribute to professional agendas for service delivery. But this paper argues that "What is needed is to provide everyday opportunities for [patients] 'reaching in' to healthcare systems", bringing with them "a unique source of insight and resilience".
Tuesday January 15th 2019
Patient, study thyself
Patient and public involvement (PPI) is a topic frequently discussed by health professionals and researchers. Good practice and ethics are important considerations - so the debate is often about how to "empower" patients, rather than simply exploit their experience and goodwill.
But what happens if patients stop waiting to be empowered, and simply start conducting research on themselves, and on their own terms?
The idea may sound bizarre - dangerous even. But modern medicine is built, at least in part, on knowledge gained by pioneering doctors who have experimented on themselves. So if it's ok for doctors, why not for patients?
This paper outlines examples of patients with complex medical conditions who - singly or in groups - have tested drug treatments, monitored disease progression, and developed home-made technological devices. They have published their results - not through academic journals, but through online forums which also offer shared knowledge and peer support.
We have previously discussed the way in which health professionals debate different types of patient/public involvement, without necessarily realising that their own roles can chop and change in the process. Is it time for professionals to stop talking about how they "involve" and "empower" patients, and start talking instead about how they partner with, and learn with patients?
Let's be clear: we do not advocate patients experimenting on themselves. But as this paper shows, some patient groups are heading in that direction. Health professionals - and their debates - may need to find ways to keep up.
Monday January 7th 2019
Tattoo you
We're starting 2019 as we mean to go on - with an edition of our quarterly magazine packed with news, views and insight.
Our contributors include the Mighty Casey Quinlan - activist, comedian and cancer survivor. Tired of hearing empty promises about better record-sharing with patients, Casey devised her own version of an electronic health record via a QR code tattooed to her chest.
We're not recommending that other readers take such radical action! But we see Casey's assertive stance as similar to the #wearenotwaiting movement, whereby patients stop waiting to be "empowered" and simply take matters into their own hands.
Our other contributors - Jen Gilroy-Cheetham and Leigh Kendall - take their own stances on the need for health professionals to understand what matters to patients.
Jennifer makes the point that "The day to day activities and rituals that are familiar to staff, aren't for the patient". Her request is that staff take the time to make sure patients understand - really understand - what is happening. For Leigh, "Great communication isn't automatic, it's something you fight like hell to achieve". One example is that with death being a taboo topic, staff may prefer to avoid talking about it. But assumptions about patient sensitivities can be disempowering and - ironically - insensitive.
The magazine also includes some excellent studies and surveys that have been published over the last few months. At the risk of blowing our own trumpet, we have included a couple of our own pieces that were picked up by the Journal of Clinical Nursing and the Canadian think tank, Policy Options.These make the case for an evidence-based approach to patient experience, and suggest ways in which the evidence could be better organised, and therefore better used.
We have various plans and projects in the pipeline for 2019, and will reveal them via this newsletter over the coming weeks. But for now, put the kettle on, download your copy of the magazine, and enjoy!
Tuesday December 18th 2018
Singalong patient engagement
Since we launched the Patient Experience Library, we have catalogued over 50,000 documents on patient experience and patient/public involvement. This one may be the most genius, or possibly the most bonkers, of the lot.
The authors note that patient engagement in research (PER) is "still an emerging approach with debated definitional and operational frameworks".
However, rather than add to the plethora of conceptual constructs, this team has produced "an impressionistic illustration of the challenges and issues that can be found in the universe of patient engagement in research".
Basically, they have made up a song.
Better than that, they have set it to the tune of a 90's hit single, "What is Love", by Haddaway - a song described by Billboard magazine as a "glorious pop/house ditty".
The original contains such deathless lyrics as, "Baby, don't hurt me, Don't hurt me no more, What is love? Yeah". But the reworked version achieves far greater heights of emotional intensity, addressing "themes related to PER operationalization as well as the obstacles and pitfalls in rebalancing the researcher-patient relationship".
The paper states that "Too often, patients and researchers live in parallel realities". In the new lyrics, that tension is "evoked by the repetition of the same questions and incessant requests to get an explanation of what PER really is and what actually goes wrong". That, surely, is something we'd all like to know.
This is a great paper which we thoroughly recommend to all our readers. If you want the tune, you can get it here, along with some not at all clichéd imagery.
Beware - once you start singing this song, you'll never stop.
Tuesday December 11th 2018
Hot spots and blind spots
Our featured report last week looked at the overwhelming nature of patient feedback. It described how hospital staff struggle with a mass of feedback from multiple sources. They reported "feeling overwhelmed and fatigued by the volume and variety of data that the Trust collected".
Formal complaints are one of the sources of feedback - but the authors stated that "it was rare for complaints to be used as grounds for making improvements". The focus was on "the timeliness of response to complaints and on trying to reduce the volume of them rather than an understanding of what an effective response looked like". Part of the problem was that "staff did not have the required skills to be able to perform sophisticated analytic tasks on the data they received".
This week's paper tackles similar issues. It makes the point that complainants are often motivated by the desire to "correct an ongoing problem or prevent recurrence". Importantly, they can have "valid information that the institution does not know or has failed to take sufficiently seriously". However, "The use of health care complaints to improve quality and safety has been limited by a lack of reliable analysis tools and uncertainty about the insights that can be obtained".
The solution, according to the authors, is to develop data-driven approaches to understanding and learning from complaints. The method involves focusing on three key areas: harm hot spots, near-miss hot spots, and institutional blind spots.
Hot spots of serious harm were safety problems during examination, quality problems on the ward, and institutional problems during admission and discharge. Near misses occurred at all stages of care - and the authors found that patients and family members were often involved in error detection and recovery.
One type of blind spot is hospital discharge, where transfer of care, sometimes involving multiple services, can lead to errors which may go unnoticed by providers while being obvious to patients. Crucially, "the more stages and staff groups a patient trajectory entails, the more likely that the patient is the only person who was present for each encounter. Accordingly, health care complaints are particularly suited to providing insight into continuity of care issues".
Unusually, the research did not confine itself to simply exploring the issues. In this case, the researchers went further - developing an analytical tool and testing it in the course of the study. Healthcare providers wanting to get a better understanding of complaints would do well to take a look at it.
The authors conclude that "health care complaints provide added value because they are patient-centred, focus on problematic care episodes, and provide an end-to-end account of care that includes concrete details not captured in incident reports or case reviews".
Tuesday December 4th 2018
The overwhelming nature of patient feedback
"All feedback collected ideally needs to have the ability to be meaningfully used by those providing frontline care. Otherwise, it becomes unethical to ask patients to provide feedback which will never be taken into account."
So say the authors of this paper, which visited three hospital sites to ask "what is impeding the use of patient experience feedback?"
It might come as no surprise to hear that "the most striking element is the overwhelming nature of the industry of patient experience feedback. Ward staff... reported feeling overwhelmed and fatigued by the volume and variety of data that the Trust collected".
Difficulty in managing the sheer volume of feedback was compounded by other factors including:
- layers of hierarchies and bureaucratic processes surrounding data collection which were said to be to be confusing to staff and patients alike.
- not enough staff or appropriate expertise... to be able to work effectively to produce meaningful conclusions from the data they received.
- fractured and disparate teams [who] struggled to make sense of the data or to be able to assist ward staff to do so.
Furthermore, "timeliness was seen as one of the main concerns with it being difficult to engage ward staff with data that are not real time. A specific example of this is the NHS Inpatient Survey where patient feedback is viewed months after it has been collected".
These practical barriers to making use of patient experience feedback sit alongside a cultural barrier within the hospitals that were studied. "Patient experience was sometimes said to be the poor relation of patient safety and finance with a lesser emphasis and priority placed on it."
According to the paper's authors, "The participants interviewed for this study nearly all saw an immense value in patient experience feedback, and most believed it should receive a high priority at a strategic and Trust board level".
However, they "largely seemed powerless to prevent the tsunami of ongoing data collection". They know that "staff find interpretation of data sets difficult or impossible... but there was no strategy in place or forthcoming at any of the three organizations we studied to address this issue".
Tuesday November 27th 2018
Parity of esteem - not yet
At the start of 2017, Prime Minister Theresa May announced that it would take years to improve mental health services. What she didn't say was that services would get worse before they got better.
Evidence of worsening quality comes from the Care Quality Commission's newly released patient survey for community mental health services, which shows that patient experience has deteriorated across several areas.
In some areas, this represents a continued negative trend, with a consistent decline in results since 2014. In other areas, the results declined significantly this year, having remained relatively stable between 2014 and 2017.
The news is not all bad. There has been a steady improvement in people's awareness of who to contact out of office hours when having a crisis. And better than average experiences were identified for people diagnosed with a psychotic disorder. Against this, though:
- Only 43% of respondents had 'definitely' seen NHS mental health services enough for their needs in the previous 12 months.
- The percentage of respondents who "definitely" felt that staff understood how their mental health affects other areas of their life had decreased.
- People's experiences of how services plan their care are at their lowest point since 2014.
As far as overall experience is concerned, 71% of respondents felt they were "always" treated with respect and dignity by NHS mental health services. This compares with 82% of adult inpatients in acute hospitals (physical health), who felt they were "always" treated with respect and dignity. It seems that "parity of esteem" is still some way off.
The report can be downloaded via our website and you can see the results for your local area via our Patient Experience in Trusts map.
Tuesday November 20th 2018
Alone in a crowd
Rare diseases are those which affect fewer than 1 in 2,000 people. And while individual diseases might be rare, there are considerable numbers of people within the population as a whole who are living with a rare disease.
Around 80% of rare diseases affect children, and almost half have their onset in childhood - so this Canadian study turns its attention to the experiences of parents whose child has a rare disease.
The study found that parents shared common experiences of navigating the healthcare system - despite the uniqueness of their children's diagnoses. Main themes were "the diagnostic journey", "seeking and accessing services", and "peer support".
For diagnosis, parents described a complicated experience, with numerous doctors' appointments and persistence in their pursuit of a definitive diagnosis for their child. But receiving a label or diagnosis was not the same as receiving help. Many parents felt that they were left with the responsibility of figuring out their next steps, and adopting the role of care coordinator. Given the complex health needs of their children, most families had interactions with many specialists and health services. A common experience was the lack of formal care coordination and communication between healthcare providers.
Parents also spoke about the barriers they faced in accessing services. Sometimes the processes they had to follow to access services were challenging to understand and could create contentious relationships with healthcare providers. Accessing services also led to employment changes for some parents. One reported missing months of work and leaving the workforce due to her child's hospitalisations.
Peer support from other parents of children with rare diseases emerged as a key resource. Even though most children had unique diagnoses, parents found that their experiences of navigation and coordination of healthcare services were similar. Social media was considered a good way to connect because their children's intense care needs often meant parents were not able to attend groups in person.
The paper concludes that "the broader research mandate about rare diseases must move beyond diagnostics and treatment to address the very real and pressing issues that arise from the patient - and by extension family - experience in navigating healthcare systems".
Tuesday November 13th 2018
The feedback avalanche
What does good patient experience look like?
That question is easily answered by staff who work face to face with patients. Smiles, thank you cards and boxes of chocolates are visible signs that a patient's experience has been good. But at the organisational level, it can be much harder to understand how patients are experiencing service quality.
We tackled this topic for an editorial in the latest issue of the Journal of Clinical Nursing. With colleagues from the universities of Exeter and Brighton, we tracked some of the policy drivers for patient experience work, and looked at how healthcare organisations have tried to turn policies into practice.
It is clear that serious efforts are being made to hear the patient voice. But we take the view that in seeking to meet the call that 'something must be done' the system has created an avalanche of patient feedback. The result is information overload, with patient experience staff sometimes struggling to keep up with the flow of data.
In fact, oversupply of information need not be a problem. Clinicians have management information systems that help them make sense of complex data. They have clinical databases that make research accessible and searchable, and they can look up clinical guidelines that help them remember key practice points.
The material on patient experience, however, has not been so well organised.
We think that the NHS needs to systematise its efforts, focusing on how things work from the patient's viewpoint, rather than validating existing practice through a ticking of boxes.
A rethink is needed on how we tap into patient experience. A rethink that takes account of these challenges and acknowledges the possibility of unpalatable answers which may disturb, or at least question, the current balance of power between organisations, professionals and patients.
This is not a shot in the dark. There are encouraging omens. And we all have a part to play in this agenda.
Tuesday November 6th 2018
Health care can't be patient centred without evidence
We're delighted to see interest from Canada in the work of the Patient Experience Library. Canada has a thriving patient engagement/advocacy culture, which we have flagged up in previous newsletters, and via comment pieces in our quarterly Patient Experience magazine.
So we are pleased to see one of our own comment pieces published on the influential Policy Options website. Miles Sibley, a Director of the Patient Experience Library, makes the point that if the NHS wants to be patient-centred, it has to understand patient experience. And that means it has to work from the evidence.
That may sound obvious. But it begs the question, "where is the evidence held?" The answer is that patient experience evidence is published across hundreds of different organisational websites, all of which are designed and structured differently, and some of which are not well maintained.
Even dedicated patient experience teams can find it hard to keep up - and the problem is that if you can't find the evidence, you can't act on it.
We built the Patient Experience Library to tackle that problem, starting with the rationale that if clinical research databases are feasible, why not a patient experience research database?
We're pleased that national NHS organisations are using the library. But we really want to see it opened up to patient experience teams, patient representatives, local Healthwatches - in fact, anybody with an interest in patient experience and patient/public involvement.
We'll keep working on that - and will aim to make the point at a meeting with Secretary of State Matt Hancock soon. In the meantime, our message to colleagues in Canada and elsewhere around the globe is simple: if clinicians can have comprehensive evidence bases to work from, so can patient experience workers.
The full article can be seen here.
Tuesday October 30th 2018
Emotional feedback
The latest edition of our Patient Experience magazine opened with the observation that one of the biggest make-or-break factors for quality of patient experience is "communication". With impressive timing, NHS England have promptly released a new guide on how to seek feedback in distressing or highly emotional situations.
The document adds to the Bite-Size Guides series , some of which we have featured previously, and all of which provide useful summaries for busy practitioners.
The guide considers the ethics of asking people for feedback when they are very upset - for example after a bereavement. Might questioning them at such a time be intrusive, or make them feel worse? Conversely, it considers the ethics of not helping people to talk about their experiences - of effectively excluding them from a process that should be open to all.
They may be no simple answers to these questions. But the guide considers matters such as timing, methods, and people's capacity to discuss their experiences - especially if they are both unwell and distressed.
As always, it is crucial not to treat feedback as a tick-box exercise. The guide makes the important point that feedback "is a way of creating a humanising atmosphere and improving relationships between everyone involved".
Conversations with people who are angry or upset may not be comfortable. But we are reminded that people "feel that sharing their experience can help improve the experience for others". And in some situations, "the opportunity to provide feedback can be a way of intervening before frustrations boil over, or can form part of the healing process".
Tuesday October 23rd 2018
Just one thing after another
It is well known that one of the big challenges to our healthcare system is the increasing number of people living with long term health conditions. This is one of the key factors propelling health and social care towards greater integration of services, as well as initiatives designed to help people "self-manage" their own health in their own homes and communities.
The drive towards self-management is not without risk, and we have previously looked at the extent to which self-management could place additional burdens on patients, rather than empowering them.
So this report from the Taskforce on Multiple Conditions is a welcome addition to the literature - not least because it takes an ethnographic approach, as opposed to exploring clinical perspectives and interventions.
The report's key question: "What is it really like to live with several long-term conditions that can be managed but not cured?" is explored through ten in-depth interviews. The interviewees represent a range of demographics and locations across England.
The authors make the point that "many people... seeking support with one condition are also living with other conditions and too often experience siloed, condition-based, care and support". It also notes that "The point at which each person goes from one to many health conditions... seems to track issues of deprivation, culture, lifestyle and place".
The report concludes that three basic principles - mobility, active involvement in care planning, and regular goal-setting - are fundamental to helping people with multiple long-term conditions to achieve a good quality of life.
"Patient experience" work often concerns itself with people's access to, and satisfaction with, services. This report, by contrast, starts with the person rather than the service(s) they use. The result is a person-centred view of patient experience - and a useful set of insights.
Tuesday October 9th 2018
Patient Experience and patient/public involvement in health and care services - Autumn 2018
Across health and care services, one of the biggest make-or-break factors for quality of patient experience is "communication".
That can mean written or verbal communication. It can mean the use of medical jargon, as against language patients can understand. It can mean communicating in accessible ways - sign language or easy-read for example.
But sometimes, it can be about sensitivity and tone of voice. And it can be as much about what is not said as what is.
Our contributors to the autumn edition of Patient Experience Quarterly all remind us of the importance of good communication.
Vidhya Alakeson, bringing her elderly father home from hospital, could have done with help to understand what his care needs at home were going to be, and help to understand the roles and responsibilities of multiple health professionals involved in his post-discharge care.
Joanne Hughes, a bereaved parent, asks for a kinder and more healing dialogue with the health professionals who could have helped her to understand why her daughter died.
Julia Jones describes the experience of having to stand up for her mother against health professionals who seemed to be following rigid procedures rather than getting to know their patient.
It has been estimated that poor communications cost the NHS in excess of £1 billion per year. But these stories reveal the kinds of human cost that can never be counted.
Evidence on patient experience comes both from personal testimony and from formal studies. So our magazine also features our top picks from recent surveys and research, with summaries of learning points, and links to the original documents.
We're always keen to hear from our readers, so if you know of a standout report that we should be featuring, or if you want to submit a comment piece, get in touch! info@patientlibrary.net
Tuesday October 2nd 2018
Speaking up in the ICU
Intensive care units (ICUs) are places where "stakes are high and time is compressed" according to this study from America. So the ability of patients and families to voice concerns may be of more pressing importance than in other care settings.
The paper opens by rehearsing some familiar arguments about why people need to feel comfortable in asking questions or raising concerns. These include understanding the risks and benefits of care, and consenting to treatment on the basis of informed choice. Safety is a factor, as "families - vigilant stakeholders - may be the first to detect a change in a patient's clinical status". And families can help to ensure continuity of care as medical team members come and go.
All of this "may be particularly important in the intensive care unit , which provides high-intensity, high-acuity, error-prone and preference-sensitive care". But, say the authors, "voicing concerns in the ICU can be problematic for patients and families: the physical environment may be perceived as strange or dangerous, patients are at high risk of death, power asymmetries are extreme, multiple clinicians and teams are involved, and the complexity of care may be overwhelming".
The study appears to be the first to address family comfort with speaking up in the ICU. And worryingly, it found that 50%-70% of patients and families "expressed hesitancy to voice concerns in real time about some common care situations with safety implications, including a possible mistake or mismatched goals related to aggressiveness of care".
The authors sort patient-perceived barriers to speaking up into three types: mechanistic (how to do it), contextual (team is too busy) and cultural (fear of being a troublemaker).
Their conclusion is that "Educational strategies should include both encouraging and supporting patients and families to voice concerns with clear steps and a genuine invitation, and preparing clinicians to respond meaningfully when patients speak up".
Tuesday September 25th 2018
Power, ceremonies and the unconscious mind
All users of health services know the experience of sitting in a waiting area. And many know the experience of sitting there long after your appointment time has passed, wondering when you might be seen. NHS England's GP Patient Survey, for example, consistently shows 1 in 3 patients reporting waits of more than fifteen minutes beyond their appointment time.
This week, we have dug back into our archive for a 2012 paper that asks why healthcare bookings so frequently overrun.
John Launer, the paper's author, is not convinced by references to staff capacity, unpredictable patient needs and so on. "Consultation lengths and emergencies do vary, but they have a statistical pattern... so you can adjust your booking system accordingly; it's just that most institutions don't bother to do so."
Furthermore, "Some doctors regularly finish an hour or two late, yet their patients are still stacked up for appointments every session without the remotest chance they will ever be seen on time".
For Launer, keeping patients waiting is not about practicalities, but power. Clinics are run in such as way as to "send clear signals to patients that we are the people who make and apply the rules, and they are the ones who are obliged to comply".
Power is reinforced by ceremony and ritual - for example, "when doctors emerge every few minutes from consulting rooms to retrieve a set of notes and then vanish again, it has a close resemblance to a Greek orthodox priest disappearing behind the icon screen".
Exploring unconscious organisational culture, Launer notes that workplaces can feature controlling behaviour and even destructive tendencies. Waiting rooms can therefore be places "where we have licence to treat patients badly, and to make up credible excuses for doing so".
Healthy healthcare organisations are ones where professionals "behave more compassionately towards patients, and indeed towards each other". They can then "feel free to start changing dysfunctional systems that seemed unchallengeable, or just part of the natural order of things".
For Launer, "An improvement in waiting times would be a good place to start".
Tuesday September 18th 2018
Rethinking engagement
Traditional methods of gathering patient feedback are "stuck in child-parent mode", according to this thought-provoking editorial from the British Journal of Psychiatry Bulletin. The author, David Gilbert, writes from his experiences as both professional and patient, and calls for a fresh approach to patient engagement.
For Gilbert, "Patient and public engagement, as traditionally conceived, buffers power by distancing patients from decision-making".
With conventional patient feedback, people are invited to "fill in questionnaires, attend focus groups or tell their stories... The focus is what happened to them in the past, mostly about their experience of services (rather than living with a condition, or about their lives beyond the institutional scope of interest)".
Subsequently, "the meaning of their data is left to professionals to assess... based on... institutionalised thinking (often what is seen as feasible rather than necessary)".
Gilbert makes the important point that "Patients are not permitted to eyeball the data or bring their own interpretations to it". At the local level, patient access to feedback data may vary between Trusts and CCGs. But at the national level, Gilbert's observation chimes with our own view that feedback data is held by so many different organisations in so many places and so many varying formats that even dedicated patient experience staff can struggle to keep up with it all. For patients and public, the task is nigh on impossible.
The editorial goes on to explore the "adolescent-parent" relationship engendered by committee processes that invite patient representatives but then marginalise their contributions. And it covers much extra ground besides, including a case study of a real-life exercise in rethinking engagement via the Sussex Musculoskeletal (MSK) Partnership.
Tuesday September 11th 2018
A letter from the doctor
In an important development for person-centred care, the Academy of Medical Royal Colleges is encouraging doctors to write outpatient letters directly to patients, copying in the GP. This reverses the traditional approach of writing to GPs and (sometimes) copying in the patient.
The move matters for two key reasons.
Firstly, it shifts the power balance. Patients become primary recipients of information about themselves. They are no longer positioned as bystanders in their own care, watching passively while professionals talk to one another above their heads.
Secondly, GPs benefit as well. The Academy states that "Doctors who have adopted the practice say their communication style has become more patient-centred. GPs find the letters easier to understand and spend less time interpreting the contents for the patient".
The new guidance does not come out of the blue. It reflects statements about patients' rights in the NHS Constitution, and GMC guidance on good medical practice. And while it is based in policy, the Academy recognises that it cannot take implementation of the guidance for granted. It calls on "hospital trusts and clinical teams to support this initiative and provide help and training to all who need it".
Addressing letters to patients first and GPs second may seem like a very small step. It is certainly one that should be achievable at little or no extra cost. But culturally, it marks a significant shift. This is an important piece of guidance that should be required reading for Trust Boards.
Tuesday September 4th 2018
Patient experience and hot cakes
Our Patient Experience in England report has been going like hot cakes from our website - not that we can claim much of the credit!
The report's content is assembled from some excellent work that has been produced over the last twelve months via national patient surveys, academic research, think tanks and official inquiries. All we have done is collate and curate it. The result is a compelling overview of the state of patient experience and patient/public involvement in England.
The report itself is just the very tip of the iceberg of patient experience evidence. We have added thousands of reports to the library over the last year, and continue to add more every week.
A year ago, when we published our first such report, we said that we had three ambitions:
1. To offer a single point of knowledge on patient experience and patient/public involvement. Much of the evidence resides in the realms of "grey literature", and it has been far too difficult for people to track it down. We want to make it much easier to find.
2. To preserve the literature. Over a forty year period, Community Health Councils, PPIFs, LINks and now Healthwatch have made valuable contributions to the collective intelligence on patient experience. But there has been no archive, so vital knowledge has been lost. Without access to their own history, health services risk repeating the same mistakes. We want to help them learn from past experience.
3. To give patient experience leads parity with clinicians. Happily, clinicians have open access to professional databases to guide their practice and professional development. Unhappily, patient experience leads don't. We want to help even up the professional playing field.
Those three ambitions remain true, and we're looking forward to working through the autumn with the people and organisations who have inspired and encouraged us. Some of those are listed on page 3 of the report, and we'd like once again to offer them our thanks.
Wednesday August 29th 2018
Patient Experience in England
NHS strategies, from the Five Year Forward View down, state that an understanding of patient experience is central to development of "person-centred" services.
But our 2018 Patient Experience in England report shows that staff teams across the NHS continue to struggle to make sense of patient feedback.
The report draws on surveys and research carried out over the last twelve months by bodies including the Care Quality Commission, NHS England, and academic institutions. It shows that:
- Patient feedback could be used to drive improvement - but enthusiasm for its collection is not matched by the capacity to turn data into insight.
- Phrases like "person-centred" and "patient involvement" are poorly defined, leading to unhelpful simplifications and difficulty in evaluating different approaches.
- There are clear links between staff experience and patient experience. For example, when patient loads are high, 65% of nurses are unable to comfort or talk with their patients.
The report covers other areas such as the Gosport Inquiry and "learning from deaths" work over the last year. And it looks to the future, with consideration of how machine learning might help the NHS to keep track of the large volumes of patient feedback now coming in via social media.
Tuesday August 21st 2018
The evidential value of lay knowledge
"They seem to need a disaster to change regulations, rather than evidence".
This 2013 quote comes from the secretary to the Parliamentary Fire Safety and Rescue Group, after government had ignored the Group's recommendations on fire safety in tall buildings. Four years later, Grenfell Tower burnt down.
Warnings about the specific risks at Grenfell Tower had come from residents and from the Grenfell Action Group. But their "lay knowledge" of the building's attributes was not acted on.
This scenario would be familiar to patients and relatives at Mid Staffordshire, Morecambe Bay, Southern Health or Gosport. In each of those cases, evidence - in the form of personal observation, feedback and complaint - was ignored until it was too late.
Our featured report this week is a short paper which considers the question of lay knowledge, and the extent to which it is recognised - even permitted - by professionals.
The authors trace the value of people's experiential knowledge all the way back to Aristotle, who described it as "practical wisdom". But they say that lay knowledge can be marginalised in policy and practice.
Sometimes this is because it is seen as "oppositional discourse", of a "political nature". It can also be because "the evidence movement remains obsessed with a hierarchy in which quantitative research-based knowledge reigns supreme".
This means that "Knowledge... can be used to... exercise discursive power in ways that privilege some definitions of health and social problems and marginalize others".
The opinion of the authors, however, is that, "Like all evidence, the 'trustworthiness' of experiential knowledge should be assessed... but it should not be ignored."
Tuesday August 14th 2018
GP patients move online
The 2018 GP Patient Survey offers some good news, with generally high levels of satisfaction at the NHS's front line of care. 93% of patients felt involved in decisions about their care and treatment. 87% felt their healthcare professional was good at treating them. And of everyone who wanted a same day appointment, 66% got one.
The survey method has changed this year, which means that comparison with previous years' results is problematic for some questions. So we looked at patients' online access to some aspects of GP services, but had to take previous years' results as a general contextual guide rather than a statistically reliable result.
With that caveat, it would appear that fewer people are booking appointments by phone (78% as opposed to 86% in 2017). But more are booking online (10%, against 9% in 2017 and 7% in 2016).
Growing numbers are also aware that they can access medical records online. In 2016, just 6% of patients knew this. In 2017, it was up to 9%, and this year, the figure has risen to 13%.
For repeat prescriptions, there is a similar trend. 14% of respondents had used online services in the last 12 months to order repeat prescriptions, up from 12% in 2017 and 11% in 2016.
Again, changes in the survey method mean that statisticians cannot be 100% reliant on a comparison of this year's results with those from previous years. But for practical purposes, GP practices can probably take it as read that more patients are looking for the convenience of online access, and that a good digital offer will contribute to a better patient experience.
Tuesday July 31st 2018
Living with and beyond cancer
This year's Cancer Patient Experience Survey brings encouraging findings, with significant improvements across a range of indicators.
91% of respondents said that they were given the name of a Clinical Nurse Specialist who would support them through their treatment. And 86% said that it had been 'quite easy' or 'very easy' to contact their Clinical Nurse Specialist.
Alongside that, 89% of respondents said that they were treated with respect and dignity in hospital, and 79% said they were definitely involved as much as they wanted to be in decisions about their care and treatment.
As always, it is worth comparing the survey's findings with patient feedback coming from other sources.
We revisited the recent CQC Adult Inpatient Survey, which reported that a quarter (25%) of patients thought their family (or someone else close to them) were not given all the information they needed to care for them after leaving hospital. That means that three quarters (75%) did feel adequately informed. But in the cancer survey, only 59% of respondents said that the doctors or nurses definitely gave their family or someone close to them all the information they needed to help care for them at home.
Additionally, the Adult Inpatient Survey found that less than two-thirds of patients (62%) left hospital with written information telling them how to look after themselves post discharge. For the cancer survey, patients were asked if they had a written care plan, but found that only one third (35%) said that they had been given one.
Since NHS strategies stress the importance of "self-management" for people with long term conditions (including living with and beyond cancer) the issue of information-giving is crucial. Differences in the way questions are asked may mean that the Cancer Patient Experience Survey and Adult Inpatient Survey are not directly comparable. But the similarities are striking, and taken together, the surveys seem to be pointing to an area that is ripe for improvement.
Tuesday July 24th 2018
Stories or numbers or stories and numbers
A few weeks ago we suggested that the Gosport Inquiry should finally bring to an end the idea that patient stories are simply "anecdote", carrying less weight than the "hard" evidence of statistical data.
This week, we have dug back into our archive to revisit the issue via a conference presentation by the always excellent Prof. Trish Greehalgh. Using the 2014 Ebola crisis as a case study, Greenhalgh shows how stories can use numbers, and numbers can tell stories.
So the Ebola story can be told from the point of view of an orphaned child, to make the case for better support for survivors of all ages.
It can also be told from the point of view of front-line medics and aid workers, to make the case for more emergency aid.
There is another point of view - the story about development of treatments and vaccines. This version can be rolled out to make the case for more medical research.
These stories can be told by real people - the child, the aid worker, the researcher. If need be, their stories can be reinforced with statistics on numbers of orphans, the scale of the emergency response, the cost of developing vaccines and so on.
Alternatively, the statistics can be presented on their own - as objective fact, coupled with sober social, economic or medical analysis. But even so, the numbers are being used to tell a story.
Coming back to patient experience, the point is that stories and statistics are always being pressed into the service of a particular narrative.
We can test the veracity of both patient stories and statistics. We can look at whether stories and statistics complement or contradict one another. But we should never assume that one form of evidence is always, and inevitably, better than the other.
Tuesday July 17th 2018
How PPI changes professionals
People with an interest in patient and public involvement (PPI) spend a lot of time talking about definitions.
There is, for example, the question of whether members of the public should be described as "patients", "service users" or "consumers". Another question is whether they are "involved", "engaged" or "participating". Deeper debate considers whether people are "co-producers", "co-creators", or simply "experts by experience".
What all of these debates have in common is that they reflect a discussion among health professionals about the status of patients.
Language reveals culture. And the debate about how to describe PPI reveals a culture in which power is firmly held by health professionals. It is about how those who hold power choose to define the terms on which patients and public will be invited to the table.
Our featured report this week makes the often overlooked point that "measures to strengthen the position of service users not only change the position of the users, they also alter the position of the professionals involved". The paper examines different types of involvement, and their implications for the positioning of professionals.
So efforts to encourage self-management of long term conditions may be framed as empowering patients through self-determination and participation in decisions about their own treatment and care. This positions health professionals as educators, advisers and supporters.
Efforts to encourage sharing of lived experience can move professionals into a different position. In professionally-led groups, they can be seen as facilitators. In self-help groups, they may have no role at all.
Finally, in efforts to improve services through awareness of user perspectives, the service users may take the role of educators, while professionals become positioned as learners.
Health professionals managing PPI activities will - rightly - continue to debate the nature of public involvement. But they should not assume that their own role and purpose runs unchangingly through different types of engagement. Whether they know it or not, the very act of engagement changes their own position and status as much as that of patients.
Tuesday July 10th 2018
What actually is peer support?
Read any NHS strategy and sooner or later you'll come across a reference to the fact that more and more people are living with long term health conditions. The favoured responses involve "self-management" - enabling people to look after themselves by, for example, monitoring and medicating their condition.
Children with long-term conditions will get help from parents and carers. But at school and in friendship circles, they may also look for "peer support".
This study asked pre-adolescent children with Type 1 diabetes what peer support actually meant to them.
Virtually all children described having a small number of close friends who were interested in learning about, and helping with, their diabetes. These friends provided support in three overlapping ways.
"Monitors and prompters" offered reminders of diabetes-related routines (eg blood glucose self-monitoring or administering insulin), for example on occasions when the diabetic child became so engrossed in activities that they lost awareness of time.
"Helpers" offered practical support - for example, by alerting adult caregivers when a friend needed assistance to manage hypoglycaemia.
"Normalizers" might make adaptations to their own lives so that friends with diabetes need not compromise self-management activities to fit in. One example was a girl whose friends delayed having lunch at school until she had completed self-management tasks so they could eat together.
Interestingly, the children interviewed were ambivalent about meeting other children with type 1 diabetes at organized groups or events. Some children speculated that speaking to peers with diabetes might help reduce social isolation, but several cast doubt on whether such encounters would lead to lasting and supportive relationships. One girl said that she would prefer to develop friendships of her own volition rather than as a result of being brought together on the basis of a shared disease status.
Tuesday July 3rd 2018
Advocate me
You probably know a powerful patient advocate. The sort of person who seems to have boundless energy, expert knowledge, and an ability to tell it like it is. But what happens when experts by experience have their own moments of vulnerability?
In the summer edition of our quarterly magazine, Sue Robins talks of her experience of moving from patient advocate to cancer patient. Her account is a powerful illustration of how independence and assertiveness can dry up in the face of illness.
Patricia Cantley tackles similar themes. Her parents had to summon up their courage to ask questions about their son's care - fearing, among other things, that any complaint might affect their daughter's prospects as a medical student.
We have to remember how hard it can be for patients and relatives to say what matters to them. The people who are actually voicing concerns may just be the tip of the iceberg.
Our third commentator, Martin Taylor, has Parkinson's Disease. He is one of the growing number of people living with long term health conditions. It is important that their experiences are understood, which is why many charities and patients' groups run awareness raising campaigns. But do such campaigns work? Martin questions their effectiveness, and suggests a different approach.
The magazine carries our usual top picks from the evidence base on patient experience and patient/public involvement - and last but not least, our NHS@70 gift to our readers is a specially commissioned set of patient experience posters.
Tuesday June 26th 2018
Gosport: An end to anecdote.
Gosport must - surely - be the point at which dismissal of patient feedback as "anecdote" finally comes to an end.
NHS culture is much better than it used to be. Patients are now encouraged to give feedback - and complaints, compliments and concerns are seen by the best providers as learning opportunities. But in a science-driven system, there is a lingering sense that "hard" evidence - statistically based - is more reliable than the "soft" stuff of patient stories.
We cannot go on with this dangerous and damaging myth.
A 2015 report from Dr. Foster explored the uses and abuses of performance data in healthcare. It found plenty of ways to manipulate statistics, including bullying of staff, "gaming" waiting time and mortality data, distorting patient pathways to meet treatment targets, and arguing about data quality in order to divert attention from poor care.
At Mid Staffordshire, the Healthcare Commission (predecessor to the CQC) followed rigorous inspection criteria and gave the Trust a clean bill of health. The Trust's Board were looking at key performance indicators that showed steady progress towards Foundation status. But it was patients and relatives, with no statistics, no performance data, and no research methodology, who got much closer to the truth of what was happening on the wards.
Even when statistics are reliable, professional and organisational fear can put reputation before truth. At Morecambe Bay and Southern Health, and in the Hyponatraemia inquiry, defensiveness, collusion and cover-up were common factors. Patient stories may indeed be unreliable at times. But, sometimes, the same can apply to professionals' stories.
We need to end the reverence for statistical evidence, and accept that it can, sometimes, be flawed. And we need to stop seeing patient testimony as "soft" and acknowledge that it can, sometimes, provide better insight than the numbers.
The plain fact is that qualitative and quantitative evidence, taken together, give us the best chance of getting an all-round understanding of how well our healthcare systems work for patients.
For too long, patient feedback has been described as "anecdotal evidence". After Gosport, we need to recognise that it is, simply, evidence.
Tuesday June 19th 2018
Adult inpatients: Problems persist.
Last week saw publication of the latest CQC national patient survey - this one providing fresh evidence on the experiences of adult inpatients.
We now have a nearly ten-year cycle of these surveys, enabling us to start getting a clear picture of patient experience trends over time. Encouragingly, there have been consistent improvements for how well doctors and nurses care for patients. 78% of patients said they "always" had confidence in nurses this year, compared with 72% in 2009. And fewer patients now say that doctors had spoken in front of them "as if they weren't there" (23% compared with 29% in 2009).
Hospital discharge, however, remains one of the weakest areas of patient experience for adult inpatients. 19% of respondents thought hospital staff did not take their family or home situation in to account when planning their discharge, while a quarter (25%) of patients thought their family (or someone else close to them) were not given all the information they needed to care for them after leaving hospital. Less than two-thirds of patients (62%) left hospital with written information telling them how to look after themselves post discharge, a figure which has deteriorated since 2013 (67%).
The problem is not just with hospital staff. 17% of survey respondents said they left hospital not knowing what would happen "next" with their care, and 22% said they did not receive enough help from health or social care professionals to help recovery or to manage their conditions.
These kinds of issues have been repeatedly highlighted in local Healthwatch reports, going as far back as 2013. If patient experience of hospital discharge remains poor, it is not for want of evidence.
Another persistent feature of the CQC patient surveys is that inpatients with a pre-existing mental health condition report a poorer experience of care across most areas of the NHS patient experience framework; information sharing, respect and dignity, coordination of care, confidence and trust, respect for patient centred needs and values, and perceptions of overall experience of care. We have highlighted this previously - and again, it is troubling to see the evidence mounting up but the problems remaining unresolved.
Tuesday June 12th 2018
Confronting Dr Robot
We have previously looked at ways in which artificial intelligence (AI) and machine learning might affect healthcare. Now a new report from Nesta adds to the debate.
According to the authors, AI could put patients more in control. But, they say, "there's a risk that the public could experience it more as a barrier than an open door, blocking access to care, offering opaque advice and dehumanising healthcare in every sense".
They say that "today's AI is narrow and not capable of the holistic thinking and complex judgement required for many clinical tasks". For them, "the path towards AI replacing humans is not solely determined by technical capability. Technology implementation will need to address trust, accountability and similar factors".
The report calls for a "people powered" AI for healthcare, based on principles of control, simplicity, dialogue, equity and accountability. These, it says, are "principles that apply to any form of healthcare that aims to be humane and person-centred". However, they "are not presently being applied to the design, development and implementation of AI".
The report recommends that "Policymakers should set rules for AI and ownership of public data that ensure the public gets not only value for any data it decides to share, and privacy elsewhere, but also AI products that deliver maximum public benefit".
Monday June 11th 2018
Power to the people
The Make Birth Better campaign is raising awareness of birth trauma, and calling for changes to maternity services. It is part of a long and proud history of women campaigning for better births.
Importantly, maternity campaigners have not just focussed on the practicalities of childbirth. They have significantly changed the culture of the medical profession. Concepts of choice and control, and the idea of partnership between patients and professionals are now part of the language of the NHS. But they stem, in large part, from the activism of women motivated by the desire for better experiences through pregnancy and childbirth.
Our guest blog on the Make Birth Better site makes the case for a comprehensive evidence base on women's maternity experiences.
All the work of the Patient Experience Library is based on an understanding that in healthcare, knowledge is power. Individually, women seeking better births can rely on personal experience and personal assertiveness. But women together - over time and across communities - need to be able to draw on collective experience and shared knowledge. And for that, they need access to the evidence.
The Library contains over 40,000 documents on patient experience and patient/public involvement. Several thousand of those relate to maternity. We want those to be freely available to patients, public, activists, researchers and, of course, health professionals.
We remain hopeful that NHS England will at some point see the value of the resource, and will want to support our efforts. But in the meantime, we're open to discussions with maternity campaigners about how to mobilise the evidence, and put more power into the hands of women and their birth partners.
Tuesday June 5th 2018
A raw deal for children
"Even taking into account the significant expansion in children's mental health services, workforce constraints mean that by 2020/21 we only plan on meeting the needs of a third of children with diagnosable mental health conditions".
This statement comes from the foreword to Lord Carter's review of unwarranted variations in mental health services and community health services.
The review considers a range of productivity and efficiency issues across various mental health and community health services. But let's stay with those children with diagnosable mental health conditions.
Back in 2016, the Five Year Forward View for Mental Health said that "too many people have received no help at all, leading to hundreds of thousands of lives put on hold or ruined, and thousands of tragic and unnecessary deaths". It spoke of "a real desire to shift towards prevention". But that desire sounds hollow in the light of Carter's revelation that two years from now, two thirds of children who may need treatment will have to go without.
Children who do get treatment for mental illness might be considered lucky - except for the fact that their experience, as patients, is consistently poor.
The Care Quality Commission's most recent Children and Young People's Survey found that patients with a mental health condition, and their parents and carers, reported significantly worse experience for matters including information and communication, transition and continuity, respect for patient-centred values, involvement of family and friends, and awareness of medical history.
At the start of 2017, Prime Minister Theresa May described mental illness as a hidden injustice. We have said before that the injustices are not hidden - they are in plain sight.
Lord Carter's review outlines ways in which productivity and efficiency improvements across mental health and community health services could save the NHS nearly £1 billion by 2020/21. Putting that saving towards better preventative work in children's mental health might be a good way to start addressing the injustices that the Prime Minister is so concerned about.
Wednesday May 30th 2018
15 steps for maternity
The Nursing and Midwifery Council has recently been consulting on its "fitness to practise" role - its work in regulating the safety and professionalism of registered nurses and midwives.
The consultation document states that "The context in which patient safety incidents occur is extremely important". It says that "By considering the context we are asking what caused an incident, rather than who is to blame".
This is vitally important, given the learning from major failures at Trusts including Mid Staffordshire, Morecambe Bay, and Southern Health. In every case, part of the context for avoidable harm and death was an organisational culture that devalued patient experience and dismissed the concerns of patients and relatives.
So the publication of NHS England's "15 Steps for Maternity" is timely, and welcome. The subtitle, "Quality from the perspective of people who use maternity services" points to its value in enabling the patient voice to be heard alongside regulators and inspectors.
The authors are keen to point out that the 15 Step Challenge is not a performance management tool or an audit. Instead, it aims to build an understanding of how people feel about the care provided, how confidence can be built by positive first impressions, and what might be done to increase levels of confidence as part of continuous improvement.
The challenge is based on a quote from the mother of a child needing frequent hospital admission. Her observation was that, "I can tell what kind of care my daughter is going to get within 15 steps of walking on to the ward". And sure enough, a series of practical guides prompt people taking the challenge to record immediate impressions of a healthcare service - taking in features such as "welcoming", "safe", "clean" and "calm".
Anyone who has read the report of the Francis Inquiry will know that these are powerful pointers towards the underlying wellbeing of staff, systems, and, ultimately, patients.
The 15 Steps Challenge has value in its own right as a means of getting service users' feedback. But it can also offer important clues to that vital question of "context" that underpins health professionals' ability to do their jobs safely and well.
Tuesday May 22nd 2018
PPI in a digital age
"We live in a digital age" says the opening statement to this report. And sure enough, the NHS is working hard to develop things like electronic patient records and telehealth, propelled by reviews including Wachter and Topol.
This report looks at ways to strengthen the voice of the citizen and patient within the process - not least because "the systems and processes that lead to the adoption of technology tend to marginalise the voice of most patients and the public".
This may be because "projects are nervous about involving the public, and are worried about adverse publicity, particularly in the wake of the Care.data scandal". But the report counters any such perceptions with real-life examples of successful approaches to involving patients and public in digital healthcare initiatives. These include:
Technology for bringing together patient data - including patient data sharing.
Technology for connecting directly with patients - including tools for self diagnosis and self management.
Technology for communicating and engaging with citizens. This includes crowdsourcing techniques and other forms of citizen science.
A series of case studies illustrate how these principles are being applied across the country, and the report is rounded off with a summary of key points of good practice, followed by suggested ways to strengthen patient/public involvement in the development of a digital NHS.
This is a good report that raises some important issues. And, following her own good practice recommendations, the author finishes with a call for interested readers to get in touch, to share ideas and continue the discussion.
Tuesday May 15th 2018
I could not survive another day
It is good to see NHS England's recent announcement of new funding for community perinatal mental health services. These will allow pregnant women and new mothers with mental health difficulties to access specialist services in every part of the country by April 2019.
We hope that the new services will be evidence-based - not just in terms of clinical need and treatments, but also in terms of understanding women's experiences through pregnancy and beyond.
So this week, our featured report is one that came out a few years ago but which is still highly relevant.
Hyperemesis Gravidarum (HG) is a severe complication of pregnancy associated with extreme nausea and vomiting. Other symptoms include headaches, heightened and warped sense of smell and extreme fatigue.
In addition to the physical complications HG can lead to depression and social isolation as well as financial and relationship problems, and women can feel they are less effective parents due to the condition. These complications in turn can lead to Post Traumatic Stress Disorder. Research indicates that around 10% (and possibly as many as 20%) of sufferers terminate otherwise wanted pregnancies for the condition.
This report describes the experiences of women who had ended pregnancies while suffering HG. 95% described their symptoms as "intolerable", and 84% said they would have wanted to continue with the pregnancy if they had not been suffering HG.
Shockingly, the researchers found that 47% of women did not receive treatment for HG. Of these, 40% requested treatment but were denied it, and the others did not ask for treatment and were not offered any. A quarter of women who were not prescribed medication reported that it was because their doctor said it would harm the foetus or there were no medications suitable for pregnancy.
The authors conclude that women are terminating wanted pregnancies because they are being denied antiemetic treatment. They state that women who have terminated due to HG carry a significant burden of guilt, remorse and often anger upon finding out subsequently that treatments are, in fact, available.
Hyperemesis Gravidarum is a physical health condition. But it is one which can have profound consequences for women's mental wellbeing - especially if the symptoms and medications are poorly understood by professionals.
As new community perinatal mental health services are rolled out across England, it is vital that they help to improve understanding of HG. That means listening to women's experiences, and recognising that better physical and mental health for HG sufferers may depend, as much as anything, on better professional responses.
Tuesday May 8th 2018
Hospital visiting Canadian style
It has been heartening to see calls for an overhaul of hospital visiting rules from Jane Cummings, Chief Nursing Officer for England. With the 70th anniversary of the NHS coming up, she thinks it's a good time to for hospitals to sign up to John's Campaign (for the right of people with dementia to be supported by their family carers) and pledge their welcome to carers.
According to Cummings, "A flexible approach to embracing the presence of carers has led to improving the overall experience of care, changing the atmosphere in wards and services, and helping to make best use of current resources. It has also led to better communication, fewer complaints, reduction in falls, violence, delirium, length of stay, improvement in hydration and nutrition, acceptance of therapy and medication, generally improved well-being and maintenance of function, complementing the work of the #endpjparalysis and the last 1000 days programme."
Over in Canada, the debate about hospital visiting has been going on for a while. Our featured report this week summarises the deliberations of a Better Together Policy Roundtable on the topic of "family presence".
The family presence approach aims to change the concept of families as "visitors" to families as partners in care in hospitals. It enables patients to designate a family member or loved one who can remain with them 24/7 and be a part of their care team. Families can be present during many aspects of the healthcare experience, including rounds, procedures and transitions.
The roundtable looked at the evidence supporting family presence, considered the current state of family presence in Canada, set about dismantling the myths and challenges of family presence, and looked at case studies of family presence policies.
It then moved on to equipping participants with knowledge about how to implement family presence policies across their organization or jurisdiction. The report says that "Participants left the second day of the roundtable with clear and actionable steps for beginning the process of adopting family presence policies within their jurisdictions or across their healthcare organizations".
We welcome Jane Cummings' call for a review of hospital visiting restrictions, and her clear support for the John's Campaign principles and pledge. We hope that this is just a first step towards the kinds of family presence approaches that the Canadians are championing.
Tuesday May 1st 2018
Better deal for PX staff - more evidence
We'd like to say thank you to everyone who liked, retweeted and commented on our BMJ Opinion piece last week, which called for a better deal for patient experience staff. A key part of our case was that PALS teams and others are swamped by patient feedback from multiple sources, presented in a bewildering variety of formats, and published across far too many different websites.
By happy coincidence, we spotted this paper last week, from a team of academics who have been looking at the "usefulness and use" of patient surveys.
There is so much good stuff in this paper that it is hard to know how to summarise it. Perhaps the best way would be via these direct quotes:
"The value of data for organizational quality improvement is not commensurate to the volume of data the system supplies. This misalignment is... in many ways, the consequence of national survey programs being set up to satisfy a national agenda rather than being designed with respect to local circumstances."
"... gleaning information from experience data requires the same analytical capability as interpreting clinical data; however, that capability is often unavailable. Staff across health systems consider patient feedback to be valuable but have neither the time nor the expertise to use it...".
"The paradigm regarding patient experience feedback is heavily rooted in large national initiatives... which are accompanied by a sluggish bureaucracy and political concerns. It is likely that these initiatives are neither capturing, nor producing, what is most useful to the organizations trying to use patient feedback to improve care".
"In order for patient-reported feedback to be an effective improvement tool, and avoid the ethical grey zone around soliciting patient input and not acting on it, feedback programs need to make efforts to facilitate data comprehension and use."
It's not that the national surveys are no good. In fact, they are packed with potentially useful data. Developing that potential, however, means giving patient experience staff the analytical tools they need. We have been doing some work on this and hope to develop some solutions. If you have thoughts on this matter, we'd like to hear them! Please get in touch at info@patientlibrary.net
Tuesday April 24th 2018
A better deal for patient experience staff
It is good to see NHS England running this year's Experience of Care week. Right across the country, patient experience teams are joining in with events, case studies, celebrations, and lots of activity on Twitter.
In an NHS that tends to be dominated by news of financial and workforce pressures, it's patient experience staff who remind us that what matters most is how patients experience the care they receive.
Our top message for Experience of Care week is simple: if staff have good experience of care, so do patients. A workforce that is nurtured, developed and supported will have a better chance of giving patients the best possible care.
Patient experience staff are central to this. And they deserve better support.
The NHS draft workforce strategy is bafflingly silent on this. It says that its purpose is "to put staff at the heart of a patient centred service vision". But it says nothing about patient experience staff - the very people who are best placed to help.
Happily, the BMJ is alert to this issue, and keen to hear more. Our opinion piece sets out clear proposals that are easily achievable by NHS England:
- A stronger learning foundation for patient experience work, with a qualification and professional development pathway. - Automatic access for PALS teams to the Patient Experience Library - the UK evidence base on patient experience.- Analytical tools to help staff make sense of the mass of patient survey data that arrives in different formats from different sources.- Acceptance by all Trusts that Heads of Patient Experience should be part of a patient-centred leadership culture.
This is the kind of professional recognition and support that clinicians take for granted. Patient experience staff deserve similar - especially in an NHS that says that "experience of care" matters.
Tuesday April 17th 2018
PALS vs robots
It is not easy to make sense of patient experience. Healthcare providers struggle to keep up with multiple datasets coming from CQC inspections, national patient surveys, Healthwatch reports, local compliments and complaints systems and more.
This paper makes the point that "enthusiasm for collecting patient experience data does not guarantee that these data will be used to monitor improvements and assure the quality of care". It goes on to say that "the eagerness for collecting [data] dissipates into confusion as busy staff struggle to transform reams of patient comments into useful information. The inevitable result is that, despite the best efforts of staff, information which patients share in good faith is wasted".
The task has, in recent years, been made even harder by the increasing tendency of patients to bypass formal feedback mechanisms and air their views via Twitter, Facebook and other social media. How are hard-pressed patient experience staff meant to keep up?
The authors consider the role of machine learning in helping providers to track large volumes of patient comments on social media and to "automate the laborious process of analysing the unstructured text".
They note that "The performance of machine learning algorithms is attractive". One system in particular can predict NHS Choices star ratings "with an admirable 97% accuracy".
So is it time to get rid of patient experience staff and use robots instead?
On this point, the authors are cautious. According to them, "Previous research has highlighted the disconnect between the collection of patient feedback, a relatively straightforward endeavour and its subsequent use to drive improvement activity" a far more elusive task".
In other words, computers can collate and sift data, but it takes skilled and experienced staff to work out what really matters, and to spot where the opportunities for service improvement lie.
As the authors themselves acknowledge, computational systems are good - they can excel at some tasks, and improve efficiency in some of the more laborious aspects of data handling. But the job of "distilling 'messy' patient data into clear and actionable insight" is - for the time being, at least - best left to humans.
Tuesday April 10th 2018
Patient Experience magazine - Spring 2018
Much of the discussion about patient experience centres on kindness and compassion. Sometimes, the talk is about dignity and respect. But how often do we think about the dynamics of power?
When the focus shifts from patient experience to patient and public involvement, we need to be especially conscious of the power balance between professionals and people who are sometimes described as "lay representatives". How are people invited to engage, and on what terms? On whose territory do meetings take place? Does professional expertise carry more weight than lived experience?
In the Spring edition of Patient Experience, we have two comment pieces that address these issues - raising questions, and offering pointers to good practice. Our third contributor describes her encounters with a health system that seems disjointed, unresponsive, even disrespectful. This creates another kind of power imbalance - one that makes a nonsense of aspirational statements in strategy documents.
We also have our usual roundup of recent reports on patient experience and patient/public involvement, including a batch that offer further evidence that the way healthcare staff are treated affects the way that patients are treated. As the NHS finalises its workforce strategy, this is vital evidence that must be taken into account.
We're always keen to hear from our readers, so if you have news and views for our next edition, get in touch!
Tuesday March 27th 2018
Staffing and patient experience - more evidence
The NHS consultation on the draft workforce strategy has now closed. A final version of the strategy will be published in July. Throughout the consultation period, we have been flagging up the connections between NHS staff experience and patient experience.
Now yet another report, this time from the Parliamentary and Health Service Ombudsman, reinforces the point.
The PHSO's job is to pick up complaints that have not been resolved by the NHS. And sure enough, the report highlights a series of such complaints, arising from serious failings in NHS mental health services. But it also considers how and why mistakes might be made in the care of people with mental illness.
A frank assessment of "The state of mental health provision in the 21st century" pulls no punches. It refers to recent CQC findings of:
- unsafe staffing levels
- staff on acute wards lacking the skills to anticipate and de-escalate violent situations
- information about risk not being available to all staff involved in a patient's care
It goes on to mention a King's Fund report which revealed "a 13% reduction in mental health nurses between 2009 and 2017, with inpatient care losing nearly 25%. Almost 10% of all posts in specialist mental health services in England are vacant."
The effect on patient experience can be seen in the complaints case studies that form the main part of the report. But the PHSO is in no doubt that "workforce challenges" are at the heart of the problem.
"The complaints we have included in this report demonstrate how patient care and safety is jeopardised by these workforce challenges. They show clinical staff ill-equipped with the skills to manage potentially violent situations, being expected to work double shifts leading to exhaustion, and clinicians having to treat conditions they have no experience of. Unless these workforce challenges are addressed it is difficult to see how the transformation of mental health care, envisioned in the Five Year Forward View for Mental Health, can be realised."
This is now the fourth consecutive report to make the links between staff experience and patient experience very clear indeed. As the workforce strategy moves from draft to completion, we hope that senior NHS managers will take note.
Tuesday March 20th 2018
Patient surveys: Read the small print
A common feature of patient surveys is some form of ratings system to indicate levels of satisfaction. Patients may be asked to give one to five stars for aspects of the service they have experienced, or to score from 1 ("Very Poor") to 10 ("Excellent").
Patient experience staff assessing the results will of course be delighted to see a sheet with top scores against all the survey questions. But this study, published in the Patient Experience Journal, suggests that the top scoring responses may merit a closer look.
The authors analysed almost two years of in-patient survey data from a large hospital system in the US, and found, puzzlingly, that "a significant percentage of patients provide perfect domain scores only to follow up with negative comments". They wanted to investigate this apparent contradiction and to "understand what patients who provide positive experience scores and negative comments are trying to tell the health care organization".
One finding was that patients sometimes use free text comment boxes on a survey form to raise issues that are not addressed by the actual survey questions. In one example, the survey asked about matters such as controlling pain or meeting emotional needs. But the patients, via their free text comments wanted to raise issues such as support staff and understanding of medications.
A second consideration is that "patients who are highly loyal to an organization may not want to decrease their ratings, based on an understanding that ratings are important to the organization". Giving high ratings while airing problems via the comment boxes may enable patients to express loyalty to the organisation, while simultaneously (and as a kind of quiet aside) suggesting room for improvement.
A further point is that "a patient may see a health domain as being predominantly great, but spoiled by 'one bad apple'". For example, a survey question on "nurses" in general may be rated as excellent, while the comment box reveals a problem with one nurse in particular.
The study contains plenty more interesting detail. But its overall message seems to be that if that if you get a five star survey response, don't rest on your laurels. For real learning, read the small print.
Tuesday March 6th 2018
Care for staff equals care for patients
Twice in the last couple of months, we have featured reports which show that workforce pressures on NHS staff generally result in poorer experience of care for patients. Those reports (here and here) focussed mainly on staffing levels and workload.
This new report takes evidence from NHS staff experience surveys and considers the extent to which staff experience (good or bad) can be a predictor of good or bad patient experience. It found that "there are some clear and strong associations between staff experience and how satisfied patients are".
As with the other reports, workload was important. "When the pressure is higher, and when staff are less satisfied with the resources and support available, patients clearly notice and have a less satisfactory experience."
However, the report goes beyond quantitative matters such as staffing levels, to look at more qualitative aspects of staff experience. It found that organisational culture matters: "In organisations where employees feel that there are not equal opportunities for career progression or promotion, or when staff experience discrimination, or when staff suffer physical violence at the hands of colleagues, patients are less happy."
The study found that for staff in general, "the ability... to contribute toward improvements at work was not as important". Except, that is, when it comes to black and minority ethnic staff. "...when BME staff thought their role makes a difference to patients, and when they were more able to contribute toward improvements at work, overall patient satisfaction was higher". The authors make the point that "the extent to which an organisation values its minority staff is a good barometer of how well patients are likely to feel cared for".
As the NHS and Public Health England consult on the draft workforce strategy, this series of reports present vital evidence that must be taken into account. They show that workforce issues are not just about staffing levels and skills: organisational culture matters too. They show that a "one size fits all" approach will not work - the NHS workforce, like wider society, comprises diverse groups with varying needs and expectations. And they show that in an NHS that aims to be person centred, the way staff are treated directly affects the way that patients are treated.
Tuesday February 27th 2018
Ignoring the alarms
This hard-hitting report from the Parliamentary and Health Service Ombudsman is a must-read for anyone involved in patient experience work and complaints management.
We hear of the needless death of a patient - Averil Hart, who died of anorexia nervosa, aged 19. The PHSO report details "multiple serious departures from the standards of care expected", and "a long series of missed opportunities to recognise her deteriorating condition".
As in so many other cases, what happened next was that grieving relatives suffered the worst possible treatment at the hands of NHS organisations.
The PHSO examined the experience of Mr. Hart (Averil's father) through a prolonged period of enquiry and complaint. They found that "most of the NHS organisations which dealt with Mr Hart's complaint failed to respond to his concerns in a sensitive, transparent and helpful way".
Responses to requests for information "were delayed and appeared evasive, and information he requested was often not provided". Responses to complaints "were equally unsatisfactory, and often appeared defensive or protective of the organisation concerned". There was "a consistent picture of unhelpfulness, lack of transparency, individual defensiveness and organisational self-protection".
The report is entitled "How NHS eating disorder services are failing patients". But it is not just about eating disorder services. Multiple organisations and services were complicit in the poor treatment of the family following Averil's death.
The PHSO says this:
"The Cambridgeshire and Peterborough Trust's handling of Mr Hart's complaint was so poor that it was maladministration.""The GP practice's complaint handling was so poor that it was maladministration.""The Norwich Acute Trust's complaint handling was so poor that it was maladministration.""NHS England's approach... was so poor that it was maladministration."
The report finishes with this observation - and warning: "The death of Averil Hart was an avoidable tragedy. Every NHS organisation involved in her care missed significant opportunities to prevent the tragedy unfolding at every stage of her illness from August 2012 to her death on 15 December 2012. The subsequent responses to Averil's family were inadequate and served only to compound their distress. The NHS must learn from these events, for the sake of future patients."
Tuesday February 20th 2018
Better experience at end of life
We have often made the point that "patient experience" is not just about what happens to people who are unwell. It is also about how relatives and carers feel about the way that loved ones are being looked after. That is particularly true when it comes to end of life care.
As this new report from Macmillan puts it, "At a time when you are at the mercy of medicine, and of your own body, you can feel extremely disempowered and out of control. And, as a family member, you can feel that everything is happening to you and around you".
The report notes that in July 2016, the Government made a "National Commitment" to improve end of life care across England. This included making sure everyone has access to the right end of life care, regardless of geography, age, diagnosis, background or means.
But the commitment came with no extra funding. Instead, implementation of the commitment was left to local sustainability and transformation partnerships (STPs). Analysis of draft STP plans, however, has shown that 41% had no mention or little detail of how end of life care would be improved.
The report authors state that "there continues to be unacceptable geographic variation and inequality in the end of life care people with cancer receive in their dying months. While some people have choices around where they die, and the chance to spend time with the people who matter to them, others spend their final year in and out of A&E, and have little opportunity to access the care of their choosing".
They go on to say that "Each year in England, an estimated 48,000 people experience poor care in the final three months of their lives. And more than 12,500 cancer patients (10% of those who die in England each year) spend the last two days of their lives without adequate pain relief".
The report makes a series of recommendations for how variations in end of life care could be better identified and addressed. It calls for "genuine choice about how you are cared for and where you spend the last days and hours of your life" - not only for the sake of patients, but also because a good experience of end of life care can have "a lasting and meaningful impact on friends and family left behind".
Tuesday February 13th 2018
Workforce pressures worsen patient experience
A few weeks ago, we featured a BMJ paper, "Patient satisfaction with hospital care and nurses in England". The authors had found that 85% of nurses in NHS hospitals were unable to complete nursing tasks due to lack of time associated with high patient-to-nurse workloads.
7% of nurses reported that they lacked time to complete necessary pain management, and 11% missed treatments and procedures. That is bad enough. But when it came to the kind of person-centred care that is a defining feature of high quality services, the picture was far worse. A staggering 52% reported lacking the time to educate patients and their families, and two out of three (65%) were unable to comfort or talk with their patients.
Now a new report from the Kings Fund and Picker Institute confirms links between workforce pressures and patient experience. They found that on busy wards with high bed occupancy, patient feedback was more negative, particularly in respect of getting comprehensible answers from nurses; and timeliness of response to call buttons.
Conversely, patients at trusts with more nurses per bed reported a more positive experience.
Patient experience was also negatively associated with higher spend on agency staff. This, according to the report authors, is unsurprising, since "use of agency staff provides less continuity of care and stability for hospitals and patients". They comment that "The main focus of concern for spend on agency staff has been on financial savings; our analysis suggests that there are quality issues at stake as well".
The report states that "work pressures and staff shortages in the NHS are escalating, and likely to worsen given financial constraints and the probable impact of UK's withdrawal from the EU". In these circumstances, say the authors, "the risks to patient care are self-evident and it is important to monitor staff wellbeing and how it is impacting on patients".
Monday February 5th 2018
More deaths. More learning.
Last week saw the publication of a long-awaited report into the deaths of five children in the care of health services in Northern Ireland. The children died in the late 1990's and early 2000's, and bereaved families have had to wait until now for a full and final account of what happened.
There are two common threads running through the families' experiences. The first is that their children died from hyponatraemia - an excessive dilution of sodium levels in the blood. According to the Inquiry report, this is a condition for which "A diagnosis is made easily". It goes on to say that "dilutional hyponatraemia should not happen in a hospital. It is a preventable hospital illness".
The second common thread is institutional denial of error, and appalling treatment of grieving relatives.
The Inquiry report describes "an underlying institutionalised reluctance to admit major shortcomings" and "no acknowledgement of any of the very many failings in care". There was "defensiveness, deceit and a strong inclination... to close ranks". Furthermore, "clinicians did not admit to error for the obvious reasons of self-protection" this defensiveness amounted to concealment and deceit".
These statements are a clear, and dismaying, echo of similar statements in inquiry reports from Mid Staffs, Morecambe Bay and Southern Health. The "Recommendations" section of the report starts by saying that "The lessons of these sad cases must be learnt because it cannot be assumed that such tragedy could not happen again". The Morecambe Bay investigation report carried an almost identical warning: "It is vital that the lessons, now plain to see, are learnt... by other Trusts, which must not believe that "it could not happen here'".
Mistakes can and do happen. There will be further avoidable deaths in NHS services. When they occur, the learning should not just be about improved practice and procedures. It should also be about how the NHS, as a healing organisation, learns to deal honestly and compassionately with bereaved relatives.
Tuesday January 30th 2018
Got questions? Get this.
You might think that writing questionnaires is a fairly basic skill for people involved in patient experience work. At the same time, we have probably all had experiences with questionnaires that were too long, or contained overcomplicated or irrelevant questions.
Writing a good questionnaire is harder than it seems, which is why this guide from NHS England is a welcome new addition to their "Bite-Size" series.
There won't be much in it to trouble academic researchers. But it will be handy for any front line practitioners needing to put together a questionnaire while simultaneously handling complaints, writing committee reports, managing volunteers and keeping the boss happy.
Some of the advice may seem basic - for example "avoid using jargon". But as it progresses, the guide takes us into more interesting territory, covering "cognitive testing", "gratitude bias" and "bipolar" versus "unipolar" scales. That may sound as though the authors ignored their own advice to avoid using jargon. But the terms are explained well, within a publication that - as with all Bite Size guides - is clear and concise.
If you need a questionnaire that patients can make sense of, and which will return a set of results that you can make sense of, this is the document to have ready to hand.
Tuesday January 23rd 2018
Defining patient/public involvement. Should we even try?
Patient and public involvement (PPI) can, at times, look like motherhood and apple pie. We can all agree that it is, by and large, a Good Thing.
Agreeing what we mean by PPI, however, can be harder. We have touched on this issue previously - the excellent "Zombies and Unicorns" paper, for example, stated that "there is a lack of consensus about what effective PPI in research processes might look like and... little conclusive evidence about the best (or worst) ways to invoke PPI in research design, research practice, or research commissioning".
This paper agrees, pointing to "a lack of a common language to share PPI practice... the term PPI is not universal in its application or definition".
In spite of this, attempts to nail down a definition of PPI may not be helpful. They can lead to "semantic intricacies" and "circular debates held primarily amongst academics".
But if we cannot agree a definition of patient and public involvement, how can we aim for consistently good practice? For the authors of this paper, the answer is to aim instead for a basic set of principles - clear enough to be commonly understood, but flexible enough to be applied across different PPI settings.
The paper goes into some detail about the research method, but the important outcome is a set of "essential" and "desirable" PPI principles, assembled from the viewpoints of both patients and professionals.
Equally important is that "the principles suggested provide quality guidelines for best practice, not prescriptive rules. The proposal of a "one size fits all" approach to PPI would be inappropriate, as no single PPI initiative will work for all situations, individuals or agendas". And "whilst PPI must be adaptable to local circumstances and objectives, the essential principles required to underpin its effectiveness may well be universal in their application".
Tuesday January 16th 2018
NHS nurses - uncaring, or just too busy?
85% of nurses in NHS hospitals report not being able to complete nursing tasks due to lack of time associated with high patient-to-nurse workloads. So says this study, recently published in BMJ Open.
The authors state that "when nurses have high patient loads... necessary nursing care can be missed because of lack of time". That may come as no surprise. Intriguingly, though, the study goes on to look at the kinds of tasks that are missed when the pressure is on. And it presents clear evidence that while some clinical care may suffer, what really gets hit is the kind of person-centred care that is meant to be the bedrock of good patient experience.
7% of nurses reported that they lacked time to complete necessary pain management, and 11% missed treatments and procedures. But a staggering 52% reported lacking the time to educate patients and their families, and two out of three (65%) were unable to comfort or talk with their patients.
The study cites Sir Robert Francis, Chair of the public inquiry into the Mid Staffordshire NHS Trust, as stating (July 2017) that safe nurse staffing in England still lacks a standardised approach. It confirms his view, with the finding that there is "substantial variation across NHS general acute hospitals in patient-to-nurse workloads. Nurses in some NHS hospitals are caring for twice as many patients at a time as nurses in other hospitals".
This matters because of what the authors describe as "The concern about nurses being uncaring or lacking in compassion". Their view is that the study "refutes the narrative blaming quality of care deficits in NHS hospitals on uncaring nurses".
On this evidence, it would appear that the problem is not so much a lack of compassion as a basic lack of nurses.
Tuesday January 9th 2018
Patient Experience magazine - Winter 2018
We kick off 2018 with the latest edition of our Patient Experience magazine, featuring another great batch of topics and insights from the world of patient experience and involvement.
On "experience", we have a story about stolen biscuits. This is a useful reminder that sometimes it's the small kindnesses that count, and that organisational attitudes are revealed not in the grand vision statements, but in day-to-day actions.
On "involvement", we have a discussion of "virtue signalling", whereby moral posturing may be seen as more important than effective engagement. An item on culturally sensitive approaches to antenatal classes covers both angles, showing how well-handled involvement can lead directly to improved patient experience.
Our collection of reports and studies contains some gems. The Care Quality Commission published three national patient surveys during the autumn, on Emergency Departments, Community Mental Health Services and Children and Young People's experiences. All provided useful insights in their respective areas. But putting all three together alongside the May 2017 Adult Inpatient survey revealed a stark fact - that people with mental health conditions have consistently poorer patient experience across the board. As the new Mental Health Policy Research Unit gets up and running, we hope that the CQC's findings will be central to their agenda.
Tuesday December 19th 2017
Need information? Ask a nine year old.
"Communication" features regularly as an issue in patient experience surveys and focus groups. People struggle to understand and retain complex information on health conditions, medication, appointments and so on.
The standard response is to produce leaflets that summarise key facts and can be handed out to patients. But do such leaflets help? What do we do about the fact that, with a UK average reading age of 9 years, much written material will be beyond the grasp of many readers?
The authors of this BMJ paper took a novel approach. They went to a group of nine year olds, taught them about total hip athroplasty, and then asked them to write a patient information leaflet on the subject.
The results are both hilarious and revealing. The children weren't interested in dressing up their messages in official language, or in observing social niceties. They just went straight to the point. "Your hip is old and rotten" was Mohammed's opener. In case you hadn't got that, Jamie helpfully explained, "It is past its sell-by date".
Outlining the procedure, Oliver wrote that, "we saw out the old bone... put the new one in and it's a new hip and then we clip it back up". David's reassurance is, "...don't worry you will be asleep. When you wake up it will all be done".
How about preparation for the op? Maria's advice is, "Don't smoke. Lose weight. Be there on time!!"
The children drew pictures to illustrate key points. Our favourite is the one that carries an important piece of advice for all patients: bring your teddy with you.
People writing patient experience leaflets may not want to adopt all of the children's approaches. Explaining the risks, for example, Mohammed may have been a little too blunt ("You might die!!!!!!"). But in with all the fun is an important point about keeping it simple and saying what you mean.
As the authors put it, "Enlisting children to help formulate these leaflets may seem whimsical. But our experience has shown us that the child can become the tutor, teaching us the value in simple relevant communication."
Tuesday December 12th 2017
Healthwatch funding cut. Again.
Last week, Healthwatch England took the step of publishing a letter to the Secretary of State for Health, along with a briefing about the state of funding for the local Healthwatch network.
The documents describe a 37% reduction in funding since the network's first allocation in 2013/14. They say that this is "putting at risk the ability of the network to deliver on its statutory obligations".
By way of evidence, they state that:
- Local Healthwatch operate on very tight budgets and with very small staff teams (often only two people) covering very large geographical areas and populations.
- There are problems with one or two year contracts not providing sufficient stability to enable long term planning and retain staff.- There are concerns around some councils' confusion between commissioning statutory Healthwatch activity and funding wider voluntary and community sector projects.
Healthwatch was set up in the wake of the Francis Inquiry into "appalling suffering" and avoidable deaths at the Mid Staffordshire Trust. It was meant to be a stronger and more effective patient voice organisation than its predecessor, the Local Involvement Network. But it is hard to see how it can fulfil that expectation with the financial rug being pulled each and every year since its inception.
Last year, our report "What Price Patient Voice" described a widespread failure to understand the value for money offered by Healthwatch and other patient voice initiatives. There is no consensus on what value for money looks like, and no benchmarking of funding levels for patient voice work. This would not be acceptable within other health service functions such as medicines or workforce, where financial assessments, value for money scrutiny and investment rationales are the norm.
Without a clear value proposition, Healthwatch will struggle to develop a strong business case. That makes the network vulnerable to further funding cuts.
It also means that local authorities are free to do what they want with funding that is intended for the statutory functions of local Healthwatch. They can cut as deep as they like. They can do so arbitrarily. And they can get away with it.
Tuesday December 5th 2017
Patient experience worse for mentally ill
For the fourth time this year, a national patient experience survey has shown that people with mental health conditions have a poorer than usual experience as patients.
The Care Quality Commission's Children and Young People's Survey has found that patients with a mental health condition, and their parents and carers, reported significantly worse experience for matters including information and communication, transition and continuity, respect for patient-centred values, involvement of family and friends, and awareness of medical history.
The Children and Young People's Survey follows on from the Adult Inpatient Survey and Emergency Dept Survey, which both revealed poorer experiences of care for people with mental illness. A fourth study - the Community Mental Health Survey - reported little sign of improvement for "substantial concerns" raised a year ago, and stated that services "have even declined slightly in key areas".
The latest findings make a nonsense of Prime Minister Theresa May's claim that mental illness is a "hidden injustice". Unjust it might be. But hidden it certainly is not. Four national surveys in a row have shown that people with mental health conditions - children as well as adults - have consistently poorer experiences of care right across the board. The evidence could not be clearer.
The CQC has done an excellent job in bringing this issue to light. It is time now for politicians and providers to act.
Tuesday November 28th 2017
Making Sense of Patient Experience
Two years after its publication, it is worth revisiting "Making Sense and Making Use of Patient Experience Data".
The report sheds light on the hard realities of patient experience work at the front line. It makes the point that patient experience staff work in small teams with limited resources.
Particular challenges include gathering an ever-increasing amount of data, keeping up with reporting requirements and ad-hoc requests, and having the time and capability to analyse data and generate insights.
One patient experience lead put it like this, "It's a nightmare to see what's going on. Trying to triangulate between 12 different data sources coming from different angles, presented differently.. " Another was somewhat more succinct: "It's mad. We need to rationalise what we ask".
The result, according to the report's authors, is that: "Staff and patient experience teams are sometimes so busy gathering data and compiling reports, that less time is available to do something with the data - efforts to improve services are in danger of being squeezed out".
Two years on from the report's publication, patient experience evidence is still published in too many different places and in too many different formats. But we have made a start on rationalising it.
We have collated and catalogued all the UK patient experience literature, so that it is now searchable. Our Knowledge Maps series has also had a good response, with people commenting on the value of having lots of key data all in one place. But we see a need to go further.
We are starting to envisage a way of simplifying the task of "gathering data and compiling reports". Discussions with staff in Trusts and CCGs indicate a clear need, and are also indicating some possible solutions. So we're limbering up for some more breakthroughs in the year ahead.
Watch this space to see how we're getting on - or better still, drop us a line if you want to contribute ideas or get involved: info@patientlibrary.net
Tuesday November 21st 2017
CQC shines light on "hidden injustice"
A year ago, when the 2016 survey of patient experience in community mental health services was published, the Care Quality Commission said that "substantial concerns remain about the quality of care some people using community mental health services receive. There has been no notable improvement in survey results in the last year".
They suggested that there was "scope for further improvements in a number of areas including: involvement in care, crisis care, care planning and reviews".
Worryingly, the 2017 survey results, just published, show little sign of improvement. In fact, the CQC's own headline is that "patients' experiences of these services across England have not improved and have even declined slightly in key areas".
The survey shows that:
- 26% of respondents said that they did not feel they got the help they needed from crisis care, compared to 21% in 2014.
- 25% of respondents reported they had not seen workers from their mental health services often enough to meet their needs in the last year - up from 21% in 2014.
- 68% of respondents felt listened to by their healthcare or social workers - down from 73% in 2014.
Especially troubling is "a marked trend that the longer a person is in contact with mental health services, the worse the experience reported".
Nearly a year ago, Prime Minister Theresa May described mental illness as a "hidden injustice". Various statements since then have been taken by some as encouraging signs that government - at the highest level - takes mental illness seriously, and that parity of esteem with physical health services is on its way.
But feedback from patients is clearly and consistently telling a different story. And those injustices are not hidden. They're right there in the CQC's evidence.
Tuesday November 14th 2017
Patient Experience in Trusts - the new map
For too long, the data on patient experience in NHS Trusts has been too hard to find.
A large volume of evidence emerges from surveys and feedback mechanisms. But it is published across multiple websites, and hundreds of individual web pages. Health professionals can struggle to find what they need. Members of the public (the source of all the data) may not even know where to begin.
In a major breakthrough for patient experience reporting, we have brought all the key Trust data together into one simple to use map. This is a huge increase in the accessibility of patient experience data. It strengthens Trusts' transparency and public accountability. And it helps the NHS on its journey towards providing information digitally and seamlessly.
The map is part of our continuing mission to bring patient experience into the light.
The map will make life easier for policymakers, commissioners and providers. It also makes the information far more accessible to members of the public, who fund and use NHS services, and who give time and goodwill to make their experiences known.
We'd like to say a big thank you to all the people from Trusts and CCGs (you know who you are!) who helped us with the concept and design, and then tested various versions.
The "Patient Experience in Trusts" map is available on the Patient Experience Library website, along with other Knowledge Maps that help to make important sources of evidence more visible.
Tuesday November 7th 2017
Patient experience: Lessons from Hillsborough
It was good to see NHS England hosting two "Learning from Deaths" events last week - one for bereaved families and one for health professionals.
The events were part of efforts to ensure that the recommendations contained in the CQC's "Learning, candour and accountability" report are implemented in a clear and structured way.
By a remarkable coincidence, last week also saw the publication of a report by Bishop James Jones, which aims to "ensure the pain and suffering of the Hillsborough families is not repeated".
Entitled "The Patronising Disposition of Unaccountable Power", the report reveals striking parallels between the experiences of the Hillsborough families and of people who have sought justice following avoidable deaths within health and care services.
The Bishop remarks that "The [Hillsborough] families know that there are others who have found that when in all innocence and with a good conscience they have asked questions of those in authority on behalf of those they love the institution has closed ranks, refused to disclose information, used public money to defend its interests and acted in a way that was both intimidating and oppressive".
Institutional reactions of this kind have been documented in the Francis report on Mid Staffs, the Kirkup report on Morecambe Bay and the Mazars report on Southern Health.
NHS staff do a fantastic job under immensely difficult conditions. Day after day, they care for people, cure sickness and save lives. On the rare occasions when things go wrong, a poorly handled institutional response can let down staff, as well as patients.
The Bishop observes that a lack of honesty does not come from individuals - it is institutionally embedded. It is "a cultural condition... an instinctive prioritisation of the reputation of an organisation over the citizen's right to expect people to be held to account".
The report urges the Prime Minister and Home Secretary to "ensure that those responsible for our national institutions listen to what the experiences of the Hillsborough families say about how they should conduct themselves when faced by families bereaved by public tragedy".
Mid Staffs, Morecambe Bay and Southern Health are public tragedies where too many avoidable deaths were followed up by inadequate investigations and dismissive treatment of bereaved families. Shrewsbury and Telford is likely to fall into the same category.
We hope that those responsible for the NHS Learning from Deaths programme will take careful note of the contents of this report.
Tuesday October 31st 2017
CQC vs Twitter: which is better?
The likelihood of patient feedback being dismissed as merely "anecdotal" is, thankfully, diminishing. Healthcare professionals know that patients can offer useful insights into quality and effectiveness - picking up issues that they themselves might miss.
Now a new study lends added weight to the idea that patient feedback is not just an optional extra, but a key part of performance and risk management within the NHS.
"Wisdom of patients" describes a project carried out by specialists in risk analysis and behavioural science. They took large volumes of patient feedback on Trusts and hospitals, from sources including Twitter, Facebook and Care Opinion. They then applied classifications and sentiment analysis to produce a "collective judgement score", or CJS. Finally, they compared the CJS with CQC inspection ratings for the services in question.
They found that on average, patient feedback ahead of a CQC inspection is better for hospitals that subsequently get a higher CQC rating. The better the patient feedback in the 90 days prior to a CQC inspection, the greater the likelihood of a more positive overall rating.
Interestingly, some 'Inadequate' hospitals scored a high collective judgement score (from the social media feedback), as did some 'Requires improvement' hospitals. So it would appear that patients are better collective judges of organisations performing well than they are of organisations performing poorly.
In spite of this, the researchers state that "while the collated patient feedback cannot perfectly identify poorly performing organisations, it can identify those organisations that are most likely to be performing poorly. Indeed, not a single organisation with a [low] CJS was rated 'Good' or 'Outstanding'.
So is patient feedback via social media a better guide to service quality than a CQC inspection? Probably not - or at least, not yet. The authors of this paper are clear that "there is still a lot to be learnt about the use of aggregated patient feedback. It is possible that the predictive power ...could be improved".
Even so, there is already "a positive association between the collective judgement score and subsequent inspection outcomes". And the paper concludes that "The near real-time, automated collection and aggregation of multiple sources of patient feedback should be used to help prioritise inspections".
Be warned - if you're not a statistician, this paper may not be an easy read. But if you persevere, you may find yourself thinking twice about how you use your social media feedback.
Tuesday October 24th 2017
A&E - what do patients think?
We hear a lot about the pressures that A&E services are under, including many reports that patients misuse the service by turning up there as a first, rather than last, resort.
The CQC's 2016 Emergency Department survey (released last week) shed interesting light on this issue. 42% of respondents did not go to A&E as their first port of call - they used alternatives such as GPs, or the 111 and 999 numbers. But three-quarters ended up in A&E anyway because they were referred there by those other services.
There may well be misuse of A&E by some people. But it may not be as widespread as some sources would have us believe.
Many patients - once there - have a very favourable experience of the service. There are high levels of confidence in clinicians, and a significant majority feel listened to and respected (78%). Even more (82%) had enough privacy while being examined or treated.
On the downside, fewer than half of those who were distressed felt that staff "definitely" reassured them. And nearly half (45%) reported being discharged without any account being taken of their family or home situation. This ties in with various Healthwatch reports (local and national) about problems with leaving hospital.
A further correlation is for people experiencing mental ill health. Their experience of A&E is poorer than for other patients, tying in with findings from the 2016 acute inpatient survey.
Tuesday October 17th 2017
Patient experience as a lever for funding... and for evidence based commissioning, and more!
The autumn 2017 edition of Patient Experience is out now, with news, views and research updates on patient experience and patient/public involvement in healthcare.
The journal features comment from a former Head of Fundraising at a major hospital charity, who explains how patient experience can be used to focus funding on the "additional extras" that can do so much to improve people's hospital visits.
Further comment comes from a senior researcher who looks at evidence-based commissioning, and considers how "knowledge mobilisation" can help commissioners put academic writings to practical use.
We have all our usual reviews of the latest patient experience studies and surveys - helping you to keep track of the resources that can guide your policy and practice. And we offer pointers to training and conference events - some supporting professional development, and some open to patient representatives as well.
We hope you'll enjoy this edition of Patient Experience and if you have ideas for other great content we should be featuring - let us know! info@patientlibrary.net
Tuesday October 3rd 2017
Harm to healing - partnership with patients
As NHS England limbers up for its "Learning from deaths" guidance development day, we thought it might be worth digging out "Harm to Healing", a 2011 report from the Canadian Patient Safety Institute.
This valuable report looks at the engagement and partnering of patients and/or their families who have been harmed in healthcare, and considers psychological aspects of recovery.
The authors find that "patients/families who have been harmed in healthcare grieve in a way that is similar to, but distinct from other forms of loss" (our underline). Importantly, they state that "Healthcare providers and leaders in healthcare organizations may also go through a grieving process similar to what patients/families experience".
They describe a "second harm", experienced by patients/family when "the healthcare organization does not provide information with a reasonable explanation about the original harm in an open, timely and respectful manner". This matters, given the CQC's recent statement (in "Learning, Candour and Accountability") that "we have heard from families who had to go to great lengths themselves to get answers..., who had their experiences denied and their motives questioned".
The report makes it clear that the process of engaging patients and relatives in investigation and remedial work is far from straightforward. "Patients/families engaged too early in their recovery journey may unintentionally suffer further harm". Health professionals need to understand that "there is a difference between eagerness [to be involved] and readiness ... eagerness can overwhelm the readiness".
We welcome the work currently being undertaken on "learning from deaths", but hope that it will not limit itself to simply reviewing systems and procedures. The NHS, as a healing organisation, also needs to look after the emotional wellbeing of patients, relatives and staff who are dealing with trauma and grief.
Tuesday September 19th 2017
Patients, professionals, power and culture
Last week, we looked at "hostage bargaining syndrome" - the propensity of vulnerable patients to deal with powerful and expert clinicians as if negotiating for their health from a position of fear and confusion.
This week's featured report looks at the position of health professionals, and considers how they react to more assertive patients - the ones who are (or are perceived to be) complaining.
Interviews with 41 staff in eight different NHS settings explored how they made sense of complaints and of patients' (including families') motives for complaining.
The authors found that complaints were seen as a breach in fundamental relationships involving patients' trust or recognition of professionals' work efforts. Complaints were most often regarded as coming from patients who were inexpert, distressed or advantage-seeking. Accordingly, care professionals positioned themselves as informed decision-makers, empathic listeners or service gate-keepers.
Troublingly, the authors note that it was rare for interviewees to describe complaints raised by patients as grounds for improving the quality of care.
Taken together, both last week's and this week's featured reports indicate that there is much more to "patient voice" than surveys and "engagement activities". Patients feeling vulnerable and powerless may be too frightened to say anything much. Those who do speak up may be seen by health professionals as troublesome.
Understanding patient experience is not just about feedback systems and action plans. It is also about power relationships and organisational culture.
Tuesday September 12th 2017
Patient? Or hostage?
There is much talk in the NHS these days of "person-centred care", and of patients and clinicians being "partners in care". The aim is to move on from the old "doctor knows best" attitude, and to encourage "empowered patients" to participate in decision-making.
Of course, culture change is often easier said than done, and this paper from America's Mayo Clinic describes how some patients can succumb to "hostage bargaining syndrome" (HBS), whereby they behave as if negotiating for their health from a position of fear and confusion.
The paper observes that medical care has recently become more focused on serving patients as consumers. But most commercial services are "want" services, while medical care is a "need" service that consumers-turned-patients often dread and may delay receiving.
Patients are often reluctant to assert their interests in the presence of clinicians, whom they see as experts. The higher the stakes of a health decision, the more entrenched the socially sanctioned roles of patient and clinician can become. HBS is especially seen when serious illness unfolds over the course of multiple, complex, emotionally laden interactions with clinicians. Cancer care and intensive care, for example, are characterised by a high degree of dependence and powerlessness for patients.
HBS can manifest as understating a concern, asking for less than what is desired or needed, or even remaining silent against one's better judgment. When HBS persists and escalates, a patient may succumb to learned helplessness, making his or her authentic involvement in shared decision making almost impossible.
The authors conclude that clinicians often have the power to arrest and reverse HBS by appreciating, paradoxically, how patients' perceptions of their power as experts play a central role in the care they provide.
This is a thought-provoking document that is well worth a read.
Tuesday August 29th 2017
Patient Experience in England
NHS strategies state that an understanding of patient experience is central to development of "person-centred" services. But our latest publication reveals that NHS staff are bombarded by eighteen separate reporting mechanisms on patient experience. Data arrives in different formats and at different times, and some of it is of questionable quality.
The report, "Patient Experience in England", cuts through the muddle, explaining how patient experience evidence is gathered and disseminated. It shows what has been learnt about patient experience in England over the last year. And importantly, it looks at whether health service providers are acting on the learning.
Good news from the last year includes generally positive experiences for cancer patients, and a sense among hospital inpatients that confidence and trust in clinical staff has gone up. However, other findings strike a warning note:
- There are "significant declines" in key areas of person-centred care.
- "Substantial concerns" remain about the quality of care some people using community mental health services receive.
- In maternity services, some women were left alone at a time that worried them during early labour, and of those who raised concerns, not all felt that their concerns were taken seriously.
The report goes on to list recent research studies that have shown an "evidence-practice gap", with Trusts, CCGs and GPs all having difficulty in translating patient experience evidence into better service delivery.
Part of the problem is that patient experience leads lack parity with clinicians in terms of their professional development and support. If they are to lead Trusts and CCGs in understanding patient experience, they need better access to the literature. We are providing a solution in the form of the Patient Experience Library, and are calling on NHS England to work with us to open up access to the Library as widely as possible.
Tuesday August 22nd 2017
Improving patient experience in primary care
A few weeks ago, we reported on the 2017 GP Patient Survey results. Our comments briefly touched on this observation, from "Improving patient experience in primary care": "...surveys are a valuable resource for monitoring national trends in quality of care [but] may be insufficient in themselves to fully capture patient feedback, and in practice GPs rarely used the results of surveys for quality improvement."
We're returning to "Improving patient experience..." to recommend a read of the report. Be warned - at some 450 pages, it's a long read. There is, however, an excellent summary offering some thought provoking findings, including these:
- Patients are reluctant to be critical when completing feedback questionnaires. Reasons included the need to maintain a relationship with the GP, gratitude for NHS care, and power asymmetries. Patients find questionnaires to be limited tools for feeding back concerns about consultations.
- Ethnic origins of patients have a bearing on patient experience. Low scores given by Pakistani patients in surveys such as the GP Patient Survey reflect care that is genuinely worse, and possibly much worse, than that experienced by their white British counterparts.
- GPs are positive about the concept of patient feedback, but struggle to engage with [it] and make changes under current approaches to measurement.
- Within practices, and in out-of-hours settings, staff neither believed nor trusted patient surveys. Concerns were expressed about their validity and reliability, and the likely representativeness of respondents.
The authors conclude that there is "a huge gap" between the measurement of patient experience, and the actions being taken as a result. Importantly, they state that "the major question for the future is how we are going to take the wealth of data on patient experience and make experiences better, rather than simply better understood".
It is impossible, in this short review, to do justice to such a wide-ranging and in-depth study. We recommend a read of the report.
Tuesday August 15th 2017
Self-management: More harm than good?
With increasing demand for health services, propelled by an ageing population, and long-term conditions such as diabetes, it is no surprise to see NHS strategies placing more and more emphasis on "self-management". Often this is couched in the language of "shared-decision-making" and patient empowerment" - on the face of it, desirable goals.
This short and snappy presentation, however, raises important questions about patients' ability to manage elements of their own care. It considers social and cultural determinants of health, and makes the point that "A background of historical oppression or social inequity will not make the [process] a collaboration but may reinforce pre-existing negative determinants of health".
The extent to which self-management burdens the patient, rather than empowering him/her also depends on the balance between care needs and the patient's own ability to fulfil them. "Patients with few demands but low capacity may experience burden whereas those with many demands but high capacity may not".
The presentation comes from Canada's "Measuring Patient Centred-Care Forum" and to some extent reflects the Canadian context. But the overall message is relevant to UK audiences as well: self-management may be an important part of NHS strategy, but we should not take its apparent benefits for granted.
Tuesday August 8th 2017
We can't be patient-centred if we don't know what it means
The NHS wants to be patient-centred. We know this because the phrases "patient-centred" and "person-centred" appear repeatedly in NHS vision statements, mission statements and strategies.
But what does "person-centred care" actually mean? Unfortunately no-one seems to know.
There are various definitions floating around, but no agreement on which one is best. So we have an NHS that is setting a course towards something that hasn't been clearly defined.
That's like setting sail for America when you don't really know where America is. With lots of luck and a fair wind, you might just get there. But it's more likely that you'll go round in circles getting ever more confused.
A recent editorial piece from the Journal of Clinical Nursing makes some powerful points about why this matters.
Firstly, in the absence of clarity and rigour, there is a tendency to simplify. A favourite idea is that "person-centredness is working with what matters to the patient; it is about acknowledging the values, choices and preferences of patients, and it is about a certain type of nurse-patient relationship - always a compassionate one!" But this kind of over-simplification misses the point that "facilitating choices and... sustaining a compassionate relationship are probably the most challenging aspects of nursing".
Another concern is that practitioners "generally experience working in contexts and cultures that are inherently unsupportive of person-centredness, meaning they cannot embody or practice in person-centred ways". This view will be familiar to anyone who has read the research indicating that in order to look after the patients, you have to look after the staff.
The authors go on to consider measurement of person-centredness. "A fundamental principle of any systematic evaluation is clarity of definition... Given that we observe few clear definitions in use, then how can organisations evaluate person-centredness?"
The conclusion is that "publishing incomplete and poorly considered definitions of person-centredness promotes the view that person-centredness is less complex than it is and that it is easier to implement than it is. This can lead to unnecessary burden or even guilt for many in our profession as to why we are not achieving it better than we do or even a collective false consciousness that we have already achieved it and should be moving on to the next fad or miracle improvement/innovation".
This succinct and well-argued article nails an issue that lies at the (confused) heart of current NHS thinking.
Tuesday August 1st 2017
Publishing patient experience data does not make it transparent
"transparency - the free, uninhibited flow of information that is open to the scrutiny of others-has been far more positive than many had anticipated, and the harms of transparency have been far fewer than many had feared. Yet important obstacles to transparency remain..."
A useful report from the American Lucian Leape Institute looks at various kinds of transparency - for example among clinicians (peer review) and between healthcare organisations (collaborative approaches). But the recommendations that most interested us were those focusing on transparency of both clinicians and organisations with the public.
Two recommendations in particular jumped out:
- "Provide patients with reliable information in a form that is useful to them."
- "Present data from the perspective and needs of patients and families."
Here in England, we spend huge amounts of time and money gathering and analysing patient feedback. The results are published - but not always in ways that aid transparency.
National patient surveys produce complex statistical data, disseminated via multiple spreadsheets. Qualitative evidence from other sources is written up in reports that use complex language across dozens of pages. Even professionals find it hard to understand some of this stuff, never mind the general public.
Worse still, the published data - both quantitative and qualitative - is scattered across hundreds of different websites. Before you can read the data, you first have to find it - and that in itself is a tough challenge. We know, because we spend every day of the week tracking down material for the Patient Experience Library.
We are determined to bring patient experience into the light. An important first step has been the creation of the Library - the first ever comprehensive database of patient experience evidence. We have started to build on that with Knowledge Maps and Insight Reports that make the evidence more visible and understandable. We have further developments in the pipeline that will continue to bridge the gap between clinicians and healthcare organisations, and the general public.
Transparency, in respect of patient experience, does not mean simply gathering and publishing data. It means "providing patients with reliable information in a form that is useful to them". We are committed to doing exactly that.
Tuesday July 25th 2017
Safe staffing in maternity services
In March 2015, the Kirkup inquiry into unnecessary deaths in the maternity unit at the Morecambe Bay NHS Trust published its findings. In an uncomfortable echo of the Francis Inquiry into deaths at the Mid Staffordshire NHS Trust, Kirkup found that failure to hear from patients was an underlying cause of repeated errors. "The treatment of complainants... exemplified the problems commonly reported, including defensive 'closed' responses, delayed replies, and provision of information that complainants did not find to be accurate".
In April 2017 the Secretary of State for Health ordered an investigation into deaths in the maternity unit at the Shrewsbury and Telford Hospital NHS Trust. It seems likely that staff attitude and communication will be examined.
In this context, we welcome a consultation by NHS Improvement and the National Quality Board on safe staffing in maternity services.
Our response will make the point that safe staffing is not just about staff/patient ratios, shift patterns and skills and proficiency. All of these matter - but so does patient voice.
The consultation document refers to "Patient, carer and staff feedback" and lists seven different sources of patient feedback. It states that areas of concern highlighted by women and families must be carefully scrutinised. It does not, however, say who should carry out the scrutiny, or how.
Staff in maternity services work in busy environments that are physically and emotionally demanding. It is not reasonable to expect them to plough through multiple sources of patient feedback, trying to make sense of them. We have already made the point that patient feedback systems are cluttered, confused and hard to understand.
Ideally, maternity staff would turn to patient experience leads for help. Other evidence shows that hospital staff find it hard to act on patient feedback, and need "organisational readiness" - back-up from other parts of the system - to be able to use feedback to increase safety and drive improvement.
But patient experience leads are not always well supported, and lack parity with their clinical colleagues. NHS clinicians work in a culture that consciously develops their expertise. So they have access to comprehensive professional databases to guide their practice and professional development. Patient experience leads have a similar need for access to knowledge. And yet they are expected to resort to Google. That's not sensible, and it's not safe.
Safe practice depends on hearing the patent voice. And safe staffing depends on teamwork. Maternity staff cannot be experts in everything - they need help from "the team beyond the ward". That wider team includes patient experience leads. And they - like maternity staff - need to be better supported.
The consultation on safe, sustainable and productive staffing in maternity services is here.
Monday July 17th 2017
How reliable are filmed patient stories?
Are filmed patient stories a good thing? There seem to be more and more of them about, so they must be popular.
Perhaps that is because film-making is so much easier nowadays than it used to be. Filmed testimony can also be more compelling than a written report. And let's face it - in today's busy world, anyone who has a choice between a two-minute film clip and a twenty page report might well settle back and reach for the popcorn.
This report, however, sounds a note of caution. The authors note that:
- It can be assumed that patient testimony is particularly raw and honest. But narrative theorists see stories not so much as truth, but as the crafting of truth to propel and reshape meaning. Patients sometimes have agendas of their own.
- Some people are better able to articulate complex care experiences, or have greater "on screen" charisma than others. They can become more influential "stars" than other participants in patient films.
- The "talking head" format can appear to offer a direct and unmediated window into the experiences of patients. But the editing process necessarily fits talking heads within a structured narrative, directing thoughts in some ways, and limiting others.
The authors conclude that "there is something inherently fragile, or fluid, about patient narrative as a form of valid knowledge". Challenges include those listed above. But at the same time, patient film work can counter the "dumbing effects of questionnaires" and the "blindness to patients [caused by] heat maps and endless data collection".
This paper will offer plenty of food for thought for anyone involved in committing patient experience to film.
Tuesday July 11th 2017
GP Patient Survey results - should we be worried?
"...surveys are a valuable resource for monitoring national trends in quality of care [but] may be insufficient in themselves to fully capture patient feedback, and in practice GPs rarely used the results of surveys for quality improvement."
This observation, from "Improving patient experience in primary care" is worth considering alongside the results of the 2017 GP Patient Survey, newly published by NHS England.
The survey provides information on patients' overall experience of primary care services and their overall experience of accessing these services. The key findings contain plenty of good news - for example, that 85% of patients rate their overall experience of their GP surgery as good, and that 87% say the receptionists at their GP surgery are helpful.
The downside is that for every single key finding under "overall experience" and "access to in-hours services", patient experience has decreased since 2016. Sometimes it's not by much - 0.3% for "convenience of appointment" for example. Other decreases, however, are larger, and NHS England makes the point that "Given the size of the survey, even small changes in percentages are likely to be statistically significant".
Should we be worried? Well, yes - on two counts. Firstly because Sustainability and Transformation Plans, with their mantra of "care closer to home" will rely on primary care services to help keep the pressure off acute services. Any reduction in patient experience of primary care must be worrying for STP leaders.
The second cause for concern is that, as stated by the National Institute for Health Research, "While the GP Patient Survey data for any given practice is used as part of its CQC inspection record, there is no standard requirement for practices to review that data or act upon them. As a result there are wide variations in the use of the data and the value that can be derived from them".
So we know two things about the 2017 GP Patient Survey results. One is that there are statistically significant declines in patient experience since 2016. The other is that GPs don't have to do anything about it. That's not to say they won't. But at the whole system level, we have an NHS that seems content to gather patient experience data, while acknowledging that "there are wide variations in the use of the data and the value that can be derived from them".
All STPs make reference to "improved patient experience" as an outcome from the "whole system" transformations they propose. The GP Patient Survey indicates room for improvement within primary care - the absolute front line of public engagement with the health system. How will STP partnerships respond? We shall see...
Get the 2017 GP Patient Survey results here
Monday July 10th 2017
Patient voice is our canary in the coalmine. Let's make sure we can hear it.
We are all patients in the NHS. We know, from personal experience, what the difference is between good and bad patient experience.
So why, when the NHS as a whole tries to understand patient experience, does it make such a dog's dinner of it?
The NHS collects a mountain of evidence on patient experience, from sources including the NHS Friends and Family Test, Care Quality Commission patient surveys, the GP patient survey, local Healthwatch reports, and online feedback tools like NHS Choices star ratings. On top of that it piles further information from local questionnaire surveys, focus groups and public meetings. And on top of that are all the compliments and complaints that come directly from patients.
All these datasets present different information in different ways, so it is very difficult to collate them, or make meaningful comparisons. In addition, the quality of some of the data is questionable.
The NHS has plenty of data on patient experience. It's just that no-one can make sense of it all.
Plenty of studies have made exactly this point. A 2015 report entitled "Making Sense and Making Use of Patient Experience Data" had this quote from a patient experience lead: "We are data rich, but we don't bring it all together (national surveys scores and comments). It's a nightmare to see what's going on. Trying to triangulate between 12 different data sources coming from different angles, presented differently..."
Another report - the 2016 Carter Review - said "...hospitals and commissioners were often looking at different datasets and from different perspectives with inevitable disagreements."
Companies in the commercial world use customer experience as a driver for service improvement. They understand the value of feedback from the general public, and make sure that collection and analysis is clear and purposeful. It is hard to imagine a big corporate allowing its outlets to muddle through heaps of customer experience data gathered from dozens of incoherent sources.
Patient experience - like customer experience in the commercial world - can be understood. But understanding it depends on having a consistent analysis of evidence drawn from reliable sources.
We need to sort through our mountain of evidence on patient experience. We need to pick out a few reliable sources that have proven value in guiding policy and practice. Then we need to stick with them. If some sources are not very good, we need to be very brave, and say so. Then we need to stop using them.
In the NHS, the patient voice is the canary in the coalmine - the early warning system that can alert us to potential problems. We need to hear our canary. But we don't need to hear canaries, chaffinches, woodpigeons, crows - the whole darn woodland. Why not? Because that's just noise.
A 2015 report, "Beyond Metrics?" described the proliferation of patient voice measures as "adding more to the noise without amplifying the signal". And the problem with noise is that people can't make sense of it. So they stop listening - they screen it out.
In the coalmine you know that if you can hear the canary, you're safe. If you can't hear it, you know there's a risk - and then you can act. If you're not even listening, you don't know where you are. And then you're really in trouble, because you don't know what to do.
Tuesday July 4th 2017
Beware zombies and unicorns
"Lack of clarity on what PPI is (or might be) has given rise to a poorly monitored, complex field of activity..."
This statement is the opener to a paper described by its own authors as a "provocation". Their concern is that the investment of time and resources in much patient and public involvement (PPI) is taking a form of "busywork" - i.e. a time-consuming technocratic distraction.
They remark that Ironically, the notion of the usefully participating, evidence-engaged patient or citizen has become ubiquitous at the same time as ignorance and "bullshit" have been successfully harnessed as resources in "post-truth" politics".
The paper reviews the development of patient and public involvement in health research, and observes that "there is a lack of consensus about what effective PPI in research processes might look like and... little conclusive evidence about the best (or worst) ways to invoke PPI in research design, research practice, or research commissioning".
An underlying problem is that "Different models of PPI carry distinctive and sometimes contradictory assumptions about the types of public to be involved, the knowledge those publics might bring to bear, and their degree of involvement in decision-making processes."
Furthermore, people who step forward as patient/public representatives have varying motives for doing so. Some are "predominantly concerned with promoting and defending their own interests and values against other participants" while others "view themselves as interdependent members of a social collective and [are] oriented towards collective ends and the common good".
The authors conclude that "formal PPI can be seen as a ghastly composite of a zombie policy that continually pops up, offering (but never providing) a solution to purported deficits in democratic engagement, despite being useless in the last policy round, and a unicorn policy, a mythical beast, prevalent, and much discussed but never discovered in replicable form in any health-care system. This zombie/unicorn hybrid creates PPI as a form of busywork in which the politics of social movements are entirely displaced by technocratic discourses of managerialism".
If you're involved in PPI, don't be offended by this last paragraph! The paper may be, as the authors describe it, "a provocation", but it is well-founded, well argued, and raises important issues that deserve serious consideration.
Monday June 26th 2017
Why it's hard to act on patient feedback
"Patients are increasingly being asked for feedback about their healthcare experiences. However, healthcare staff often find it difficult to act on this feedback in order to make improvements to services."
So says a recently published study based on work with staff in three separate NHS Trusts.
The authors note that a growing international body of evidence suggests that patient experience, safety and clinical effectiveness are inextricably linked. But in spite of the wealth of feedback now available to healthcare services, there is little evidence that this has led to improvement in the quality of healthcare. "Simply providing hospitals with patient feedback does not automatically have a positive effect on quality standards".
Why is it that hospital staff find it difficult to translate patient experience into service improvement? The study points to three factors:
Normative legitimacy: To what extent are staff receptive to patient feedback? Is good patient experience seen as essential to safety and clinical effectiveness, or as a "nice but not necessary" add-on to clinical priorities?
Structural legitimacy: To what extent are staff teams (on a ward, say) empowered to identify and act on service improvement opportunities prompted by patient feedback?
Organisational readiness: Where staff teams need support for improvements from other parts of the hospital or the wider Trust, how ready are those other staff teams to pitch in and help?
The authors conclude that:
- Without the moral imperative to listen to the patient voice, improvement rarely takes place.
- Staff must have sufficient autonomy, ownership and resource in relation to a problem in order to enact change.
- Insufficient organisational readiness usually blocks action planning.
This is a must-read paper, full of analysis and insight that will strike a powerful chord with anyone who has worked at the front line of NHS patient feedback and quality improvement.
Thursday June 22nd 2017
When patients go unheard, people die.
"It is vital that the lessons, now plain to see, are learnt and acted upon, not least by other Trusts, which must not believe that 'it could not happen here'. If those lessons are not acted upon, we are destined sooner or later to add again to the roll of names.
The Report of the Morecambe Bay Investigation [into avoidable deaths]. Dr Bill Kirkup CBE, March 2015
"I had a meeting with a trust member and the analogy he used was that they were a bit like British Airways and it was like losing baggage. I really couldn't believe what the person was saying to me. It was harrowing.
Parent of a patient who died in the care of the Southern Health Trust. December 2015
We know why patient experience matters. It's because when patients go unheard, people die.
The best known example is the disaster at the Mid Staffordshire NHS Foundation Trust, where a series of unnecessary deaths led to the landmark Francis Inquiry. In his report, Sir Robert Francis was unequivocal about the reason for what he described as "appalling suffering" in the Stafford hospital. He said that it "was primarily caused by a serious failure on the part of a provider Trust Board. It did not listen sufficiently to its patients."
We think of Mid Staffs as a particularly low point in the history of the NHS. But it is not the only one.
Two years after Francis, the Kirkup inquiry revealed unnecessary deaths of mothers and babies in a maternity unit run by the Morecambe Bay NHS Trust. The inquiry report said that patients and relatives had encountered "defensive 'closed' responses, delayed replies, and provision of information that complainants did not find to be accurate."
Soon after that, the Mazars review into unexpected deaths at the Southern Health NHS Foundation Trust described "an ad hoc and inadequate approach to involving families and carers in investigations".
Different places, different providers, different services. But all joined by a common thread: a failure to value patient voice.
There is more. A review of unexpected deaths in a maternity unit run by the Pennine Acute Hospitals Trust said that "Staff attitude has been a feature of a significant number of incidents". A Parliamentary and Health Service Ombudsman report into the death of a three year old child in Devon said that "local NHS investigation processes were not fit for purpose and they excluded the family".
People sometimes think that "patient experience" means dealing with grumbles about appointments, car parking and hospital food. Or compiling Family and Friends Test reports, and wondering whether anyone will actually read them.
The nitty-gritty of patient experience may seem trivial. But the patient voice is the canary in the coalmine. It is an early warning system that can help managers to spot that all may not be well at the front line.
A patient-centred NHS will take every piece of patient feedback seriously. Because when patients go unheard, people die.
The Care Quality Commission is asking for people's views on "How can we assess how well providers review, investigate and learn from deaths?" The consultation is open until the 14th July 2017. Details here.
The Patient Experience Library's submission to the consultation can be seen here.
Thoughts? e-mail us: info@patientlibrary.net
Tuesday June 20th 2017
The state of patient experience - 2017
There are important differences between the American and British health systems. But that doesn't mean we can't learn from our US colleagues.
The Beryl Institute's "State of Patient Experience 2017" report is based on a survey of 1,644 healthcare organisations, both within and outside the US. It has some interesting findings that could be relevant to how patient experience work is carried out in the UK. Consider these points :
- Patient experience was seen as the top organisational priority, but employee engagement/satisfaction was second. There seems to be an understanding that happy staff equals happy patients.
- In US hospitals, investment in patient experience staff is growing year on year.
- In US hospitals, the leadership's desire for improved patient experience is just as much a driver for action as government-mandated measures. The top two supporting factors are "strong visible support from the top" and "formal PX structure or role". "Highly engaged staff" are seen as a further key factor in achieving positive patient experience.
As Sustainability and Transformation Partnerships start to pick up their momentum after the general election lull, those leading STPs would do well to bear the American learning in mind.
Almost all STPs mention "improved patient experience" as a desired outcome. Achieving that requires a systematic approach, with focused leadership, plus investment. In the detail underpinning STP planning, that needs to be stated.
Tuesday June 13th 2017
Patient/public involvement: Should money come into it?
Patient/public involvement: Should money come into it?
Across the UK health and care sector, many thousands of people are involved as patient/public representatives. As committee members, research participants, focus group contributors and survey respondents, they offer huge amounts of time and "expertise by experience" - nearly always as volunteers.
If patient and public input to the sector's learning and development has a value, should the value be recognised? Should our volunteer contributors become paid contributors?
Canada's Change Foundation has considered the issue. They recognise that payment for patient and public involvement (PPI) could undermine the ethos of volunteerism, or could engender a sense that opinions are being bought, rather than freely sought.
But they also consider the downside of volunteerism. This includes the possibility that expecting people to participate without payment could mean that low income patients are excluded from deliberation and debate. This matters in the context of health inequalities, where the most vulnerable in society are already relatively voiceless.
The authors state that they are "neither for nor against paying. Our concern is to work within the principles of fair, equitable and barrier-free public engagement". So they decide the payment issue on a case-by-case basis.
To help them do so, they have developed an easy-to-use decision tool. This sets the question of payments for PPI against parameters that guide decision makers towards a rational outcome.
By using the tool, you may or may not end up paying PPI participants. But at least you'll be able to explain how you have come to your decision
Tuesday June 6th 2017
Earth to Simon Stevens: Invest in patient experience
People involved in patient experience work can sometimes feel overwhelmed by the quantity and variety of reporting. There is a constant flow of feedback and reports from the CQC, Healthwatch, Friends and Family Test, Care Opinion, NHS Choices and more. Methods and approaches can change over time, making it hard to get a baseline for patient experience, or a sense of whether things are getting better or worse.
The Adult Inpatient Survey is a refreshing constant in the reporting landscape. The 2016 survey, just published, is the 14th of its kind, and so is able to offer insights into inpatient experience over the long term. The good news is that traditional patient bugbears - communication, cleanliness and hospital food - all show signs of improvement. Confidence and trust in clinical staff has also, encouragingly, gone up.
The spanner in the works comes from what the Picker Institute (which co-ordinated the survey) describes as "significant declines in key areas of person centred care".
Fewer patients feel involved in decisions about their care and treatment. Fewer report positive experiences of leaving hospital. And fewer believe they are getting enough help to recover and manage their condition. All this will come as a blow to an NHS that wants to help patients to be more active in self-managing their conditions.
Picker comments that "the results highlight a risk that improvements of the past could be lost if trusts and policy makers fail to keep the provision of high quality person centred care a top priority". We agree.
Publication of the report highlights two issues that are vital to a well-functioning NHS. The first is transparency. Publication of findings like these - consistently, and over many years - help us all to see what works, and what doesn't, from the patient's point of view.
The second is the value of patient experience work. Small investments in rigorous survey work can reveal insights (such as a possible threat to patients' ability to self-manage) that could cost the NHS very large sums of money.
The report has a clear message to Dept of Health policymakers: there are significant declines in key areas of person centred care. It also has a clear subtext: patient experience work offers valuable insight. And that is worth investing in.
Tuesday May 30th 2017
STPs versus public opinion - a divergence of views
NHS England's Five Year Forward View promises a "radical transformation of patient experience". But this report from the Health Foundation indicates that the general public expect their experience to get worse, not better.
According to polling by Ipsos Mori, 44% of people think the general standard of NHS care has worsened over the past year. And almost half (48%) think it will get worse over the next year.
Some people might argue that polling results of this kind are not worth having - that they are based on people's ill-informed opinions rather than rational and objective analysis of the state of care.
Our view is that public opinion is always worth having. We all use NHS services, and so do our nearest and dearest. We all have a pretty good idea of how good those services are. Top commercial brands know about the value of public opinion - however subjective it may be. They listen very carefully to what people think of their services.
Of course, corporates cross-check customer feedback against rational and objective evidence - for example, sales figures and financial returns. And this is where the NHS comes unstuck.
The Five Year Forward View is to be implemented through 44 Sustainability and Transformation Partnerships. Their published plans all mention improved patient experience. But few, if any, have set baselines for current levels of patient experience, or set targets for how and when patient experience will be improved.
The general public are pessimistic about improvements in care and patient experience. STPs are optimistic. It looks worryingly as though planners and strategists are out of touch with public opinion.
Sustainability and Transformation Partnerships need to put forward measures that show the general public that the promised "radical transformation of patient experience" is on its way. The alternative is to accept that, perhaps, the public may be right.
Tuesday May 23rd 2017
Patient and public involvement: Breaking organisational boundaries
"People tend not to care about organisational boundaries, but about how services can work better for them and their families." So says Helen Hirst, CEO of a group of Yorkshire CCGs, in NHS England's statutory guidance on public participation in commissioning.
She's right. But the same should apply to health professionals located within NHS organisations.
If we can only see as far as our own organisational boundaries, we'll never understand properly how services can work better for patients and communities. We need to see what has been tried elsewhere, and to learn from other organisations' successes - and failures.
The problem for patient engagement leads is that the learning is hard to track down. There is a wealth of knowledge on patient and public involvement, but it is scattered across hundreds of different websites - from Healthwatch, through various NHS bodies, to national charities and think tanks.
We have brought it all together in the Patient Experience Library because we don't think it's right that while clinicians have access to professional knowledge databases as a matter of course, PPI leads have to resort to Google.
We're delighted that the library is mentioned in NHS England's statutory guidance, and we're talking to the Dept of Health and others about how we can open up the library to NHS trusts and CCGs.
Tuesday May 16th 2017
Participation does not come naturally
Participation should be natural, says Rob Webster, Lead CEO for the West Yorks and Harrogate STP. His comment is the opener to NHS England's statutory guidance on patient and public participation in commissioning health and care.
We agree - sort of.
Participation should indeed be a natural part of NHS commissioning. But that doesn't mean that it comes naturally. In fact, it usually comes with lots of toil, sweat, and - sometimes - a few tears.
Patient and public participation is not easy. And that's why this excellent guide from NHS England is so welcome. At 32 pages, it is comprehensive. But it is broken down into clear sections, with lots of hyperlinks to take readers to further guidance and resources if they want.
The sections cover matters such as the policy and strategy context, participation frameworks and principles, and ten "key actions" for CCGs on how to embed involvement in their work.
We were delighted to see the Patient Experience Library mentioned as a useful resource, and there are plenty of other helpful pointers in the guidance as well.
Rob Webster is right - participation in NHS commissioning should be natural. This guide is an important help for people who are trying to make it so.
Tuesday May 2nd 2017
This is why insight matters
After Mid Staffs and the Francis Inquiry, you might think that lessons had been learned about treating statistics and performance indicators with caution. Francis was clear that "appalling suffering" and avoidable death at the Stafford Hospital occurred because the Board and management of the Trust spent too long looking at figures and not enough time listening to patients.
In spite of that, the view persists among some health professionals that quantitative data is "hard" data, and that patient stories are simply "anecdotal".
It is not unusual for patient voice champions such as Healthwatch to be challenged on the value of their report findings. A common question is about sample size and statistical validity. Sometimes, challenges of this kind are fair. Mostly, they completely miss the point.
This report, from Healthwatch Essex, takes key statements from a group of carers and turns them into poetry. The sample size was small. But the insights are profound.
There is nothing in this report that lends itself to "hard" statistical analysis. But if you want to know what it feels like to have to agonise over putting a loved one into a care home, read this report. It says more about patient and carer experience than a table of numbers ever could.
That is why insight matters.
Monday April 24th 2017
This is what compassion looks like
Every week, the Patient Experience Library trawls hundreds of websites, searching out new publications to add to the UK's collective evidence on patient experience.
We read thousands of reports every year. Most are good, some are excellent. This one, from Healthwatch Essex, is astonishing.
The work is based on a series of interviews with people who have had to arrange residential care for a loved one.
The interviews were transcribed and thematically analysed so as to draw out poems from people's experiences.
The result is powerful and moving testimony, describing the love, pain, guilt, sadness and loss that people feel when having to "put someone in a home".
There is much talk in health and care services about "person-centred care". Some of it can be convoluted, focusing on definitions and procedures. This report (perhaps we should call it an anthology) shows what caring for someone really means, and takes us deep into the experiences of people trying to do their best for loved ones who are moving beyond their reach.
A wonderful piece of work, displaying an innovative approach, and true compassion.
Tuesday April 18th 2017
(Still not) Learning from Mistakes
The Shrewsbury and Telford Hospitals (SaTH) NHS Trust has been in the news recently, following a series of avoidable deaths of babies.
Four years ago, the final report of the Francis Inquiry into the Mid Staffs disaster said this, "The suffering of the patients and those close to them ... requires a fully effective response and not merely expressions of regret, apology and promises of remedial action. They have already been at the receiving end of too many unfulfilled assurances".
Compare that statement with this, from one of the mothers whose baby died in the care of SaTH: "To hear that this (mistake) has happened before - it's just another blow. I've had an apology from the hospital, and assurances that this won't happen again. But other families have had those assurances and those apologies and if those were followed up, in the way that they said that they would, then I would have my daughter".
It would appear that Sir Robert Francis's warning about "unfulfilled assurances" has not been heeded.
In March 2015, the report of an investigation into avoidable deaths of mothers and babies at the Morecambe Bay NHS Foundation Trust said "It is vital that the lessons, now plain to see, are learnt and acted upon, not least by other Trusts, which must not believe that "it could not happen here". If those lessons are not acted upon, we are destined sooner or later to add again to the roll of names".
In June 2016, the Royal College of Obstetricians and Gynaecologists (RCOG) "Each Baby Counts" report looked at intrapartum and neo-natal deaths. It said "Many national reports have highlighted the fact that the same mistakes are made repeatedly, which suggests that our risk management processes may not be mitigating risk as we hope".
In July 2016, the PHSO's "Learning from Mistakes" report into the death of a three year old child said "local NHS investigation processes were not fit for purpose, they were not sufficiently independent, inquisitive, open or transparent, properly focused on learning, or able to span organisational and hierarchical barriers, and they excluded the family and junior staff in the process".
At Mid Staffs, Morecambe Bay and Shrewsbury and Telford, avoidable deaths occurred for different reasons. But a common thread running all the way through was a failure to hear from patients, and, in some cases, outright denial that patients had valid cause for concern.
A second thread was the failure to learn from mistakes. This includes a failure to treat patient feedback as a fundamental part of risk management. PALS teams and patient experience leads should be seen as an early warning system - the "canary in the coalmine" that can help NHS Trusts to spot that all may not be well on the wards.
We welcome Jeremy Hunt's call for an inquiry into the Shrewsbury and Telford deaths. But we worry that it will simply add to a growing pile of inquiry reports that all draw similar conclusions.
The NHS needs to start learning from its mistakes - particularly in respect of learning to listen to patients. Repeated "unfulfilled assurances" are a disaster, as are repeated "filed and forgotten" inquiry reports.
We have created the Patient Experience Library so that vital learning does not get dissipated and lost. We will be writing - once again - to Jeremy Hunt and Simon Stevens to call for more support for PALS teams and patient experience leads.
Tuesday April 11th 2017
Investing in patient experience: House of Lords weighs in
If you only have time to read one report this week - or even this month - read this one.
The House of Lords Select Committee's report on the Long-term Sustainability of the NHS is a breath of cross-party sanity, recognising issues and concerns that people in the NHS and care services have been talking about for years.
Among many forceful statements, we picked out this one: "We are concerned by the absence of any comprehensive national long-term strategy to secure the appropriately skilled, well-trained and committed workforce that the health and care system will need over the next 10-15 years."
"Workforce development" does not just mean clinicians. Fundamental to a patient-centred NHS are skilled, well-trained and committed patient experience leads. They can spearhead NHS England's goal of care that is "person-centred, coordinated, and tailored to the needs and preferences of the individual, their carer and family".
Last July, the PHSO's "Learning from Mistakes" report called for more support for PALS teams. We have done the same in Patient Experience Library reports including "What Price Patient Voice" and "Flying Blind?"
We are now looking at assembling these, and other evidence sources, to produce an investment case for PALS teams and patient experience leads. We'd like to know what you think. Please get in touch.